Key words
tension-type headache, epidemiology, prevalence, risk factors, comorbidities.
Abbreviations
TTH, tension-type headache; CTTH, chronic tension type headache; IHS, International Headache Society; HDI, Headache Disability Index; CDH, chronic/daily headache.
Introduction
Headache is one of the most common complaints encountered in Internal Medicine and Pediatric and Adult Neurology clinics. It has reported that the vast majority of headaches are tension-type headache (TTH) and migraine [1-10]. TTH is defined as mild to moderate band-like pressure headache with few associated symptoms. It varies considerably in frequency and duration, from rare, short-lasting episodes of discomfort to frequent, long-lasting, or even continuous disabling headaches. Chronic (CTTH) is defined as TTH that occurs ≥15 days a month [11]. It has been identified that poor self-rated health, stress (mental or physical), anxiety, depression, temperament instability, i.e., higher emotionality (i.e. higher level of shyness and intensified level of fear), reduced or inappropriate physical exercise, irregular or inappropriate meals, poor posture and high intake of coffee and dehydration, are risks or triggers for TTH [12-15]. Pericranial muscle tenderness on palpation is the most common abnormal finding in episodic TTH (ETTH) although its absence does not rule out TTH. Anxiety or depression considerably increase the level of muscle tenderness in the head and neck [16]. For CTTH, somatic complaints as generalized myalgias, arthralgias, sleep difficulties, chronic fatigue, carbohydrate craving, decreased libido, irritability and disturbed memory and concentration, are common [17]. Stovner et al. [18] reported that approximately 60% of individuals with TTH experienced no more than one headache attack per month, but about 40% had several per month and about 4% had headache at least half the days of the year. In a population-based study done by Lyngberg et al. [13] in Denmark, the authors reported that 24% to 37% had TTH several times a month, 10% had it weekly and 2% to 3% of the population had CTTH.
It is a common trend among clinicians that if a patient meets the criteria for TTH and has unremarkable neurological examination, there will be no need for further diagnostic testing. However, neuro-imaging is indicated in presence of atypical pattern of headache, seizures, neurological signs (i.e. possibility of the diagnosis of secondary headache), symptomatic illnesses as tumor, etc [19].
The pathophysiology of TTH is multifactorial and varies between individuals. It has been suggested that episodic TTH (ETTH) is predominantly a disorder of peripheral mechanisms (myofascial nociception), while CTTH reflects a central mechanisms (sensitization and inadequate endogenous pain control). It has been suggested that recurrent bouts of TTH may lower the threshold for new episodes by altering the myofascial tissues (myofascial trigger points) and increase the sensitivity of neurons of the trigeminal tract (Peripheral Sensitization). Muscle tenderness and psychological tension was found to be associated with and aggravate TTH. CTTH has been found to be associated with continuous nociceptive input from pericranial myofascial tissues, the nociceptive second-order neurons in the spinal dorsal horn (2nd& 3rd cervical segments) and the trigeminal nucleus caudalis (central sensitization) with hypofunction of the central opioid system (defective central antinociceptive system) [20].
Several large-scale epidemiological studies, population- based studies, self-report questionnaires, data collected from medical records, hospital-based studies, etc, have found that TTH, although common, has a variable prevalence worldwide. In crosssectional epidemiologic studies, it was observed that the prevalence of TTH peaked between ages 30-39 regardless of gender and decreases slightly with age [21]. The average age of onset of TTH was estimated to be 25-30 years. The female to male ratio was estimated to be nearly 5:4, which indicates that women were affected only slightly more than men [2, 4, 5, 6, 7, 9, 10, 18]. TTH was also identified during childhood [1, 3, 8, 22] andin the 5th decade of life [23].
Rasmussen et al. [21] in their population-based study reported that the lifetime prevalence of TTH was 79%, with 3% were CTTH. In a longitudinal study of Waldie and Poulton [24] which was done on age ranged between birth to age 26, the 1-year prevalence was reported to be 11.1% at age 26 for TTH compared with 3.2% for migraine. Buchgreitz et al. [25] reported that the lifetime prevalence of frequent episodic TTH was 17% and 4% for CTTH and the point prevalence of TTH was 15% (of them 15% had infrequent ETTH, 16% had frequent ETTH, 12% had CTTH and 57% had coexisting migraine). In adult population, it was found to range from 3.1% in Saudi Arabia [26] to 84.7% in Norway [27]. It was observed from five population based studies that the life time prevalence of ETTH was 46% (range 12-78%) [18]. The prevalence of TTH was found to range from 0.5% at 7-years old and 2.4% at 12-years old in Serbia [3] to up to 55% between age of 7 to 14 years in Germany [28].
As TTH is one of the most common primary headaches, it is important to identify the epidemiology of TTH across populations through various age groups, its risk factors and co-morbid conditions for proper identification of the exact neurobiology, management, and outcome and so improving individuals’ quality of life and lessen the economic burden.
Aim of work
The work in this study was aimed to: 1) determine the prevalence and epidemiological characteristics of different types of TTH in Assiut District, Egypt; 2) detect the frequency and the important predictors of severity, duration, frequency and change to chronic form of TTH; and 3) determine the important risk factors and co-morbid conditions associated with TTH to determine their emphasis to the clinical impact and importance in patients’ management.
Materials and methods
The study design
Assiut governorate (located in south Egypt, nearly 400 kilometers from Cairo) has a population size of 3,444,967 [Urban: n = 1,636,359, 47.5%; Rural: n = 1,808,856, 52.5%]. Urban area is divided into 15 Shiakhats which are distributed as 9 (26.4%) in the 1st section and 6 (21.1%) in the 2nd section. Rural area is divided into 30 villages, 17 in the north and 13 in the south [29]. This is a population- based door-to-door cross-sectional study, done throughout one year (2009) in Assiut district, Egypt. It included 4700 randomly selected individuals without prior knowledge of their health or social background. Sample was classified according to the percentage of population in urban (n = 2230, 47.5%) and rural (n = 2470, 52.5%) places. We selected 9 areas, [urban = 5 , 3 from the 1st section (n = 1338) and 2 from the 2nd section (n =892)] and 4 rural [2 villages from the north areas (n = 1235) and 2 villages from the south (n = 1235)]. In urban area, first section include: Al-Shiakha Al-thaltha, Al- Biseri and Al-Sharikat and second section include: Al-Shiakha Al-saba and El-Walidia. In rural area, first section include: Elwan and Banighalib and second section include: El-matea and Awlad Ibrahim. Sample size determination was calculated according to EPI info version 3.5.1 [30]. Cluster sample technique was used. In each selected area we started from its center and went in one direction in radial manner visiting all households till the required number was reached. TTH was diagnosed according to the International Headache Society (IHS) diagnostic criteria [11]. Excluded from the study were the followings: 1) subjects who refused to participate (n = 1203) and those with unreliable answers (n = 324). The causes of refusal were variable, as fear from strangers, fear from detecting serious disease or simply being uninterested. The causes of un-reliability were: false positive response as a way to measure the blood pressure or false negative response as a way of refusal. We compensated the number of excluded individuals till the target number of individuals was obtained (n = 4700), 2) other primary headache types and 3) secondary headache.
The protocol of this work was approved by the ethics committee of faculty of medicine, Assiut University, Egypt and all participants gave their consent to participate.
