D Blez1, G Leroux2, M Merlant2, P Cacoub2, Laurent Chiche3, E Caumes1 and S Jauréguiberry1*
1Department of Infectious Diseases and Tropical Medicine, Pitié Salpêtrière Hospital, 47-83 Bvd of the Hospital, APHP, Paris, France
2Department of Internal Medicine and Clinical Immunology, Pitié Salpêtrière Hospital, 47-83 Bvd Hospital, APHP, Paris, France
3Department of Vascular Surgery, Pitié Salpêtrière Hospital, 47-83 Bvd Hospital, APHP, Paris, France
Corresponding Author:
Stéphane Jaureguiberry
Department of Infectious Diseases and Tropical Medicine
Pitié-Salpêtrière Hospital
Paris, France
Tel: +33142160393
Fax: +33142160445
E-mail: stephane.jaureguiberry@aphp.fr
Received date: November 11, 2017; Accepted date: November 20, 2017; Published date: November 22, 2017
Citation: Blez D, Leroux G, Merlant M, Cacoub P, Chiche l, et al. (2017) Endovascular Chronic Q Fever with Contiguous Psoas Abscess and Spondylitis. Arch Med Vol No:9 Iss No:6:3
Copyright: © 2017 Blez D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Q Fever; Spondylitis; Aortic aneurysm; Abdominal CT; Abscess
Introduction
Vascular chronic Q fever (CQF) is a severe form of Q fever, a ubiquitous zoonosis, with non-specific symptoms, challenging diagnosis and that can lead to several complications associated with a poor prognosis. We present here the case of a rare form of endovascular CQF in whom the treatment could have been started earlier if the diagnosis had been evoked in a systematic way.
Case Report
