Gyan Chand1*, SK Mishra1, Ashok Kumar2 and Suman Vimal1
1Department of Endocrine Surgery, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Rae Bareli Road, Lucknow, Uttar Pradesh, India
2Department of Genetics, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Rae Bareli Road, Lucknow, Uttar Pradesh, India
Corresponding Author:
Gyan Chand
Department of Endocrine Surgery
Sanjay Gandhi Post Graduate Institute of Medical Sciences
Rae Bareli Road, Lucknow, Uttar Pradesh 226014, India
Tel: 0522 266 8700
E-mail: drgyanchandpgi@gmail.com
Received Date: September 06, 2017; Accepted Date: September 09, 2017; Published Date: September 16, 2017
Citation: Chand G, Mishra SK, Kumar A, Vimal S (2017) Endoscopic Thyroidectomy: Experience of Breast and Axillary Approach. J Univer Surg. Vol. 5 No. 3:18 doi:10.21767/2254-6758.100086
Copyright: © 2017 Chand G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Endoscopic thyroidectomy; Thyroidectomy via axillary approach; Thyroidectomy via breast approach; Minimally invasive thyroid surgery
Introduction
Conventional open thyroidectomy remains the treatment of choice for benign and malignant thyroid tumors since ages, the open thyroid surgical procedures leaves a scar line in the lower anterior neck. This incision line sometimes may developed in to dark scars, hypertrophic scarsor keloid and may lead to parastheisa and hyperesthesia [1].
After the advancement in technology of laparoscopic and endoscopic surgery, thyroid and parathyroid surgery has been attempted using endoscopic approach. Since endoscopic parathyroidectomy and thyroidectomy were first introduced by Gagner and Huscher et al [2,3], various endoscopic thyroid surgery approaches have been devised, including direct cervical surgical approach (anterior or lateral cervical), extracervical access (chest wall, breast, or axilla) and a combination of approaches during last two decades [4-15].
Endoscopic thyroid surgical technique is still in early stage and it is almost establish in patients with benign thyroid nodules. After the surgical experience was accumulated, the application of endoscopic thyroidectomy was extended to patients with early thyroid cancer.
In this study we have reviewed our experience of endoscopic thyroid surgery through ipsilateral breast and axillary approach (IBAA). The purpose of this study is to evaluate the feasibility, safety and outcome of endoscopic thyroid surgery through this approach and to analyze the clinic-pathological features, duration and complications in our patients.
Methods
Between July 2013 to June 2016, 41 patients underwent 43 procedures of endoscopic thyroid surgery through ipsilateral breast and axillary approach at our department was included in this study. All procedures were performed by single surgeon and retrospectively analyzed.
All patients presented with visible goiter in the neck, routine preoperative diagnostic investigations were performed, including ultrasound neck, fine needle aspiration cytology and thyroid function test. All patients were explained about surgical procedure, possible complications and the possibility of conversion from endoscopic to open thyroidectomy. The informed consent was obtained from all the patients before surgical procedure. All patients were opted for endoscopic thyroid surgery.
