Background: Scabies is an ectoparasitic disease caused by Sarcoptes scabie, an obligate human parasite. Its diagnosis is mainly clinical. Several authors have recently described his resurgence.
Objectives: This study aimed to describe the epidemiological and clinical profile of human scabies and appreciate its therapeutic outcomes in patients seen in consultation at Hospital Aïoun center.
Patients and methods: This is a prospective descriptive study in regional hospital Aïoun (Hodh El Gharbi) over a period from 1st November 2014 to 31 August 2015.
Results: At 10 months, 66 cases were collected, representing a proportional morbidity of 1.6% (mean age 28 years, 59% female). The majority of patients were from urban areas (61%). Family contagion was found in 77% of cases. Among our patients, 64% used the clothes of a member of the entourage. The bad personal hygiene and use lightening cosmetics were observed respectively in 53% and 8% of cases. The clinic was dominated by the nocturnal pruritus associated with scraping ridges (30%), pustules (26%) and vesicles (21%). The main lesions observed sat at the folds or in the inter gluteus (20%), the interdigital spaces (17%), genital lesions (12%) and the armpits (11%). The clinical forms observed were dominated by common form in adults (73%) followed by the common form of infant and children (20%) and profuse form (8%). Among our patients, 33% had a bacterial infection. Under topical anti scabious treatment, antibiotic and antihistamine, the outcome was favorable and no cases of recurrence or complications were observed did.
Conclusion: Scabies is a highly contagious to affection, and especially prevalent neglected. Following this work, we recommend public awareness to behavior changes and early diagnosis and taking appropriate burden of disease in order to prevent the epidemic in communities.
Keywords
Scabies, Diagnosis, Treatment, Benzyle benzoate, Aïoun
Introduction
Scabies or scabiose is a benign skin condition caused by an ectoparasite, the Sarcoptes scabies, hominis variant [1-6]. According to epidemiological data from the World Health Organization (WHO), ubiquitous disorder that affects about 300 million people/year in world [1,3-6]. Favored by promiscuity and lack of hygiene from 1.7 to 11, this is a highly contagious skin disease transmitted by direct human contact or indirect [1,7-11]. Scabies develops as small outbreaks in communities, this infestation to a negative impact on the quality of life of people infected causing stigmatization and ostracism substantial [12]. Clinically, scabies is characterized by an itchy rash with risk of scratching injury and serious secondary infections [13]. Severe forms, particularly contagious, can be observed in immunocompromised patients or elderly 1. Diagnosis is mostly based primarily on clinical [14,15] and its management includes treatment of the patient, his close contacts and disinfection of linen and bedding [2,15]. To our knowledge, no published data available on the pathology in Mauritania. The objective of this study was to determine the epidemiological, clinical human scabies and appreciate its therapeutic results of patients seen at the regional hospital Aïoun in Mauritania.
Patients and Methods
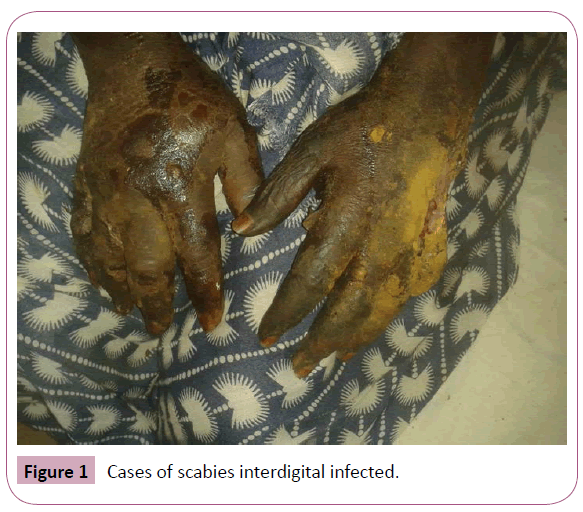
This is a prospective descriptive study in regional hospital Aioun (Hodh El Gharbi) over the period 1st November 2014 to 31 August 2015. This study aimed to determine the epidemiological clinical profile human scabies and appreciate its therapeutic results. Were included in the study all patients seen who described a nocturnal increase in itching and/or a notion of contagion and in whom found on physical examination characteristic lesions of human scabies. Consent to participate in the study was free and informed. Confidentiality, as the anonymity of the patients were observed. For each patient were collected epidemiological data (age, gender, origin), clinical data (date of onset of the disease concept of contagion, clinical signs, maps and complications), therapeutic and evolution. The diagnosis of scabies is held before the presence of intense itching, especially nocturnal and injuries scabious nodules (interdigital spaces, anterior wrists, axillae, umbilicus, areolas breasts in women, penis in men, armpits, scrotum, perineum, or umbilicus, soles in infants) (Figure 1). No biological further examination was made. All patients were treated with benzyl benzoate 10% + 2% Sulfiram (Ascabiol®) in dermal application, at bedtime and an antihistamine therapy was associated to relieve patients. The treatment was accompanied by the recommended hygiene measures. Contacts subjects received the same treatment measures and superinfected cases were treated with cloxacillin before applying the ascaricide. The evolution is marked by a complete and definitive clinical remission at the end of treatment.