The research description
Field team included a neurologist (KOM) and one paramedical stuff member. The paramedical staff introduced the objectives of the study and the neurologist interviewed headache sufferers using a detailed sheet which included medical and neurological history and examination. Questions regarded headache characteristics included: headache description, precipitating, aggravating and relieving factors, co-morbid conditions or related medical conditions and a family history of headache. The frequency of the attacks of headache were classified as follow: a) infrequent episodic: if the individual experiences 1 attack every 2-4 months, b) frequent episodic: if the individual experiences 1-14 attacks per month, c) chronic: if individual experiences ≥ 15 attacks per months, d) chronic daily headache: if the individual experiences one attack per day for 3 months. Headache Disability Index (HDI) was also calculated as a marker of headache severity [31]. Measurement of the educational level and social and economic levels were determined as follow [32]: regarding educational level, it was considered a) low: if the subject was before school age, illiterate, can read and write or in primary school, b) middle: if the subject was in a secondary or a tertiary school, and c) high: if the subject had a bachelor, master, Ph.D. or M.D. degrees. Regarding socioeconomic class, it was considered a) low: if score was < 50, b) middle: if score was >50-<140, and c) high: if score >140.
TTH sufferers were invited to attend our out-patient headache clinic whenever needed for proper assessment. Follow up was done monthly. The decision to investigate the patient was based on clinical suspicion to exclude red and blue flags of secondary headache. Investigations included electroencephalography (EEG), computed tomography (C.T) or magnetic resonance imaging (MRI) for the brain whenever needed.
Statistical analysis
Calculations were done with the statistical package SPSS, version 12.0. Data were presented as mean±SD (standard deviation) as they were normally distributed. Unpaired two-sided Student’s t test was used for comparison of means and Chi-square (χ2) test for numerical variables. Estimation of prevalence rates of different headache types was done by dividing the total number of headache suffers over the total population at risk. Correlations between clinical characteristics, risk factors, co-morbid conditions and severity of headache were determined using Pearson’s test and Spearman rank correlation coefficient. 95% confidence intervals (95% CI) were calculated using a binomial approximation of the Poisson distribution. Univariate logistic regression followed by binary logistic regression analysis using forward LR variable selection method, followed by calculation of 95% CI were used to determine the predictors for transformation from episodic to chronic headache. For all tests P-value <0.05 was considered significant.
Results
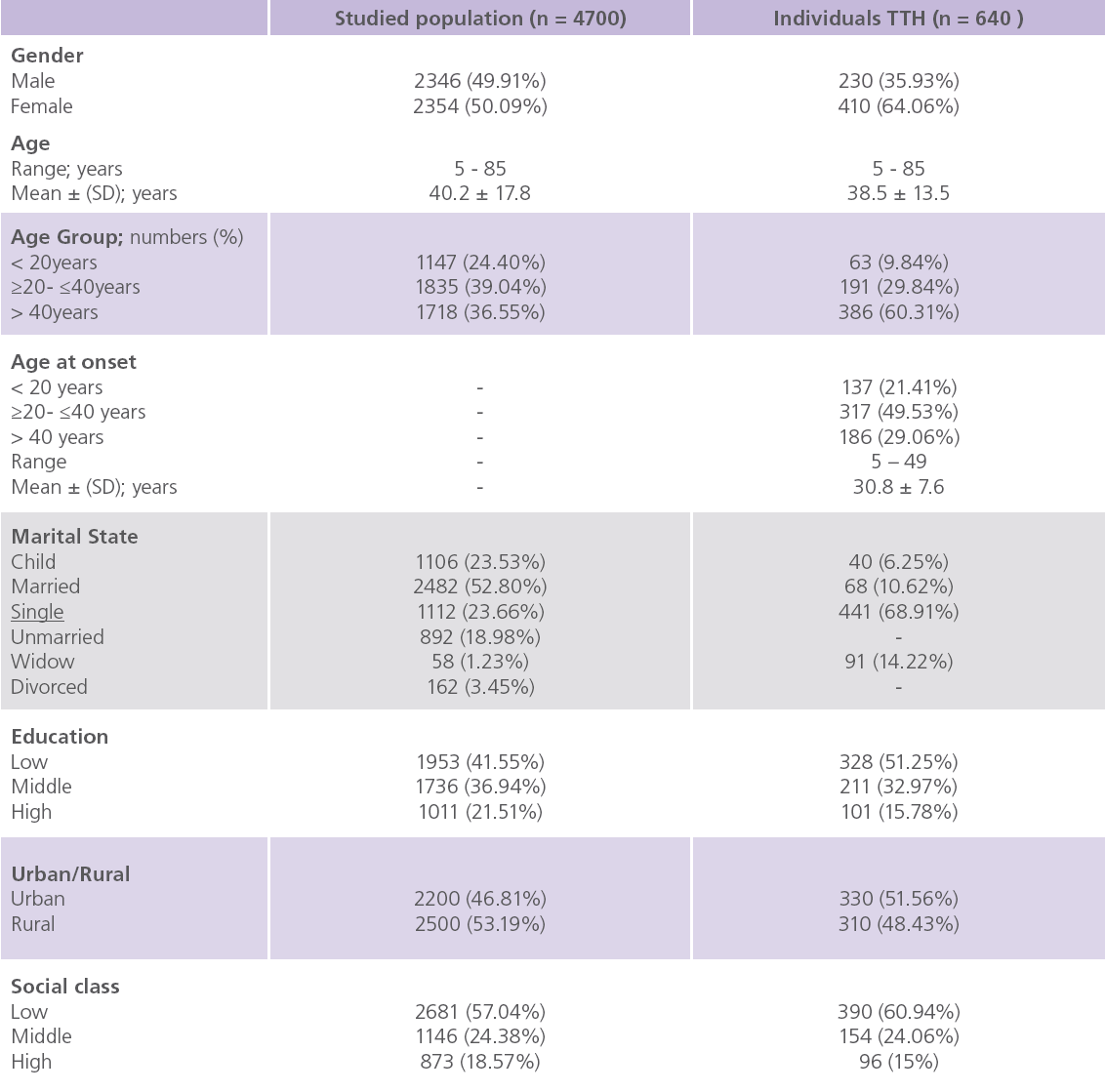
Table 1., showed the socio-demographic characteristics of the studied population and individuals with TTH. This study included a total of 4700 individuals (male: 2346, 49.91%; females: 2354, 50.09%). Of them, 75.6% were ≥ 20 years, 24.63% were children, 52.8% were married, 78.5% had low/middle educational levels and 57.04% were of low socioeconomic status. The mean age of TTH sufferers was 38.5 ± 13.5 years, the mean age at onset was 38.5 ± 13.5 and was significantly lower in males (P = 0.007) and female-to-male ratio was 1.8:1. Nearly 68.91% were singles, 51.25% were of low educational level and 60.94% had low social class. Family troubles were identified as the most frequent precipitating factor for TTH (69.5%) followed by glair (39.7%), fasting (21.4%) and early insomnia (19.7%).