Patients’ selection criteria
Inclusion criteria:
1. Motivated patients (committed to scar free neck)
2. Dominant thyroid nodule size <6cm in greatest diameter
3. Benign on thyroid cytology
4. Normal thyroid function test
5. Ability to understand the surgical options and provide informed consent
6. No previous neck surgery
Exclusion criteria:
1. Preoperative diagnosis of thyroid cancer
2. Presence of cervical lymph nodes
3. Big nodules and compression on trachea
4. Retrosternal extension
5. Previous neck and chest surgery
6. Abnormal thyroid function test
Surgical procedure
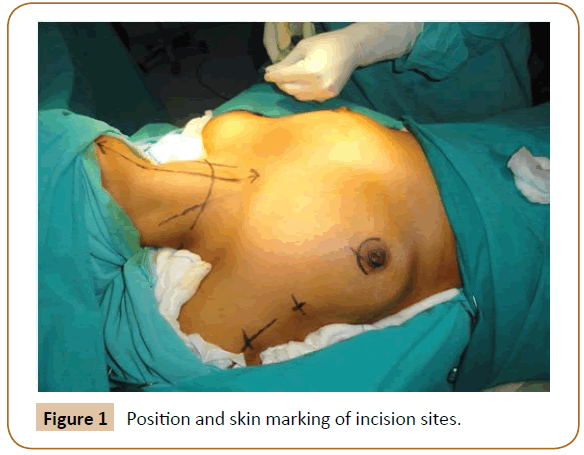
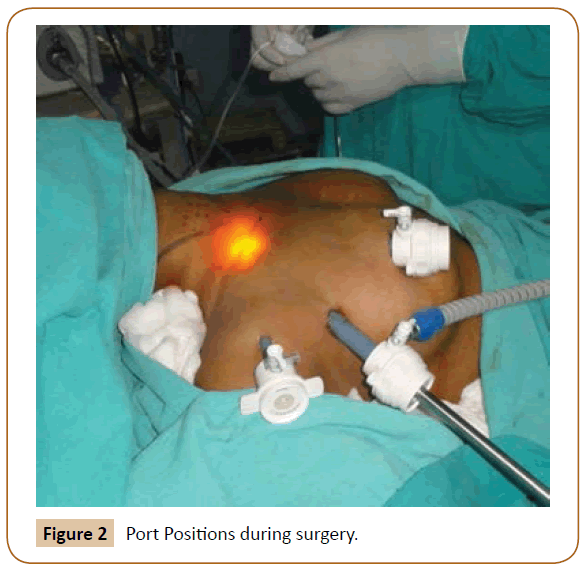
All patients were operated under general anesthesia with single lumen flexometallic endotracheal tubes. They were put on supine positions at 30 degree reverse trendelenburg position with sandbag under the shoulder. The ipsilateral arm was extended up to 90°-120°. Incision sites were marked. A diluted epinephrine solution (1:200000) was injected into the anterior chest wall and cervical area (Figure 1). Three incisions for ports were made; two were in axilla at anterior axillary line and one in superiormedial circumareolar site on ipsilateral breast. First 12mm port was inserted through axillary incision blindly towards the thyroid cartilage; withdraw it about half of its length, so a blind space was created into subcutaneous plane. It was connected with CO2 insufflations at 6 to 8mm Hg and thirty degree telescope was inserted. Another two ports were now placed directing to this tunnel and subcutaneous plane was created under vision with scissor connected with electro cautery (Figure 2).
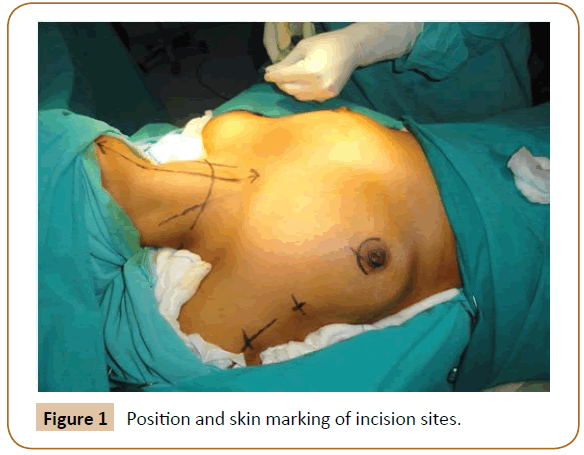
Figure 1: Position and skin marking of incision sites.