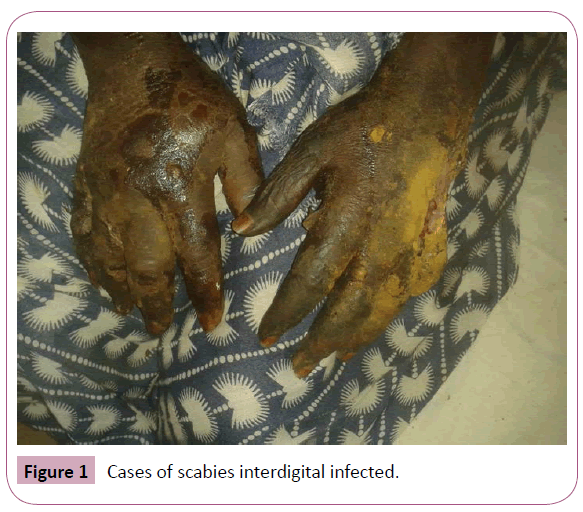
Figure 1: Cases of scabies interdigital infected.
Results
During the study period, 4083 patients were received in consultation including 66 cases of scabies, a frequency of 1.6% (66/4083 consultations). The mean age of the patients was 28 years ± 16 years (range, 2-70). We identified 27 cases (41%) were men and 39 cases (59%) were female, yielding a male/female ratio of 0.7. All patients were living with family and most (61%) came from urban areas. The notion of family contagion was found in 51 cases (77%). Sixty-four percent (64%) of our patients said exchanging clothes with relatives. Poor personal hygiene was observed in 35 cases (53%). Among our patients, four cases (8%) used cosmetic products to whiten or lighten their skin.
Overall clinical signs were dominated by the nocturnal pruritus associated with scraping ridges (30%), pustules (26%) and vesicles (21%). Main observed lesions are noted in Table 1. Achieving inter or under gluteal folds was observed in 20% of cases, followed by inter digital spaces (17%) and genital lesions (12%) (Table 2). The clinical forms observed were dominated by common form in adults (73%) followed by the common form of infant and children (20%) and the profuse form (8%). Cases of secondary infections were observed in 22 cases (33%). Under topical anti-scabious treatment, antibiotic and antihistamine, the outcome was favorable. No case of recurrence was observed was after a month of treatment.
| Skin lesion observed |
Frequency |
Percent |
| Streaks scrapings |
20 |
30% |
| Pustules |
17 |
26% |
| Vesicles |
14 |
21% |
| Sillionsscabious |
4 |
6% |
| Nodules |
4 |
6% |
| Vesiclo-papuleux |
3 |
5% |
| Papules |
2 |
3% |
| Crusts |
2 |
3% |
Table 1: Types of skin lesion observed.
| Topography of lesions |
Frequency |
Percent |
| Inter or under gluteal folds |
13 |
20% |
| Interdigital spaces |
11 |
17% |
| Genital lesions |
8 |
12% |
| Armpits |
7 |
11% |
| Diffuse |
5 |
8% |
| Umbilicus |
5 |
8% |
| Wrist |
5 |
8% |
| Thighs |
4 |
6% |
| Scalp |
3 |
5% |
| Back |
3 |
5% |
| Breast areola |
2 |
3% |
Table 2: Topography of lesions.
Discussion
Our study has limitations that should be considered. First, the method of recruitment in hospital reduces the size of our sample.