In August 2016 a 68-year-old man was hospitalized for weight loss (15 kilograms in 6 months), fatigue and pygalgia radiating to the left lower limb, lasting for two months despite three lumbar corticosteroid infiltrations and 2 short antibiotic courses with amoxicillin-clavulanic acid for seven days. He had a history of coronary stenting, high blood pressure, occlusive arteriopathy of the lower limbs and a 40 millimeter diameter infrarenal aneurysm diagnosed by ultrasound in 2007 and monitored every year. He did not report any contact with farm animals, but often stay Southern France.
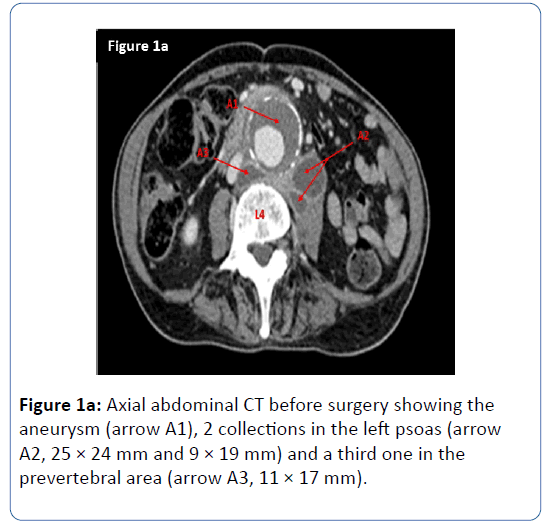
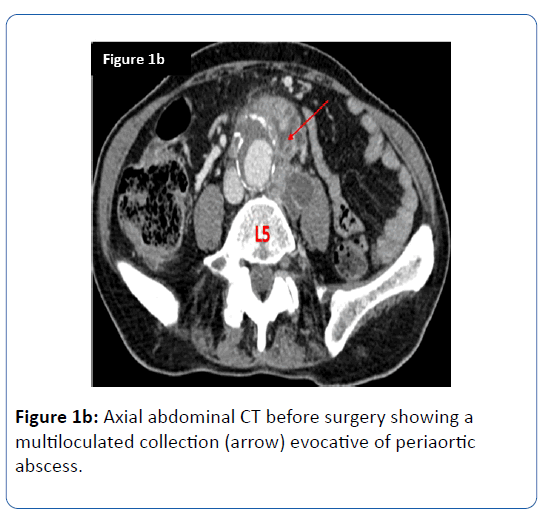
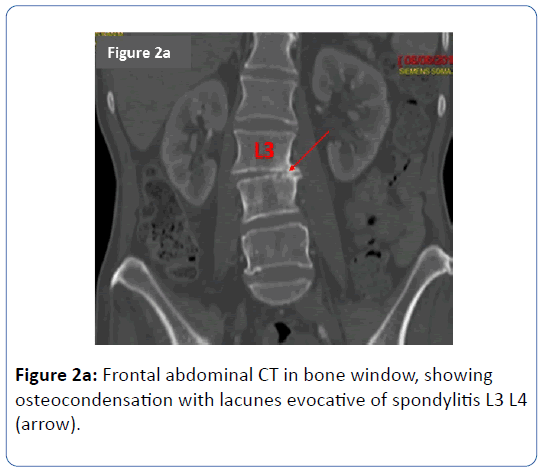
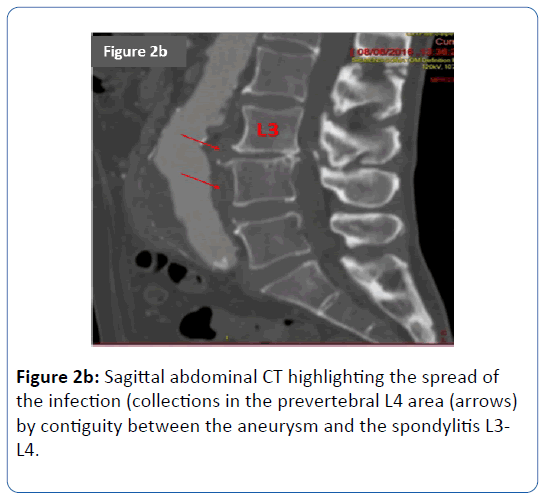
He experienced symptoms evocative of spontaneously healed pneumonia in 2013 without any medical documentation and a resolving pneumonia in 1970 treated with anti-tuberculous therapy without bacteriologic evidence. Physical examination revealed apyrexia, a cardiac systolic aortic murmur, arterial blood pressure was 109/77 mmHg, heart rate was 73 per minute, abdominal aortic murmur. Leucocytes blood count was 12370/mm3 (normal range, 4000-12000/mm3), C-reactive protein was 44 mg/L (normal value, <5 mg/L), creatinine was 57 micromol/L, liver enzyme levels and creatin-phosphokinase were normal. Thoracoabdominal computed tomography (CT) revealed a perianeurysmal collection, an abscess in the left psoas and signs of L3 L4 spondylitis (Figures 1 and 2).
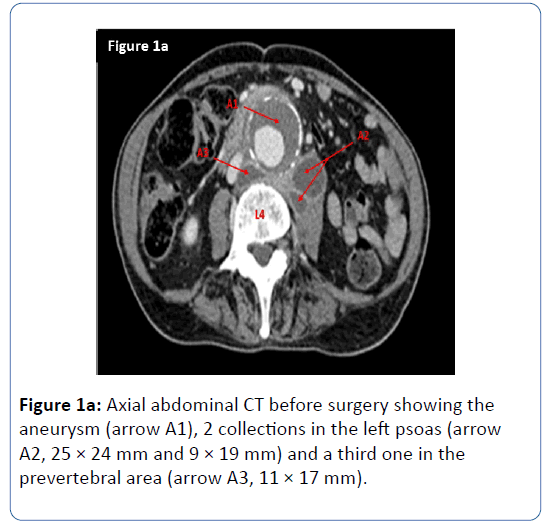
Figure 1a: Axial abdominal CT before surgery showing the aneurysm (arrow A1), 2 collections in the left psoas (arrow A2, 25 × 24 mm and 9 × 19 mm) and a third one in the prevertebral area (arrow A3, 11 × 17 mm).
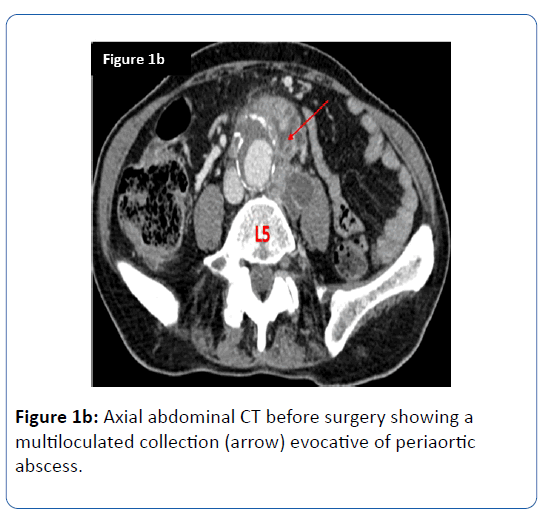
Figure 1b: Axial abdominal CT before surgery showing a multiloculated collection (arrow) evocative of periaortic abscess.
