Jie Zhang, Zhong Jia* and Chao-Jun Kong
Department of Hepatopancreatobiliary Surgery, Hangzhou First People's Hospital, Nanjing Medical University Affiliated Hangzhou Hospital, Hangzhou Zhejiang, China
Corresponding Author:
Zhong Jia
Department of Hepatopancreatobililiary Surgery
Huansha Road No. 261, Hangzhou First People's Hospital
Nanjing Medical University Affiliated Hangzhou Hospital
Hangzhou, Zhejiang 310006, China
Tel: +86-13958114181
E-mail: jiazhong20058@hotmail. com
Received Date: August 30, 2017; Accepted Date: September 06, 2017; Published Date: September 14, 2017
Citation: Zhang J, Jia Z, Kong CJ (2017) Emergent Percutaneous Transhepatic Drainage for Superinfected Choledochal Cyst during Pregnancy. J Univer Surg. Vol. 5 No. 3:17 doi:10.21767/2254-6758.100085
Copyright: © 2017 Zhang J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Biliaryatresia; Choledochalcyst; Percutaneous trans-hepatic drainage; Pregnancy
Introduction
Congenital choledochal cysts are cystic dilations of the biliary tree varying in location from ampulla Vater to intrahepatic bile ducts. About 20% patients have no any discomforts (abdominal pain, jaundice, abdominal mass, etc) until adulthood. It seems to occur more frequently in females, presentation in pregnancy or the postpartum period is rare [1]. Obviously, infected choledochal cyst during pregnancy pose an increased risk to the pregnant woman and her developing fetus unless proper treatments have been adopted timely [2]. In general, some radiologic examinations are forbidden because of the presence of gravid uterus. Herein, we would like to report rare case of choledochal cyst combined serious infectious shock during pregnancy rescued by urgent interventional ultrasonography technique and discuss the management of this disease discovered during pregnancy.
Case Report
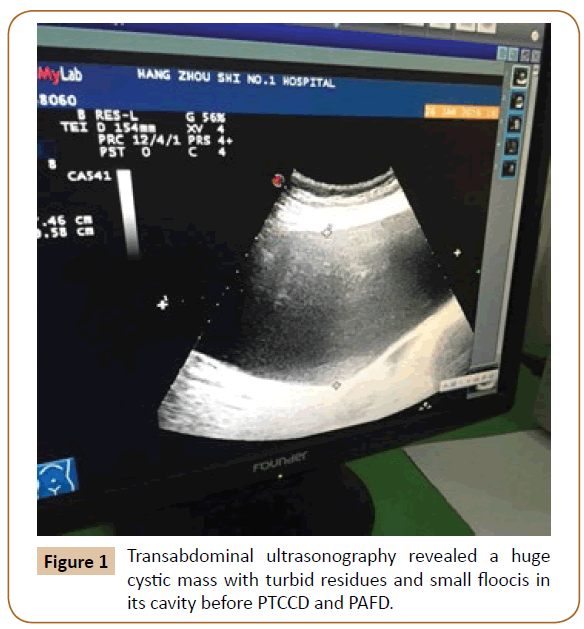
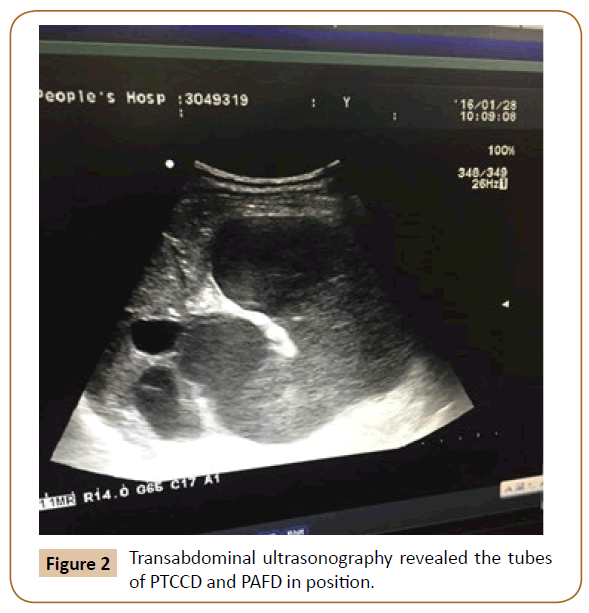
A 23-year-old primigravid woman at 18 weeks gestation presented with right upper quadrant abdominal pain, slight fever, and nausea of 10 days duration. The patient was not jaundiced. Abdominal palpitation confirmed a high-tension mass combined with tendness in epigastrium. Laboratory data including alanine transaminase (ALAT), aspartate transaminase (ASAT), alkaline phosphatase (AKP), serumbilirubin, and pancreatic enzymes were within normal limits. Serum albumin was very low up to 23 g/L and counts of leukocyte ascended up to 13. 8 × 109/L. Neukophil (neutrophil) contributed to 88. 