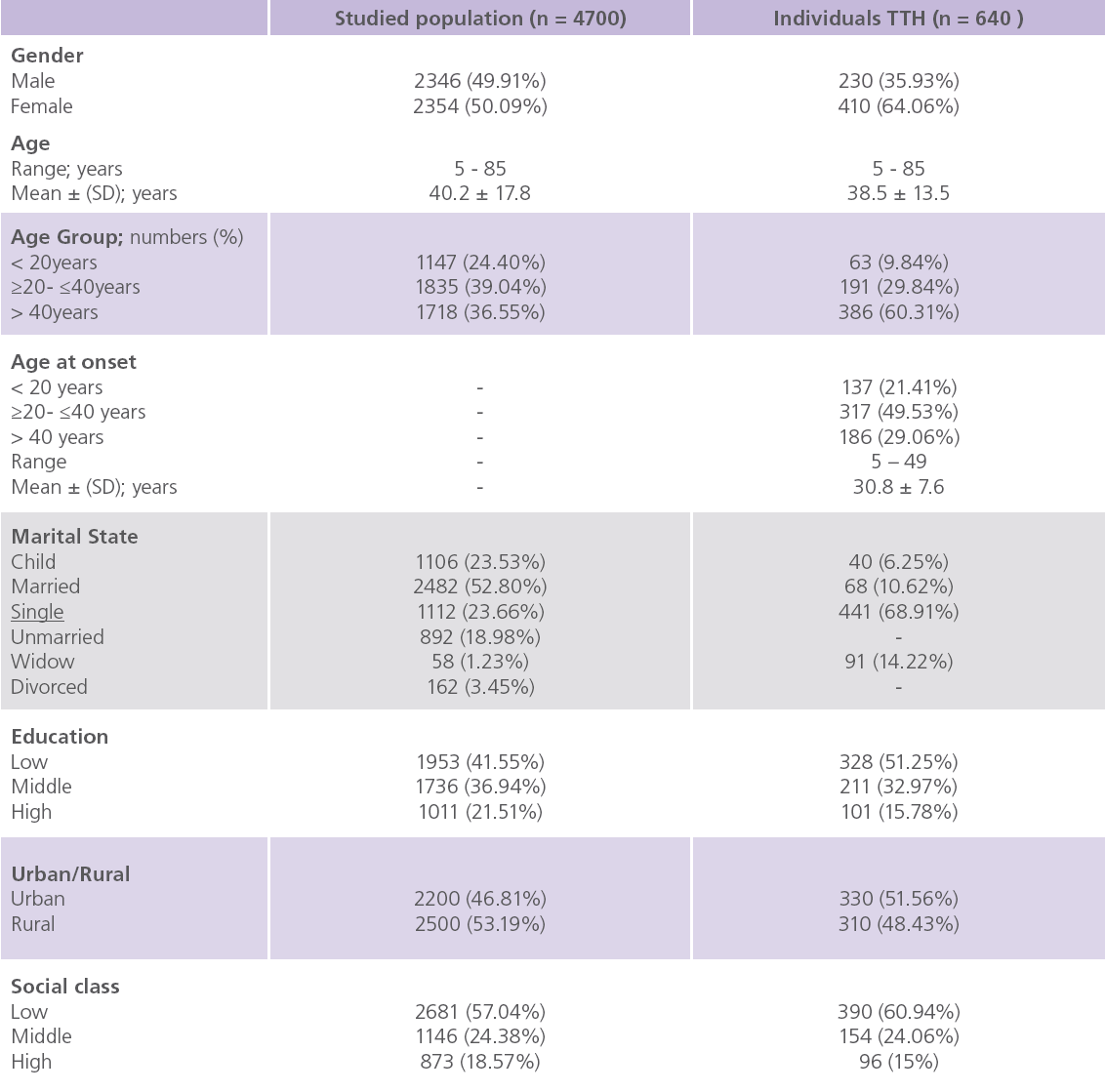
Table 1: Socio-demographic characteristics of the studied population and individuals with TTH.
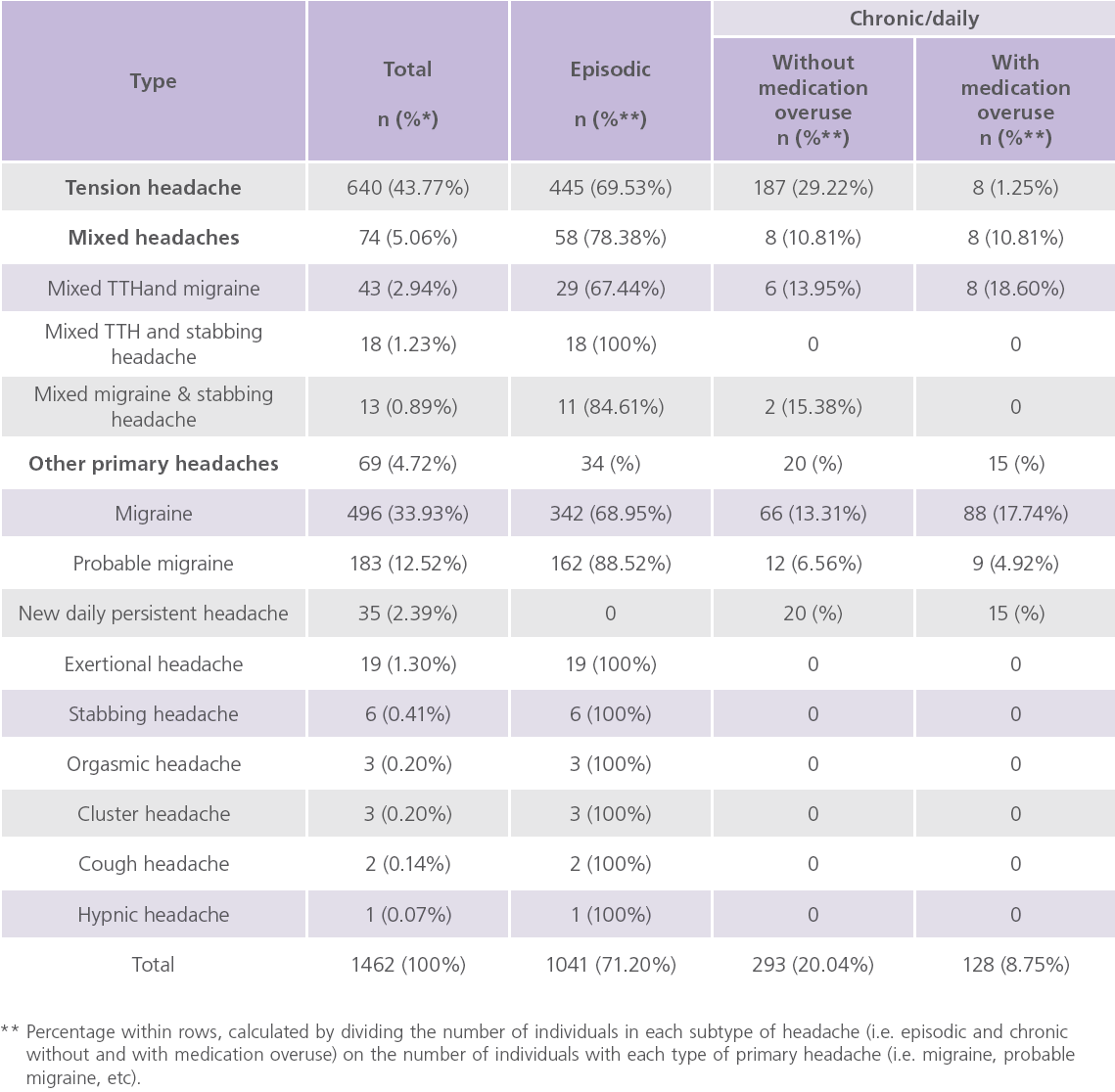
We reported headache in 35.49% (n = 1668), of them 87.65% (n = 1462) had primary headache, of them 43.78% (n = 640) had TTH, 33.94% for migraine, 12.52% for probable migraine, 4.72% for other primary headaches and 5.06% for mixed headaches (table 2). Frequent episodic TTH was reported in 48.2%, 11.10% for infrequent episodic TTH, 21.4% for chronic TTH and 19.3% for chronic daily headache.