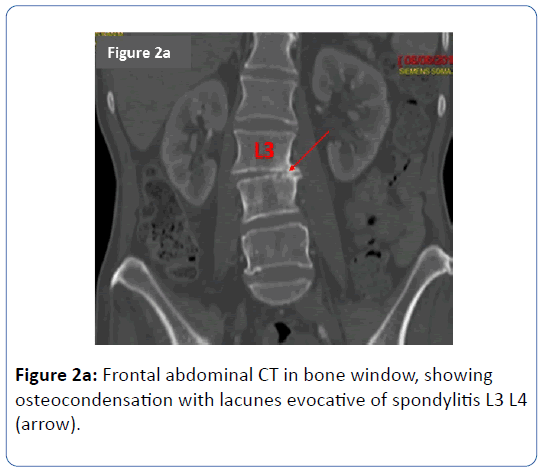
Figure 2a: Frontal abdominal CT in bone window, showing osteocondensation with lacunes evocative of spondylitis L3 L4 (arrow).
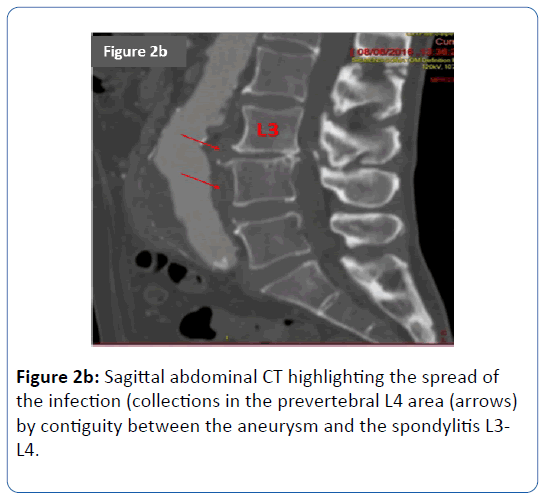
Figure 2b: Sagittal abdominal CT highlighting the spread of the infection (collections in the prevertebral L4 area (arrows) by contiguity between the aneurysm and the spondylitis L3- L4.
The 2-deoxy-2-[18F]fluoro-D-glucose positron emission tomography/computed tomography (18F-FDG PET/CT) showed hypermetabolism of these lesions without remote infectious focus. There was no vegetation seen in a trans-thoracic and trans-esophageal ultrasound. CT-guided puncture of the periaortic collection found purulent fluid, but the gram stain and cultures remained sterile for bacteria and mycobacteria. Infected vascular tissues were surgically removed and he benefited from the implementation of an axillobifemoral bypass. An antibiotic course with piperacillin-tazobactam, vancomycin and amikacin was started from the day of the surgery. Seven days after the surgery but six months after the appearance of symptoms Q fever serology performed at National Reference Center (Marseille, France) was positive with an indirect immunofluorescent antibody (IFA) for the anti-phase I antibody (IgG 1:12800, IgM negative and phase II antibody (IgG 1:1600, IgM negative) supporting the diagnosis of endovascular chronic Q fever with contiguous psoas abscess and spondylitis (herein 2 major diagnosis criteria using expert review criteria [1]), as PCR and culture of Coxiella burnetii were not performed. Legionella serology was also positive at low titers (1/16), whereas serologies for rickettsiosis, bartonellosis and brucellosis were negative.
Tuberculosis was ruled out as the acid fast bacilli staining (auramine) and the 90 days’ time culture (Lowenstein) were negative. There was no anatomopathologic evaluation of the surgically removed tissue but no clinical elements for inflammatory large blood vessel diseases in the past history of the patient were retrieved. Antibiotics were changed for doxycycline 100 mg twice a day and hydroxychloroquine 600 mg per day. After three months of such treatment, the antibody titers remain stable. Unfortunately, the clinical course was complicated by various hospitalized acquired infections and medical hazard leading to the death of the patient in October 2016.
Discussion
This case illustrates an unusual form of severe vascular CQF associated with iliopsoas abscess and spondylitis, revealed by persistent lumbar pain with radiation to the left lower limb. The literature about this form of CQF is poor. Indeed, in a review of the literature Galy et al. [2] reported 7 cases of endovascular chronic Q fever associated with iliopsoas abscess without endocarditis (14 cases if the endocarditis was not excluded), of which 4/7 and 8/14 respectively had spondylitis. When the endocarditis was ruled out, the spread of the infection seemed to be by contiguity. After the Q fever endocarditis, endovascular infection is the second most frequent form of CQF that almost always complicates a preexisting aortic aneurysm or aortic allograft [3] and is associated with a poor prognosis (18.2 to 23.7% mortality rate despite an optimal treatment) [4]. CQF treatment consists in at least 18 months of tetracycline and hydroxychloroquine regimen [5] with better outcome when surgical management can be performed, in case of vascular infection [4]. In our case diagnosis was suspected almost 6 months after the beginning of the disease and was belatedly mentioned. This form of CQF needs to be kept in mind face to septic aneurysm without clear diagnosis.