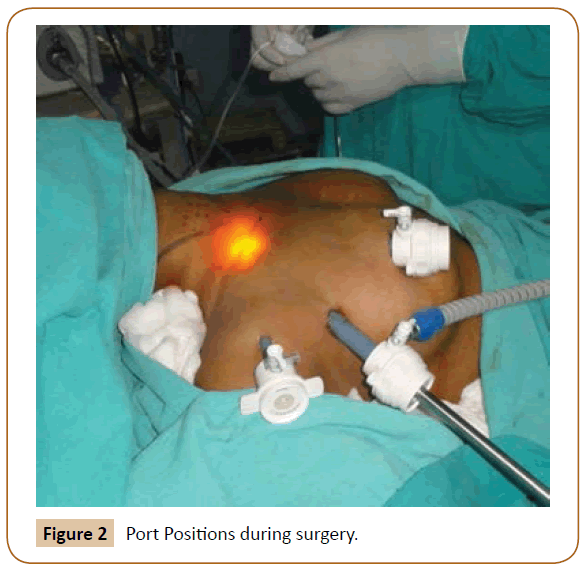
Figure 2: Port Positions during surgery.
Subplatysmal adequate working space was created from thyroid cartilage superiorly to sternal not chinferiorly then dissected the strep muscles from thyroid lobe from lateral side. The sternohyoid and sternothyroid muscles were dissected from each other than the upper end of sternothyroid muscle was resected using 5-mm ultrasonic vessel sealing device (SonoSurg: Olympus, Japan). The inferior pole of thyroid mobilized first by coagulation and cutting of inferior polar vessels. It was followed by lateral mobilization of thyroid lobe and carefully visualization and preservation of parathyroid glands and recurrent laryngeal nerve. Thyroid isthmus was then resected and in lastthe upper pole of thyroid lobe was dissected. Finally gland put into endobag and delivered through axillary port incision and closed the wound with negative pressure drain in situ.
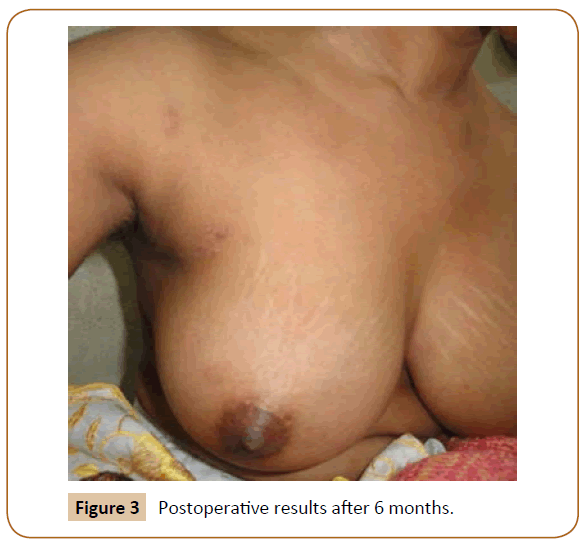
The extent of surgery, size of gland, weight of gland and duration of surgery was recorded. Post-operative care was same as conventional open thyroid surgery. The hypocalcaemia, voice change, hemorrhage and hospital stay was noted. We checked the serum ionized calcium on first postoperative day morning and we define the postoperative hypocalcaemia as serum ionized calcium levels <4.6mg/dl (ranges from 4.6-5.3mg/dl), with or without clinical symptoms of hypocalcaemia or positive Trousseau’s sign with subnormal serum ionized calcium levels (4.6-5.3mg/dl). During follow-up final histopathology and cosmetic outcome was evaluated (Figure 3).
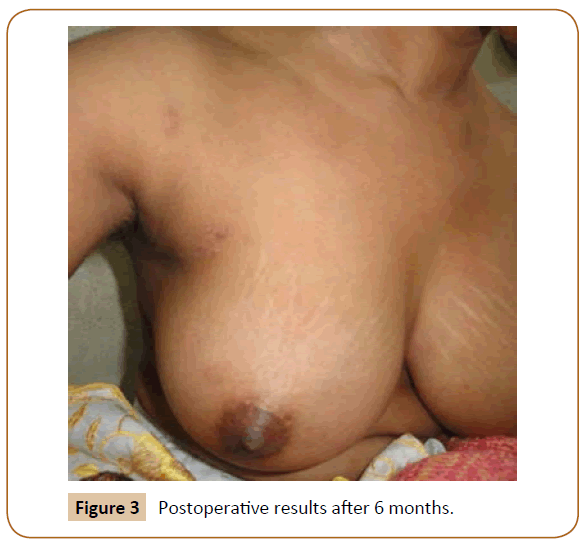
Figure 3: Postoperative results after 6 months.