3% and C-reactive protein was positive. Abdominal ultrasonography revealed a large cystic mass (12 cm × 18 cm) located between portal hepatis and pancreas, head, and floccis were found floating in the cystic luminal cavity, which was considered to be infected choledochal cyst. The patient was treated conservatively with antibiotic, bowel rest and surpertive therapy as usual. Unexpectedly, two days later, her upper abdominal pain became more severe than before, and her general condition developed worse. Blood pressure declined to 70/40 mmHg, Heart beat rate ascended to 153/min, temperature was 39. 5°C Re-abdominal palpitation disclosed a huge mass with tendness, rebound pain and regard muscle. The size of choledochal cyst increased to 18 cm × 25 cm (Figure 1). The levels of serum bilirubin, ALAT, and ASAT were elevated to 2. 4 mg/dL, 82 U/L, and 9 U/L, respectively. Thenekocyte, neutrophil, and C-reactive protein were elevated to 18. 3 × 109/L, 91%, 160 mg/ dL, respectively. The diagnosis of AOSC and sepsis were made. Ultrasound-guided PTCCD and percutaneous abdominal fluid drainage (PAFD) were in turn performed urgently. There was about 1900 ml dark brown turbid fluid and 200 ml mild yellow half-transparent fluid drained out from PTCCD tube, PAFD tube respectively in 10 minutes. The symptoms and physical signs of abdominal pain were improved immediately. Amazingly, about 3050 ml fluid was drained from PTCCD tube in first 24 hours. Thereafter, the dilation of cyst diminished. (Figure 2) Infection of cyst was also controlled in next 3 days. Laboratory data except serum albumin recovered to normal range finally. She was followed-up periodically by ultrasonography and her post treatment course was uneventfully until term pregnancy.
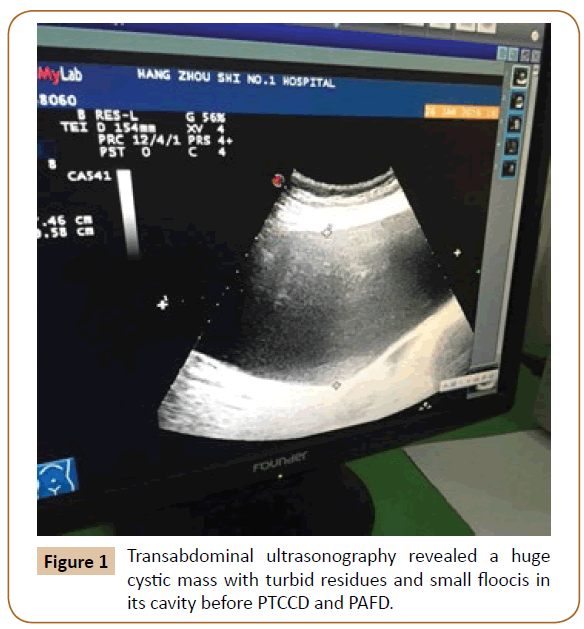
Figure 1: Transabdominal ultrasonography revealed a huge cystic mass with turbid residues and small floocis in its cavity before PTCCD and PAFD.
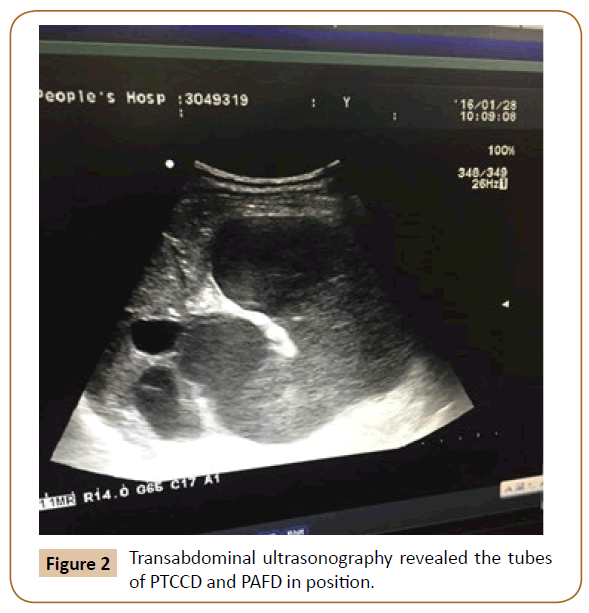
Figure 2: Transabdominal ultrasonography revealed the tubes of PTCCD and PAFD in position.
However, the pregnant woman’s nutrition was not so good to support the development of fetus. She had to cesarean section and included labour at 20 weeks of gestation. At 8 weeks postpartum, the patient underwent surgical excision of the choledochal cyst, cholecystectomy, and formation of a Rouxen- Y hepaticojejunostomy. Pathologic examination revealed typical features of choledochal cyst and chronic cholecystitis. The patient’s postoperative course was uncomplicated, and she is now healthy 10 months after surgery.