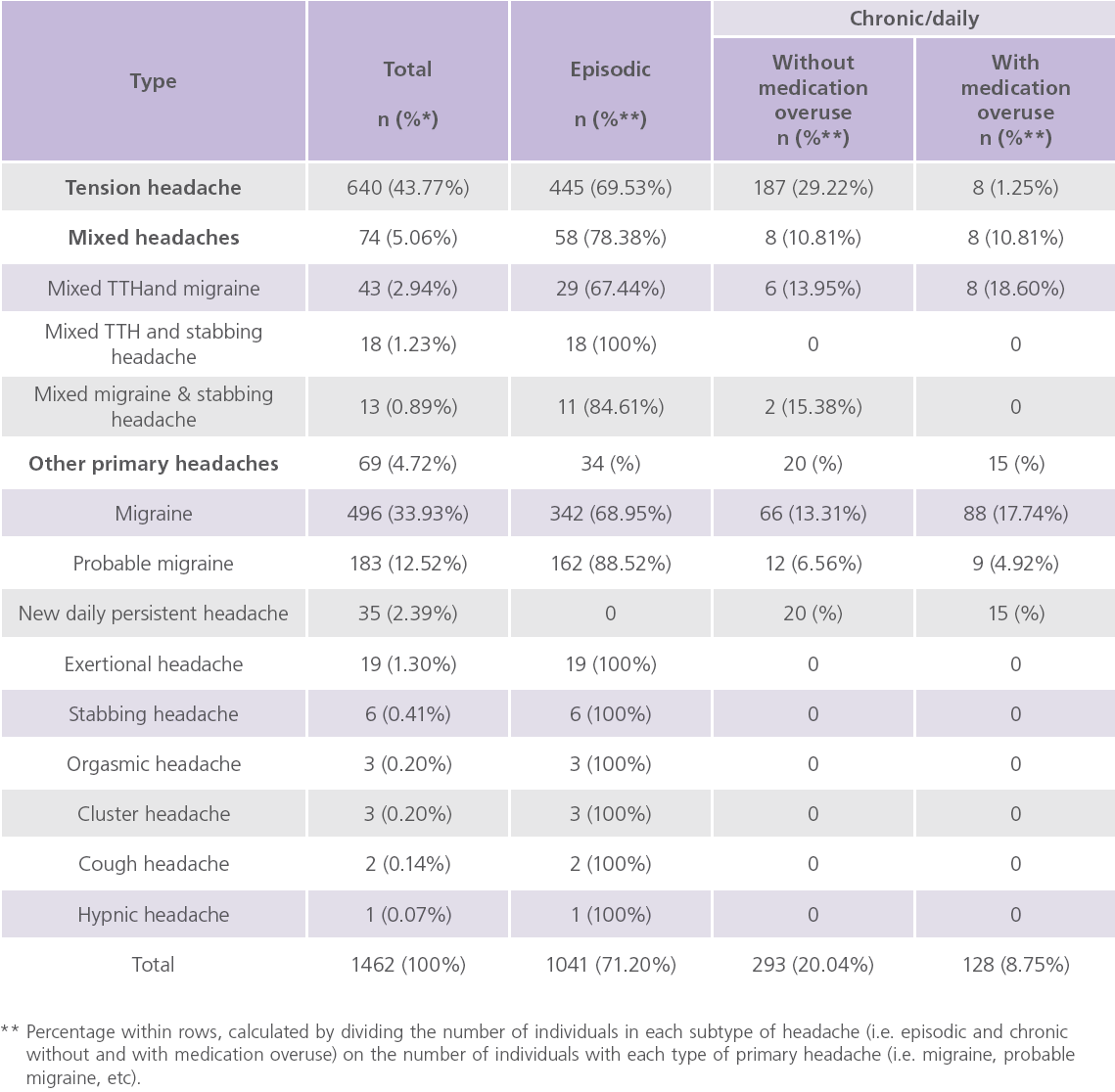
Table 2: Number and percentage of different types of primary headaches.
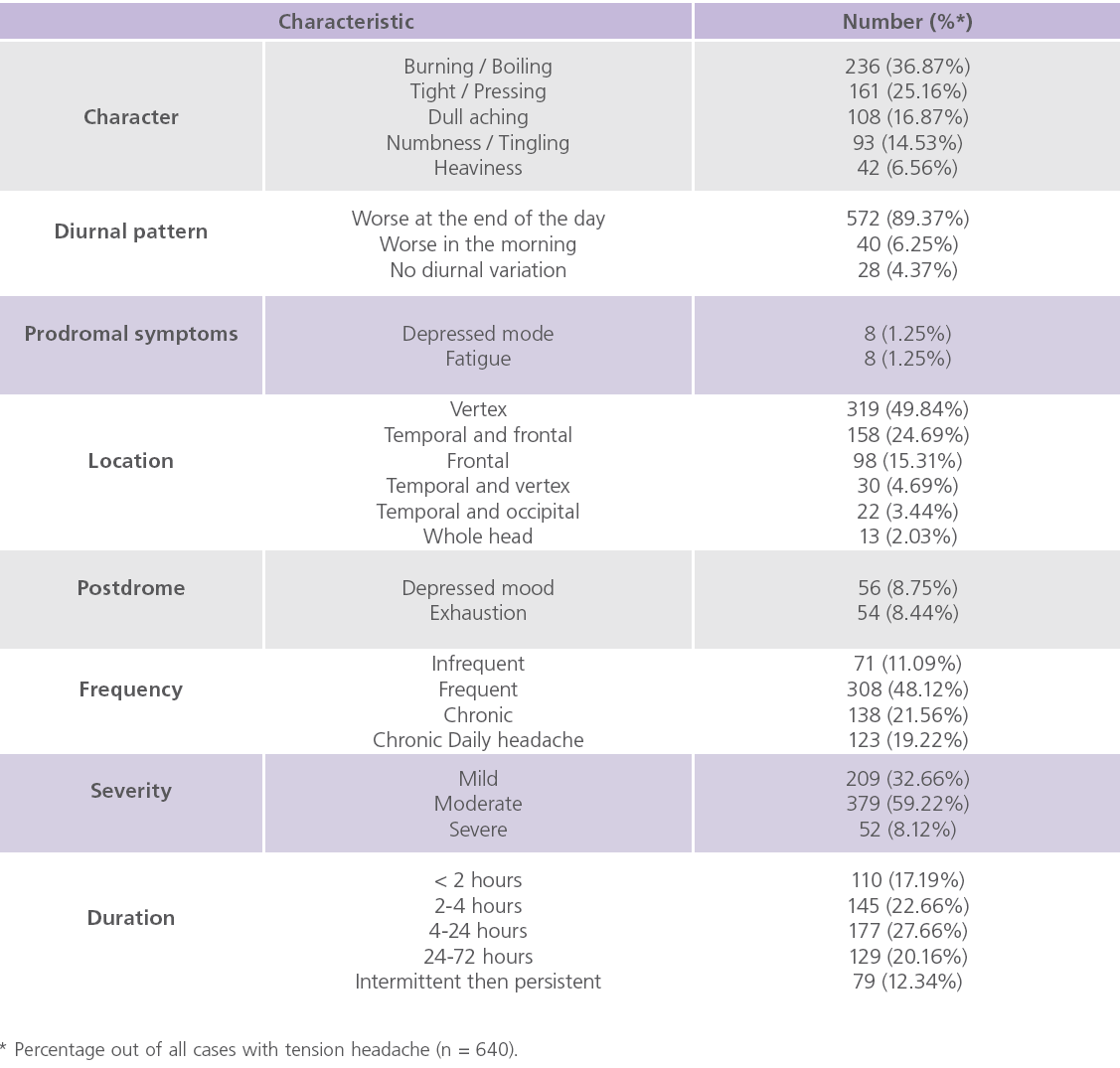
Table 3, showed the clinical characteristics of TTH in the studied population. The identified clinical manifestations of TTH include: scalp tenderness (23.4%),
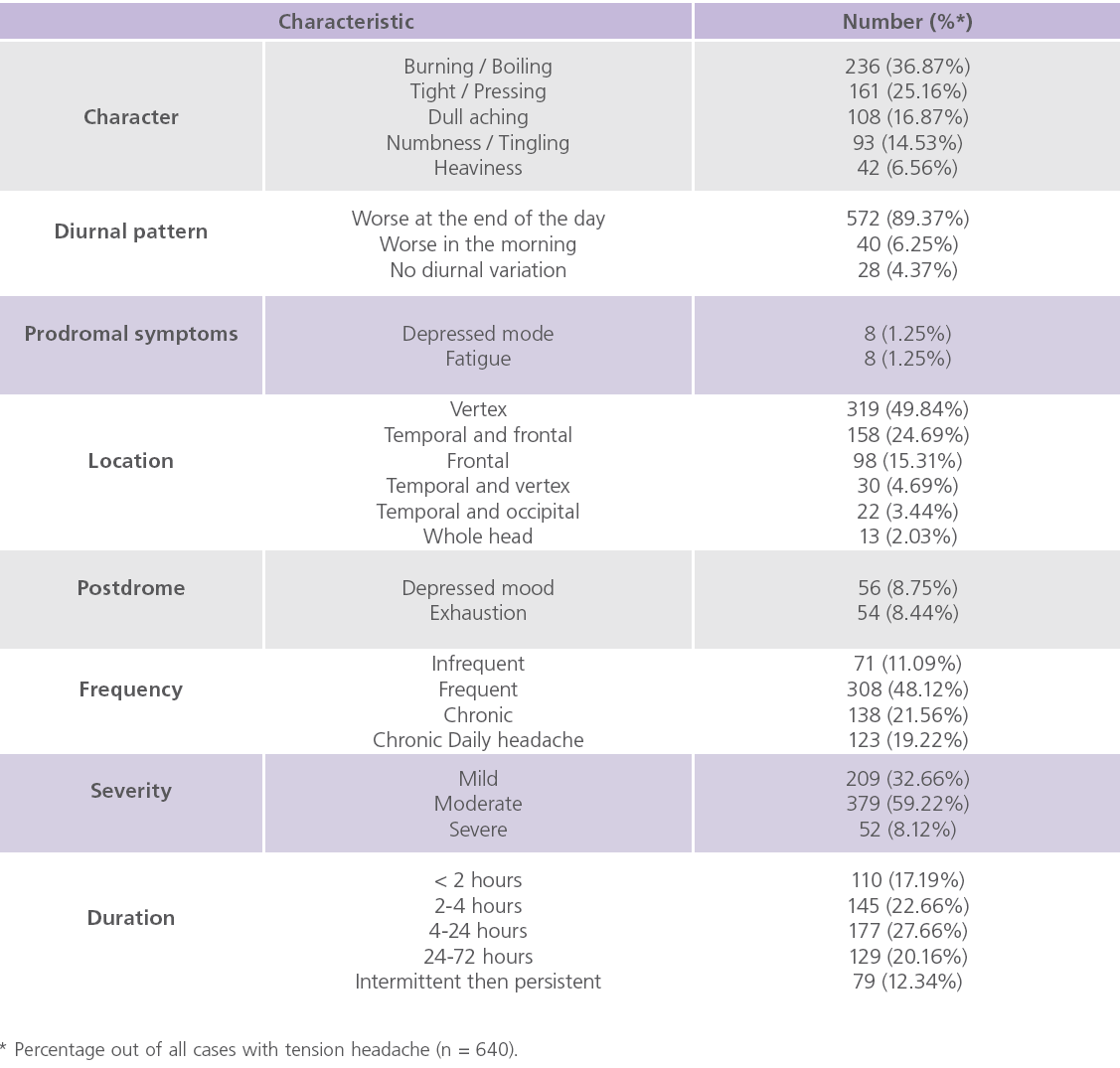
Table 3: Clinical characteristic of TTH.
lacrimation (14.7%), blurring of vision (8.6%), photophobia (7.5%), insomnia (6.5%), nausea (4.7%) and vomiting and eye burning (0.6% for each). The most common relieving factors for TTH were rest (45.5%) and self-medications (25.8%).