Results
Between July 2013 to June 2016, total 41 patients were operated endoscopically using ipsilateral breast and axillary approach, two patients were operated twice for completion total thyroidectomy endoscopically. The clino-pathological characteristics are described in Table 1. Mean duration of goiter was 2.2 years (range 1 month to 8 years). On thyroid function test all were euthyroid. 37 patients were operated successfully endoscopically however four patients were converted to open surgery due to intractable bleeding from the thyroid surface and from the upper pole. No frozen biopsy was send during surgery however two patients underwent completion total thyroidectomy endoscopically after the final histopathology turns out to follicular thyroid carcinoma. Three patients diagnosed as papillary thyroid carcinoma on final histopathology was underwent completion total thyroidectomy and central neck dissection by conventional open techniques. The mean duration of surgery for hemithyroidectomy was 139.24 minutes and for total thyroidectomy was 243.33 minutes. In Hemithyroidectomy groups the mean tumor size was 4.21cm, the mean tumor weight was 17.15gm, and the mean hospital stay was 2.49 days (range 1 to 7 days).
| Clinico-pathological characteristics |
Value (N=41) |
| Age (Years) |
32.85 (range, 16-70) |
Gender
Male
Female |
7
32 |
Tumor size
Upto 3cm
>3-4cm
>4-5cm
>5-6cm |
05
13
14
10 |
Preoperative FNAC diagnosis
Colloid nodule
Follicular lesion
Hurthle cell lesions |
33(80.5%)
5(12.2%)
3(7.3%) |
Final Histopathological diagnosis
Colloid nodule
Follicular adenoma
Hurthle cell adenoma
Thyroiditis
Carcinoma
FVPTC
TCVPTC
WIFTC
MIFTC |
26 (63.41%)
07(17.07%)
01(2.44%)
02(4.88%)
05(12.20%)
02(4.88%)
0192.44%)
01(2.44%)
01(2.44%) |
Surgical procedure
Hemi thyroidectomy
Total thyroidectomy
Completion total thyroidectomy
Converted to Open |
34(79.16%)
3(6.98%)
2(4.65%)
4(9.30%) |
Table 1 Clinico-pathological characteristics.
The postoperative complications includes temporary voice change noticed in two hemi thyroidectomy patients however temporary hypocalcaemia was noticed on postoperative day two, in two patients who underwent endoscopic total thyroidectomy, managed with oral calcium. One patient underwent endoscopic completion total thyroidectomy and two patients which were converted to open, developed temporary postoperative biochemical hypocalcaemia and they were managed with oral calcium.
The post-operative pain was relived on 1st to 3rd days after surgery and mean duration of drain was 3-4 days after surgery. The sarcoma was noticed in the neck in few cases. On followup visit from 04 month to 40 months, suggested that none had hypocalcaemia or recurrent nerve palsy. The patients have excellent cosmetic outcome in follow-up visits.
Discussion
The first endoscopic thyroid surgery for 5 to 7cm adenoma was performed by Oghami et al using three port technique, two in circumareolar and one in parasternal position 10, In this technique there was a scar in anterior chest wall and then Ikeda et al. applied chest and axillary approach for thyroid adenoma, Grave’s disease, and papillary micro carcinoma [10,13]. Shimazu et al modified this approach to axillary- bilateral breast approach for endoscopic thyroidectomy [16]. Endoscopic thyroid surgery has generally been thought to be appropriate for benign thyroid disease, although endoscopic thyroid surgery is also feasible for Grave’s disease and well-differentiated thyroid carcinoma in some selected patients [17-19].