Diagnosis of CQF is also matter of concern. In our patient, Legionella serology was positive, at low titers, which resulted from a cross-reaction between Legionella and Coxiella burnetii serology, as described in previous report [6]. CQF is usually associated with high titers of Immunoglobulin G against phase I antigen of Coxiella burnetii (IgG1), that can also be elevated in case of recent acute Q fever (in which a serological control is needed to see the decrease in antibody titers), the positive predictive value increase with the titer (37% for 1:800; 75% for 1:6400 cut-off) as discussed by Raoult et al. [1]. Polymerase chain reaction (PCR) in blood, pus or tissue may also help the diagnosis. Thus, diagnosis of CQF is based upon a score with microbiological, serological and imaging criteria, which allows classifying a case as definite or possible diagnosis of CQF [6].
Usually, organisms suspected to be involved in spondylitis or iliopsoas abscesses are Staphylococcus aureus, Streptococcus spp., Mycobacterium tuberculosis (when the origin is skeletal infection) and Escherichia coli (when the origin is the urinary tract or the bowel [7]). During septic aortic aneurysm [8], Salmonella spp., Staphylococcus aureus and Streptococcus spp., but also Campylobacter fetus, Listeria monocytogenes, Mycobacterium tuberculosis, Aspergillus spp., and Brucella spp. could be involved. In our patient, all of these pathogens had been excluded by microscopic examination, culture and serological testings. In a study of 26 patients treated for septic aneurysm, Coxiella burnetii was isolated in one case [8], and in 2 of 25 patients with septic aortic aneurysms in another study [9]. To our knowledge no guidelines exists asking for a mandatory research for Q fever. Serology has to be done facing a negative result for all other research [8]. Coxiella burnetii seems to be rare in septic aneurysm and ask for a systematic research to avoid delay for appropriate treatment that negatively impacts on global outcome as our patient.
Conclusion
Although rare this case highlights the severity of the disease with high mortality rate. This case asks for an earlier serological and PCR testing for Q fever in case of septic aneurysms to avoid delayed diagnosis. Systematic research need to be discussed regarding the rarity of this infection among all septic aneurysms. More studies are needed to evaluate the cost-effectiveness of this strategy.
21424
References
- Raoult D (2012) Chronic Q fever: Expert opinion versus literature analysis and consensus. J Infect 65: 102-108.
- Galy A, Decousser J, El-Anbassi S, Nebbad B, Belzunce C, et al. (2016) Psoas abscess and chronic Q fever: A contiguous or hematogenous complication? A case report and literature review. Infect Dis 48: 626-631.
- Raoult D, Marrie T, Mege J (2005) Natural history and pathophysiology of Q fever. Lancet Infect Dis 5: 219-226.
- Eldin C, Mailhe M, Lions C, Carrieri P, Safi H, et al. (2016) Treatment and prophylactic strategy for Coxiella burnetii infection of aneurysms and vascular grafts. Medicine 95: e2810.
- Raoult D, Houpikian P, Dupont H, Riss J, Arditi-Djiane J, et al. (1999) Treatment of Q fever endocarditis. Arch Intern Med 159: 167.
- Musso D, Raoult D (1997) Serological cross-reactions between Coxiella burnetii and Legionella micdadei. Clin Diagn Lab Immunol 4: 208-212.
- López V, Ramos J, Meseguer V, Pérez Arellano J, Serrano R, et al. (2009) Microbiology and outcome of Iliopsoas abscess in 124 patients. Medicine 88: 120-130.
- Brossier J, Lesprit P, Marzelle J, Allaire E, Becquemin J, et al. (2010) New bacteriological patterns in primary infected aorto-iliac aneurysms: A single-centre experience. Eur J Vasc Endovasc Surg 40: 582-588.
- Fournier PE, Casalta JP, Piquet P, Tournigand P, Branchereau A, et al. (1998) Coxiella burnetii infection of aneurysms or vascular grafts: Report of seven cases and review. Clin Infect Dis 26: 116-121.