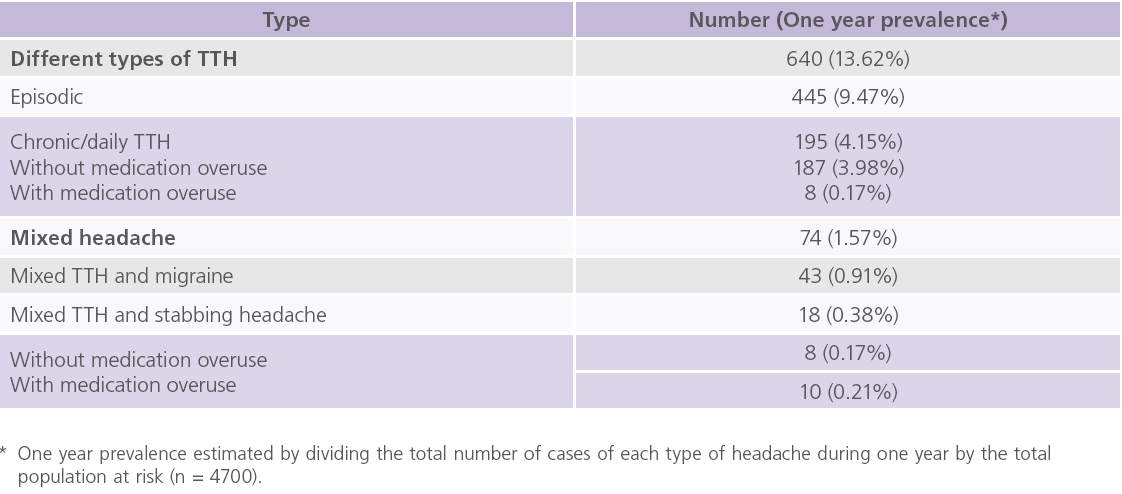
Nearly 59.22%/32.66% had moderate/mild attacks. We reported that anxiety (27.3%), depression (23.8%) and hypertension (20.5%) were the common co-morbid conditions associated with TTH. Only 1.2% had co-morbid medication overuse headache while TTH was the common reported condition in the families of individuals with TTH (27.7%). We reported an overall prevalence of primary headaches to be 31.11%, among them 13.62% for TTH, 10.55% for migraine, 3.89% for probable migraine, 1.57% for mixed headache and 1.47% for other primary headaches (table 4).
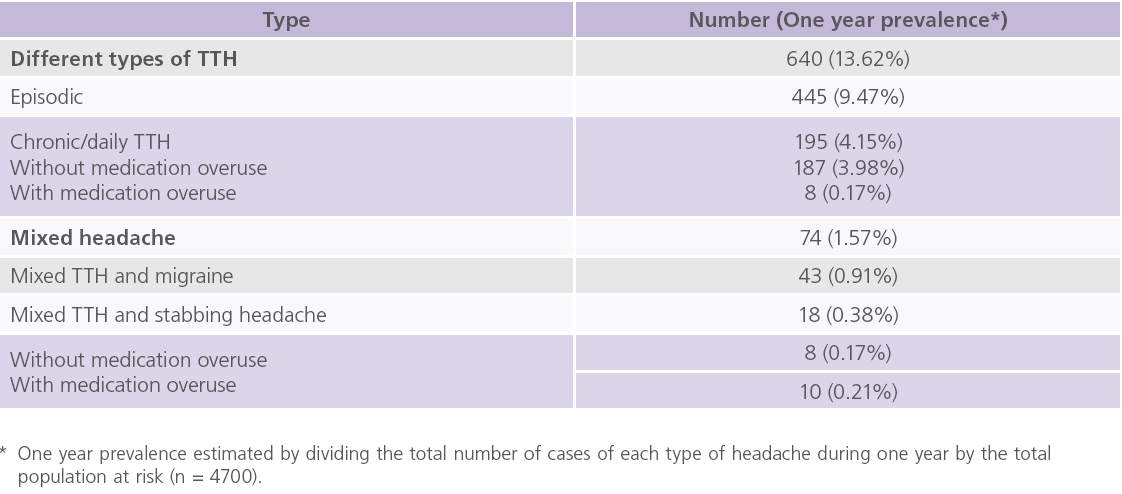
Table 4: Prevalence of TTH.