Present study composed of endoscopic thyroid surgery for clinically euthyroid benign goiters, out of 41 patients, majority have solitary thyroid nodule. The basic principle of thyroid surgery was same during this technique of endoscopic surgery, such as capsular dissection, identification and preservation of parathyroidand recurrent laryngeal nerves so the operation can be performed safely. This study showed that endoscopic thyroidectomy via breast and axillary approach has learning curve. The majority of patients were young (20-30 years of age), and they reported thyroid nodule early (33% reported within six months duration) and more than 50% had <4cm thyroid nodule in size.
The complications rate in this technique was minimal such as five patients (11.63%) did experience transient hypocalcaemia and two patient (4.65%) experienced transient recurrent laryngeal nerve palsy however none of patient noticed permanent hypocalcaemia or recurrent laryngeal nerve palsy on subsequent follow-up visits. The cause of hypocalcaemia and recurrent laryngeal nerve palsy in these patients might be caused by lateral thermal spread by the ultrasonic coagulation devices [20].
The rate of conversion to open has been reported at 0-13% 21 the main reasons for conversion to open surgery are hemorrhage, difficult dissection, tumor size, thyroiditis and tracheal injury [21]. In present study, four patients were required conversion to open because of bleeding from surface of nodule and from the superior thyroid vessels.
Our endoscopic thyroidectomy approach has several potential weaknesses in terms of operative time, hospital stay and invasiveness. It should achieve the same result as conventional surgery with additional advantage of shorter hospital stay, less postoperative pain and excellent cosmetic results especially in young women. In current series the cosmetic result was excellent; however we required more extensive dissection to create working space therefore the dissection was not truly minimally invasive. Recently Wong et al. reported the chest wall approach did not differ significantly from conventional thyroid surgery inform of producing inflammatory markers like interlukin-6, tumor necrotic factor, C-reactive protein and cortisol, which indicate the degree of surgical damage [22].
Yeung et al concern about scar around the nipple, especially in western women [23]. Therefore surgeons from western countries favor endoscopic neck surgery through trans axillary approach, however trans axillary has several drawbacks including, lateral approach to thyroid, narrow working space, long scar in axilla and contralateral lobectomy requires ipsilateral approach [24]. In our series’ most of our patients were satisfied with their nipple scar.
There are chances of potential adverse effect due to carbon dioxide insufflation in surgical working space with some reports of subcutaneous emphysema [25]. However no adverse effect has been reported in our series with using carbon dioxide at low pressure (7 mm Hg) with high flow rate (7 L/min). This high flow helps us in maintain the working space during carbon dioxide gas loss, either due to frequent use of suction to clear smoky field produced by electric cauteryor when ports are not airtight fully.
In conclusion, endoscopic thyroidectomy by the breast and axillary approach in selected patients with benign thyroid disease is an effective procedure and allows excellent cosmetic results. This method is a valid option to the selected group of patients who do not want visible scar in the neck.
Conflict of interest
Authors have no conflict of interest.
Acknowledgments
No industry sponsorship of current work.
20376
References
- Lee D, Nam Y, Sung K (2010) Single incison endoscopic thyroidectomy by the axillary approach. J Laparoendosc Adv Surg Tech A 20: 839-842.
- Gagner M (1996) Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 83: 875.
- Huscher CS, Chiodini S, Napolitano C, Recher A (1997) Endoscopic right thyroid lobectomy. SurgEndosc11: 877.
- Gagner M, Inabnet BW III, Biertho L (2003) Endoscopic thyroidectomy for solitary nodules. Ann Chir 128: 696-701.
- Cougard P, Osmak L, Esquis P, Ognois P (2005) Endoscopic thyroidectomy. A preliminary report including 40 patients.Ann Chir 130: 81-85.
- Inabent WB III, Jacob BP, Gagner M (2003) Minimally invasive endoscopic thyroidectomy by a cervical approach. Surg Endosc 17: 1808-1811.