Furthermore, the diagnosis was made only on a clinical basis. Finally, this prospective study was conducted over a short period (10 months) which could have influenced. The prevalence observed which, however, was 1.6%. Scabies is not a reportable disease, which would explain its variable prevalence across the world [1,2,13,16,17]. Several studies have reported a high prevalence in communities that had low socioeconomic status [1,2,7,9,11,15,17,18]. A study conducted by WHO had collected data from 18 surveys in prevalence between 1971 and 2001, had reported a prevalence of scabies between 0.2% and 24% [13]. In our study the average age was 28 ± 16 years (2 to 70 years). This figure was higher than that reported by Kouotou et al. [18]. The female (59%) was mainly represented in our study. A male predominance has been reported by other authors [18,19]. All patients were living with family and most (61%) came from urban areas. Similar observations have been reported by Kobangué et al. at Bangui who had observed that 94% of patients with scabies were residing in urban areas [19]. In our study, the notion of familial contagion was found in 77% of cases. This percentage is higher than that found in Bangui and Yaounde [18,19]. This high prevalence in our study could be explained partly by the fact that patients lived in community and frequently exchanged several objects, including clothes (64%) and partly by the negligence of personal hygiene (53%). These results are similar to those previously reported by other authors, who found that scabies reached with predilection people with defective personal hygiene [1-3,13-15,18,20-26]. Eight percent (8%) of our patients were using cosmetics to depigment (to whiten or lighten their skin). Other authors have found a link between this phenomenon and scabies long term [27,28]. The use lightening cosmetics can cause side effects including skin disorders that promote skin infestations such as scabies.
Clinically, we found all the classic functional signs of scabies with chronic pruritus night as the most common sign. Our results are similar to those reported in the literature [3,11,13,16,22,29]. Regarding the preferential localization of lesions, Kouotou et al. had already noted the predominance at the inter-gluteal folds or under and cuffs [18]. In addition, the low frequency of diffuse sites (8%) we noticed was low compared to that found in other studies [18,19].
As for the clinical forms, we observed a predominance of the common form in adults (73%). This dominance could be explained partly by the poor hygiene in some households and secondly by the very limited bathroom due to lack of water. The common form of infant and child was observed in 20% of cases. This could be explained by the fact the most important vulnerability of children because of close physical contact with their parents or other members of the entourage. Several studies have reported a high prevalence of scabies in pediatric environment [19,25,30]. Profuse form (8%) in our study was observed only in women who use topical steroid creams lightening of the skin. Similar observations have been reported by other authors [27,28].
The outcome was favorable in all our patients and no cases of recurrence or complication of treatment were noted in our study.
Other factors that may influence the effectiveness of treatment were taken into account including the treatment of patient contacts, disinfect the patient environment, linens and bedding. Cases of human scabies should always be accompanied by relatives seeking to contact investigation infested and treatment of potentially contaminating machine to avoid an epidemic in communities.
Conclusion
Scabies is a highly contagious disease responsible for outbreaks in disadvantaged families often neglected as a public health problem. Its diagnosis is based mainly on the epidemio-clinical arguments but often difficult to confirm and therapeutic management requires strict synchronization between patient treatment, contacts topics and disinfection of the environment. The effective prevention of disease and its spread requires both awareness of populations to changes in behavior and as practitioners in the diagnosis and early treatment to limit its spread and secondary infections.
7305
References
- Chosidow O (2006) Clinical practices. Scabies. N Engl J Med 354: 1718-1727.
- Andriantsoanirina V, Izri A, Botterel F, Foulet F, Chosidow O, et al. (2014) Molecular survey of knockdown resistance to pyrethroids in human scabies mites. ClinMicrobiol Infect 20: O139-141.
- Kosanovi A, Li A, Ina ML, Quiaios A, Teaia V, Domingues J, Sai N (2014) The profile of scabies patients in Zagreb. PsychiatrDanub 26 Suppl 3: 533-536.
- Thomas J, Peterson GM, Walton SF, Carson CF, et al. (2015) Scabies: an ancient global disease with a need for new therapies. BMC Infect Dis 15: 250.
- Walker GJ, Johnstone PW (2000) Interventions for treating scabies. Cochrane Database Syst.
- McCarthy JS, Kemp DJ, Walton SF, Currie BJ (2004) Scabies: more than just an irritation. Postgrad Med J 80: 382-387.