Discussion
Choledochal cyst consist of five forms according to anatomic location. Type I represents cystic dilation of common bile duct and accounts for 90% of all cases. It seems to be more likely first initiative presentation with sudden onset during pregnancy. The degree of cystic dilation is often greater than is usually described in non-pregnant cases. The definite etiology remains unclear. It is believable that enlarging pregnant uterus may cause biliary outflow obstruction [3]. In addition,pretrogen may also have a negative effect on muscle-tension of cystic wall and induce further dilation.
Many complications (spontaneous rupture of cyst, AOSC, pancretitis, biliaryperitonitis, sepsis, etc) may lead to fatal consequence or preterm labor. Majority of these cases were managed conservatively, and delivered by selective ceasarean section. Only minor cases had to suffer emergent surgery.
However, up to date, effective management strategies for pregnant women with choledochal cysts have not been well done according to previous reports, which may be associated with risk of maternal or fetal mortality and morbidity [4,5]. Cyst excision during pregnancy has generally been avoided because of the significant risk to the mother and fetus. Asymptomatic cysts during pregnancy don't desert worrisome. Any symptomatic cyst or rapidly enlarging cyst should be treated immediately as follows. A) Antepar tum cyst T-tube drainage by laparotomy has been reported, but it is not easy accepted by pregnant woman or her relatives [6]. So, if possible, nonsurgical management should be performed until the second trimester or postpartum, when the surgical risk is lowest. B) Antepartum ultrasound-guided percutaneous cyst drainage seems to be miniinvasive. But it is likely to result in bile juice leakage due to directly puncture. Furthermore, long-term management becomes a big problem after cyst decompression it's difficult to remain a stable position accordingly when the size of cyst is changed. C) Endoscopic techniques (endoscopic retrograde cholangiopancreatography and endoscopic nasobiliary drainage) allows the pregnant women with choledochal cysts in hope according recent European practical guideline if the fetus gets adequent protection from potential radiological damage during procedures. However, the stricture of cyst lowest-end makes a big challenge to do so. D) A wise procedure in this case are PTCCD and PAFD, which may increase the likelihood of successful outcomes for the mother and fetus. It is not a temporizing measure, but a persistent cathter drainage compared to previous report [4]. The least invasive procedure not only could benefit the mother the most while keeping the fetus in a natural environment of healthy intrautering growth, but also could provide a good preoperative condition until the definite surgery.
Based on our experience, full-term management of PTCCD and PAFD is safe, accessible and convenient during peripartum or perioperation. Many previous controversial points (such as the mode of delivery, the risk of spontaneous rupture during labor) are no longer a primary concern because the long-term placement of drainage tubes in this case could ensure cyst decompression in a persistent stage. Therefore, intensively nursing for drainage tubes is of crucial importance. If necessary, the other treatments including effective antibiotics, total parenteral nutrition support, and correction of electrocyte dysfunction should also be recommended. Of note, the drainage tubes may be accidently obstructed by turbid bile juice or small floocis, 10-15 ml natri chloride solution rapidly irrigated into drainage tube (2-3 times a day) could resolve the dilemma. The time for definitive surgery is addressed at 2-3 months later after partum. Otherwise, potential adhesion to the adjacent tissues of cyst will raise the difficulty of surgery. Generally, the drainage tubes will be placed until no surgery-related complications found 7-10 days later after definitive surgery.
Conclusions
The valuable use of ultrasound-guided double cathers drainage in our practice will minimise the risk of the pregnant women the most through infection control, depressure of cyst, and liver function improvement. The immediate procedure will also offer a better preoperative condition for further surgery. So, the use of this improved procedure as a pre-operative management or a rescue measure for choledochal cyst with associated biliary atresia during pregnancy has not been reported in the literature. We believe that if it is skillfully performed, there is only a minimal risk of the procedure-related complications.
Conflict of Interest
All authors declare that they have no conflicts of interests concerning on the paper.
20227
References
- Stain S, Guthrie CR, Yellin AE, Donovan AJ (1995) Choledochal cyst in the adult. Ann Surg 222: 128-133.
- Angel JL, Knuppel RA, Trabin J (1985) Choledochal cyst complicating a twin gestation. South Med J 78: 463-466.
- Taylor TV, Brigg JK, Russell JG(1977) Choledochal cyst of pregnancy. J R Coll Surg Edinb 22: 424-427.
- Nasu K, Matsuki S, Kawano Y,Miyakawa I, Nakashima K, et al. (2004) Choledochal cyst diagnose and conservatively treated during pregnancy. Am J of Perinatology 21: 463-468.
- Gulati MS, Srivastava DN, Paul SB, et al. (1999) Pre-operative management of congenital choledochal cyst with ultrasounded-guided percutaneous choledochalcystostomy. Australas Radiol 43: 514-516.
- SafioleasMC, Moulakakis KG, Misiakos EP (2005) Surgical management of choledochalcysts in adults. Hepatogastroenterology 52: 1030-1033.