- Henry JF, Sebag F (2006) Lateral endoscopic approach for thyroid and parathyroid surgery. Ann Chir 131: 51-56.
- Shimizu K, Akira S, Tanaka S (1998) Video assisted Neck surgery: endoscopic resection of benign thyroid tumor aiming at scarless surgery of the neck. J SurgOncol 69: 179-180.
- Shimizu K, Akira S, Jasmi AY, Kitamura Y, Kitagawa W, et al. (1999) Video assisted neck surgery: endoscopic resection of thyroid tumor with very minimal neck wound. J Am CollSurg 188: 697-703.
- Oghami M, Ishii S, Arisawa Y, Ohmori T, Noga K, et al. (2000) Scarless Endoscopic Thyroidectomy: breast approach for better cosmoses. SurgLaparoscEndosPercutan Tech 10: 1-4.
- Park YL, Han WK, Bae WG (2003) 100 cases of endoscopic thyroidectomy: breast approach. SurgLaparoscEndosPercutan Tech13: 20-25.
- Saski A, Nakajima J, Ikeda K, Otsuka K, Koeda(2008) Endoscopic thyroidectomy by the breast approach: a single institution’s 9-year experience. World L Surg 32: 381-385.
- Ikeda Y, Takami H, Sasaki Y, Kan S, Niimi M (2000) Endoscopic neck surgery by the axillary approach. J Am Surg 191: 336-340.
- Benhidjeb T, Anders S, Berlehner E (2006) Total video-endoscopic thyroidectomy via axillo-bilateral breast approach (ABBA). Langenbecks Arch Surg 391: 48-49.
- Cho JH, Kim SW, Chung KW, Park KS, Han W, et al. (2007) Endoscopic thyroidectomy using a new bilateral axillo breast approach. World J Surg 31: 601-606.
- Shimazu K, Shiba E, Tamaki Y,Takiguchi S, Taniguchi E, et al. (2003) Endoscopic thyroid surgery through the axillo-bilateral breast approach. Surg Laparosc Endosc Percutan Tech 13:196-201.
- Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, et al. (2007) Endoscopic thyroidectomy fot thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg 31: 2302-2306.
- Li ZY, Wang P, Wang Y, Xu SM, Cao LP, et al. (2010) Endoscopic thyroidectomy via breast approach for patients with grave’s disease. World J Surg 34: 2228-2232.
- Bellantone R, Lombardi CP, Raffaelli M, Crea CD, Oragano L, et al. (2003) Video assisted thyroidectomy for papillary thyroid carcinoma. Surg Endosc 17: 1604-1608.
- Yamamoto M, Sasaki A, Asahi H, Shimada Y, Sato N, et al. (2001) Endoscopic subtotal thyroidectomy for patients with Grave’s disease. Surg Today 31: 1-4.
- Miccoli P, Minuto MN, Ugolini C, Pisano R, Fosso A, et al. (2008) Minimally invasive video assisted thyroidectomy for benign thyroid disease: an evidence-based review. World J Surg 32: 1333-1340.
- Wong M, Zhang T, Mao Z, Dong F, Li J, et al. (2009) Effect of endoscopic thyroidectomy via anterior chest wall approach on treatment of benign thyroid tumors. J LaparoendoscAdvSurg Tech A19: 149-152.
- Yung GH (2002) Endoscopic thyroid surgery today: a delivery of surgical strategies. Thyroid 12: 703-706.
- Lee KE, Kim HY, Park WS, Choe JH, Kwon MR, et al (2009) Postauricular and axillary approach endoscopic neck surgery: a new technique. World J Surg 33: 767-772.
- Gottlieb A, Sprung J, Zheng XM, Gagner M (1997) Massive subcutaneous emphysema and sever hypercarbia in a patient during endoscopic trancervicalparathyroidectomy using carbon dioxide insufflation. AnesthAnalg 84: 1154-1156.