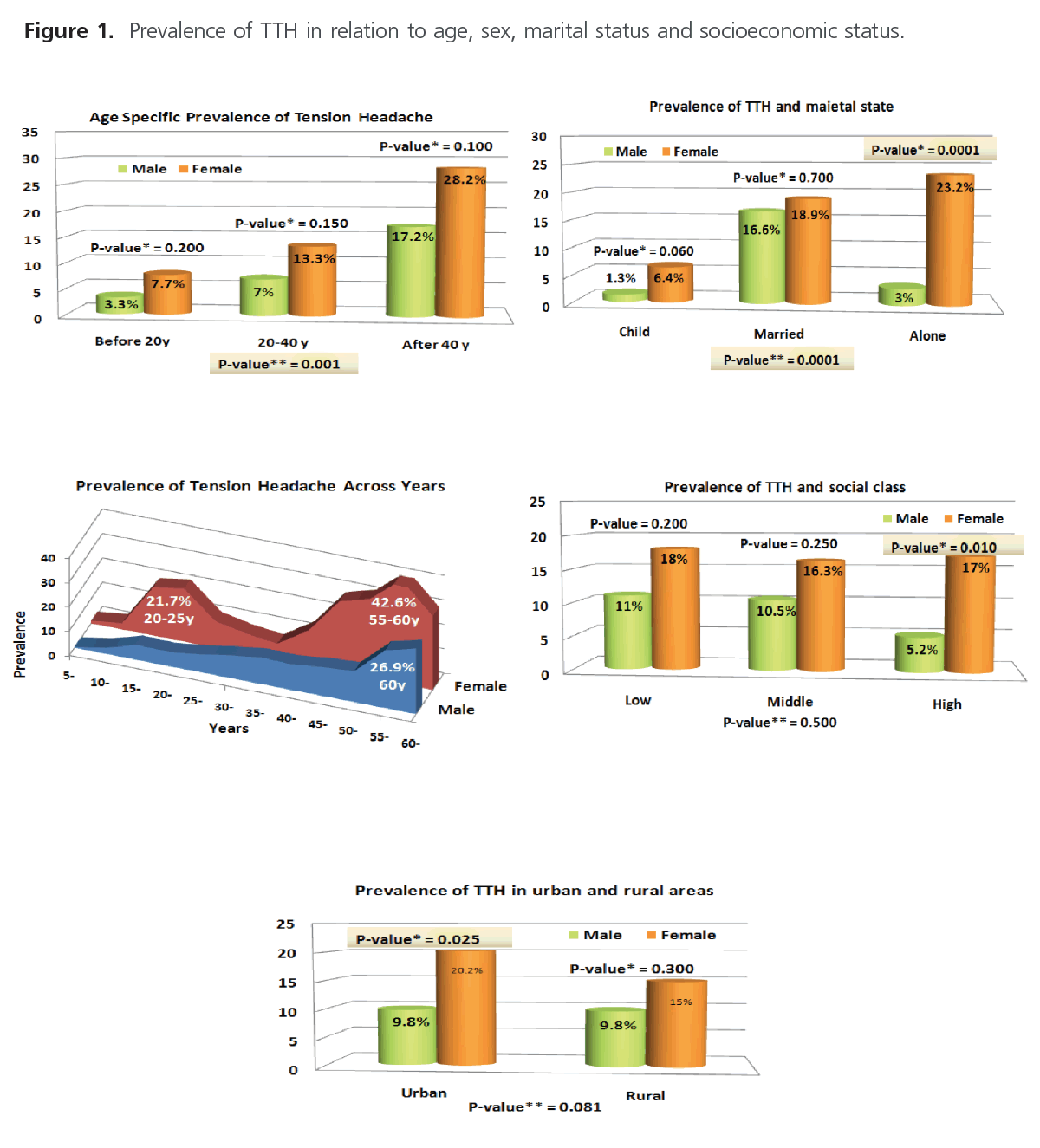
Table 5 and (figure 1) showed the prevalence of TTH in relation to age and in relation to age, sex, marital status and socioeconomic status. The prevalence of TTH was reported to be higher among adults, females, singles, rural residents and those with low socioeconomic states.
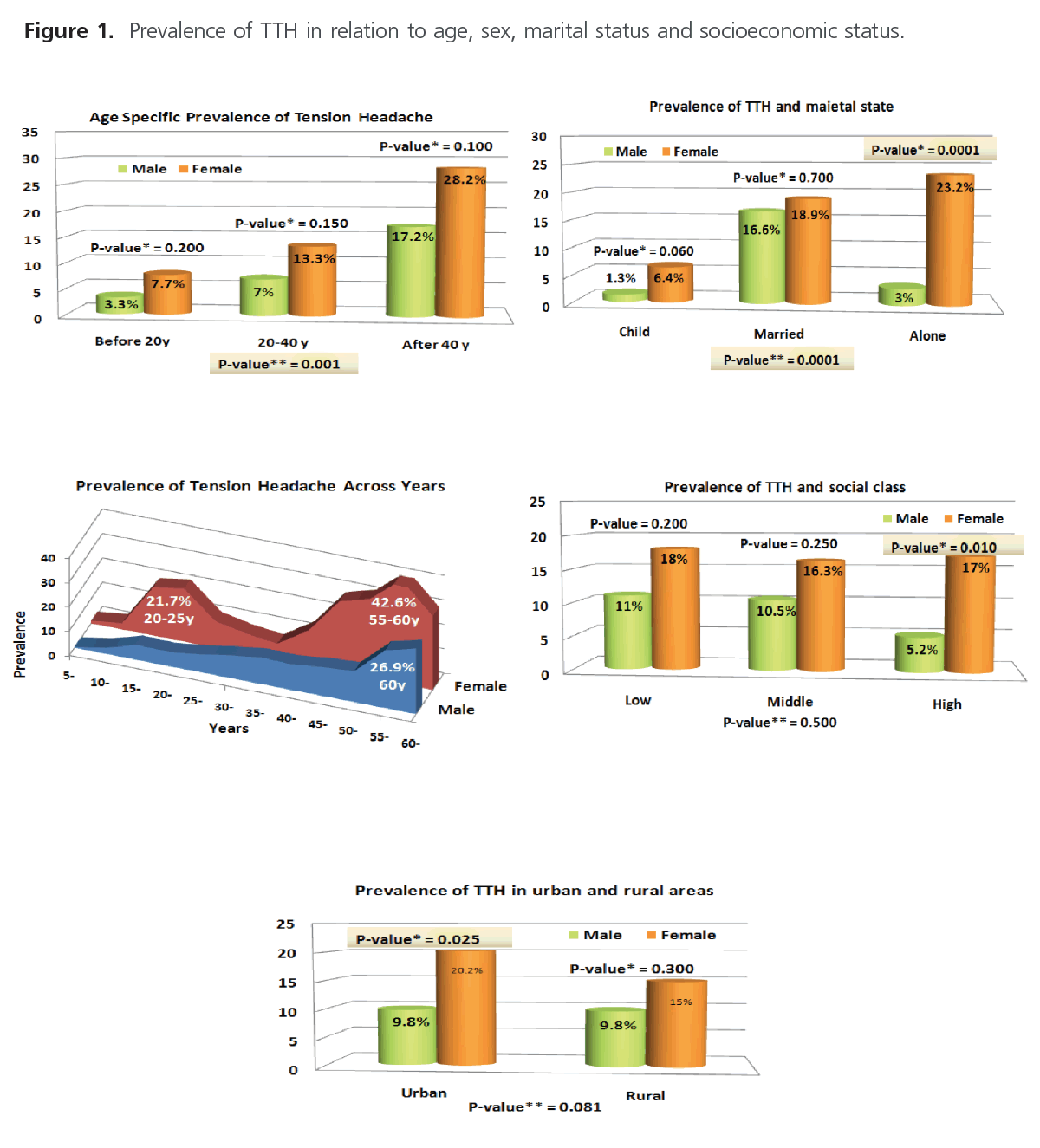
Figure 1: Prevalence of TTH in relation to age, sex, marital status and socioeconomic status.