- Lohezic-Le Devehat F, Marigny K, Doucet M, Javaudin L (2002) Grapefruit juice and drugs: a hazardous combination? Therapie 57: 432-445.
- Hengge UR, Currie BJ, Jäger G, Lupi O, Schwartz RA (2006) Scabies: a ubiquitous neglected skin disease. Lancet Infect Dis 6: 769-779.
- Utsumi M, Makimoto K, Quroshi N, Ashida N (2010) Types of infectious outbreaks and their impact in elderly care facilities: a review of the literature. Age Ageing 39: 299-305.
- Spadoni S, Lamand V, Vonesch MA, Béranger C (2014) [Scabies: A world plague]. Med Sante Trop 24: 41-48.
- Bouvresse S, Chosidow O (2010) Scabies in healthcare settings. CurrOpin Infect Dis 23: 111-118.
- Hay RJ, Steer AC, Engelman D, Walton S (2012) Scabies in the developing world-its prevalence, complications, and management. ClinMicrobiol Infect 18: 313-323.
- Walton SF, Currie BJ (2007) Problems in diagnosing scabies, a global disease in human and animal populations. ClinMicrobiol Rev 20: 268-279.
- Gaspard L, Laffitte E, Michaud M, Eicher N, Lacour O, et al. (2012) Scabies in 2012. Rev Med Suisse 8: 718-772.
- Romani L, Steer AC, Whitfeld MJ, Kaldor JM (2015) Prevalence of scabies and impetigo worldwide: a systematic review. Lancet Infect Dis 15: 960-967.
- Berenji F, Marvi-Moghadam N, NaghibozakerinMeibodi P (2014) A retrospective study of ectoparasitosis in patients referred to Imam Reza Hospital of Mashhad, Iran. Biomed Res Int 2014: 104018.
- Kouotou EA, Nansseu JR (2015) Features of human scabies in resource-limited settings: the Cameroon case. BMC Dermatol 15: 12.
- Kobangué L, Guéréndo P, Abéyé J, Namdito P, Mballa MD, et al. (2014) Scabies: epidemiological, clinical and therapeutic features in Bangui. Bull SocPatholExot 107: 10-14.
- Scott GR, Chosidow O (2011) European guideline for the management of scabies, 2010. Int J STD AIDS 22: 301-303.
- Karim SA, Anwar KS, Khan MA, Mollah MA, Nahar N, et al. (2007) Socio-demographic characteristics of children infested with scabies in densely populated communities of residential madrashas (Islamic education institutes) in Dhaka, Bangladesh. Public Health 121: 923-934.
- Hegab DS, Kato AM, Kabbash IA, Dabish GM (2015) Scabies among primary schoolchildren in Egypt: sociomedical environmental study in Kafr El-Sheikh administrative area. ClinCosmetInvestigDermatol 8: 105-111.
- Talukder K, Talukder MQ, Farooque MG, Khairul M, Sharmin F, et al. (2013) Controlling scabies in madrasahs (Islamic religious schools) in Bangladesh. Public Health 127: 83-91.
- Terry BC, Kanjah F, Sahr F, Kortequee S, Dukulay I, et al. (2001) Sarcoptesscabiei infestation among children in a displacement camp in Sierra Leone. Public Health 115: 208-211.
- Boralevi F, Diallo A, Miquel J, Guerin-Moreau M, Bessis D, et al. (2014) Clinical phenotype of scabies by age. Pediatrics 133: e910-916.
- Piérard-Franchimont C, Hermanns-Lê T, Piérard GE (2014) Diagnosis and evolution of scabies. Rev Med Liege 69: 467-470.
- Morand JJ, Ly F, Lightburn E, Mahé A (2007) Complications of cosmetic skin bleaching in Africa. Med Trop (Mars) 67: 627-634.
- Mahé A, Ly F, Aymard G, Dangou JM (2003) Skin diseases associated with the cosmetic use of bleaching products in women from Dakar, Senegal. Br J Dermatol 148: 493-500.
- Mumcuoglu KY, Gilead L (2008) Treatment of scabies infestations. Parasite 15: 248-251.
- Romani L, Koroivueta J, Steer AC, Kama M, Kaldor JM, et al. (2015) Scabies and impetigo prevalence and risk factors in Fiji: a national survey. PLoSNegl Trop Dis 9: e0003452.