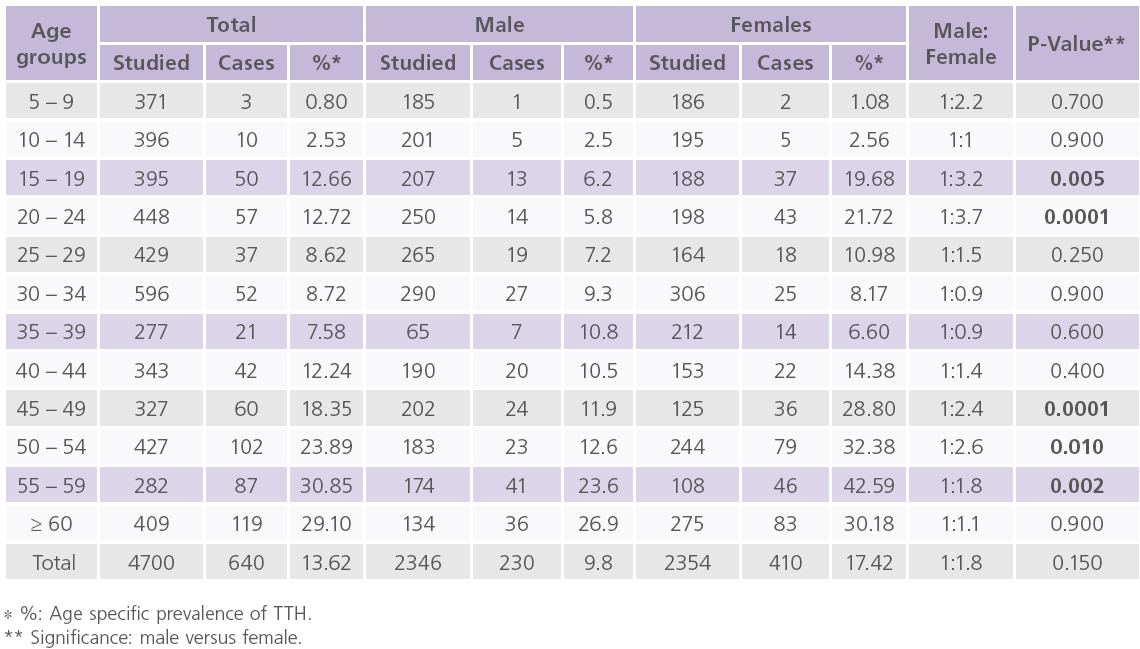
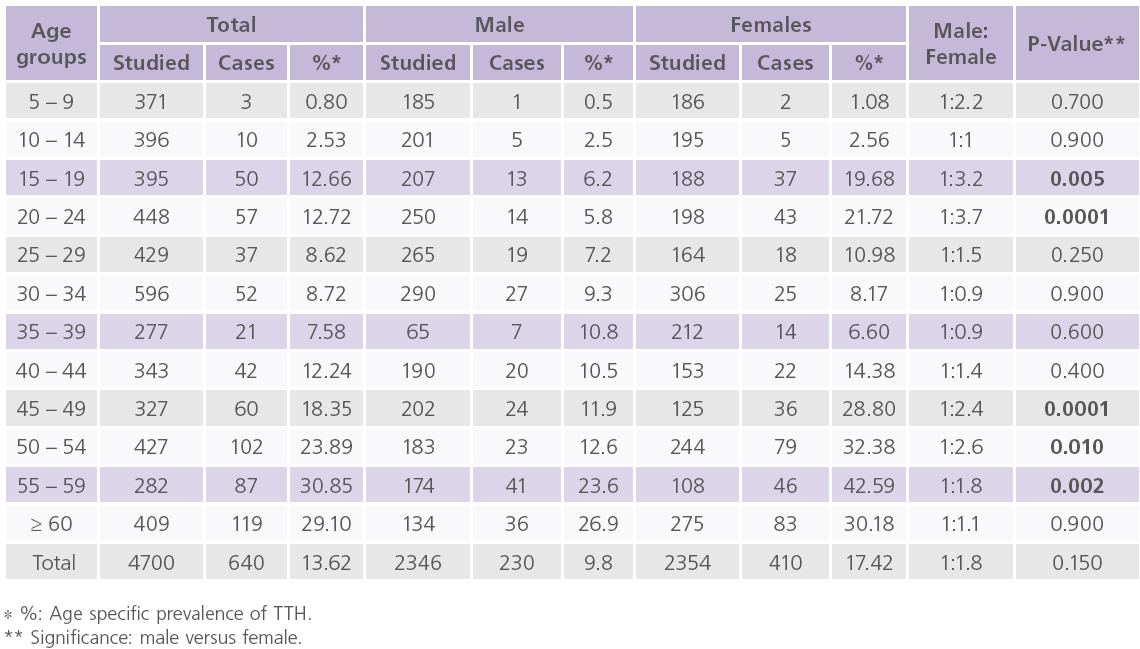
Table 5: Prevalence of TTH in relation to age.
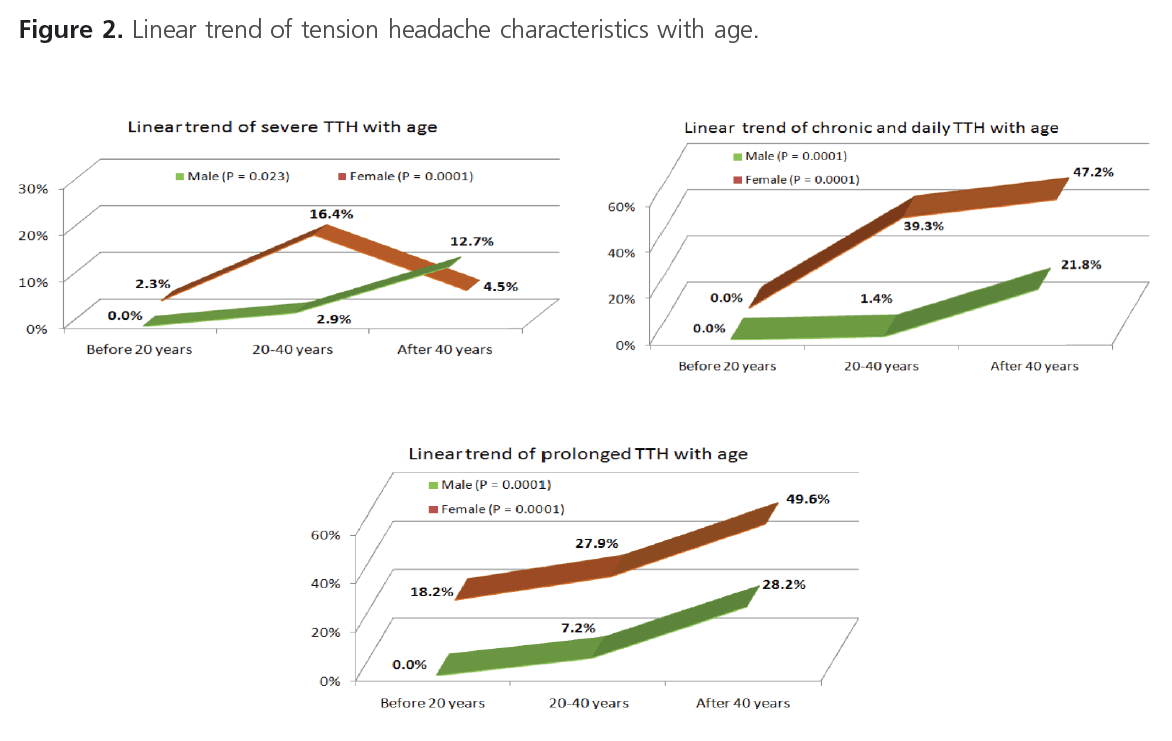
Figure 2 showed the linear trend of TTH characteristics with age. It showed significant change regarding the relationship between age and severity of TTH (males: P = 0.023; females: P = 0.0001). In males, we reported progressive increase of the percentage of severe TTH with age especially after the age of 40 (12.7%), but between the age of 20 and 40 years (16.4%) in females. Significant change with age was identified regarding the relationship with duration of TTH (P = 0.0001). The percentage of prolonged TTH (>1day) was found to be progressively increased with age especially after 40 (males = 28.2%; females = 49.6%). Significant change with age was identified regarding the relationship with frequency of TTH attacks (P = 0.0001). The percentage of chronic and daily TTH was also found to be progressively increased with age particularly after the age of 40 (males = 21.8%; females = 47.2%).
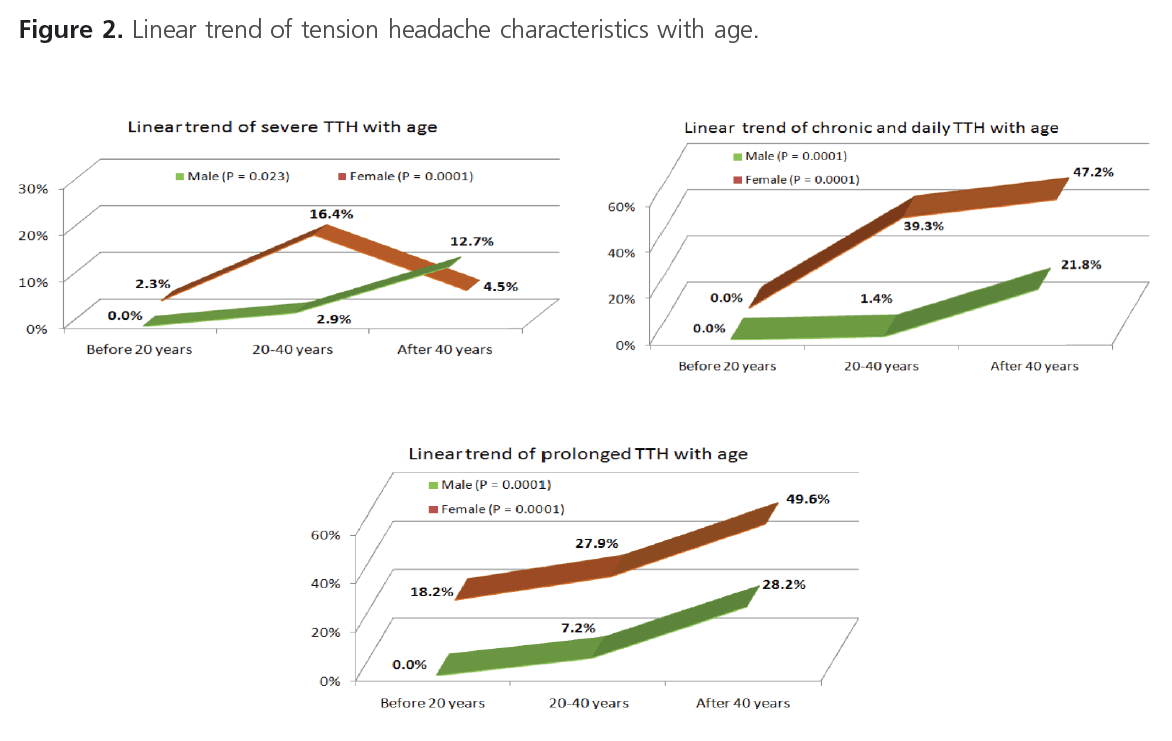
Figure 2: Linear trend of tension headache characteristics with age.
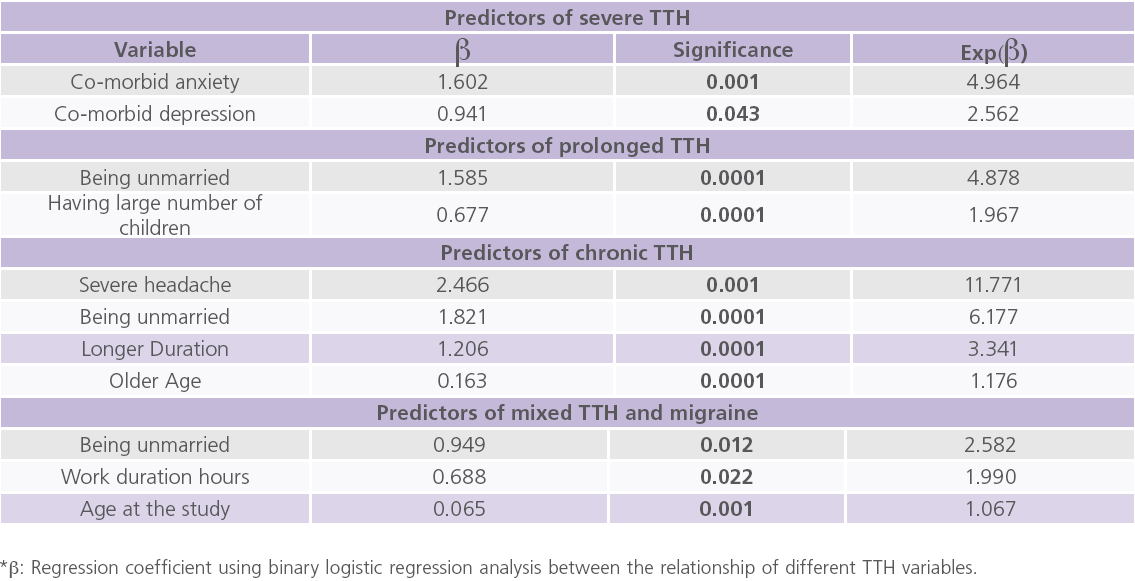
Table 6 showed the predictors related to the variables of TTH. Significant changes were identified between age and a) severity of TTH particularly after the age of 40 (12.7%) in males (P = 0.023) and 20- 40 years (16.4%) in females (P=0.0001), b) duration of TTH particularly after the age of 40 (males = 28.2%; females = 49.6%) (P = 0.0001), and c) frequency of TTH attacks (P = 0.0001). Also the percentage of chronic/daily TTH was also found to be progressively increased with age particularly after the age of 40 (males = 21.8%; females = 47.2%). The odds ratio of having severe TTH was found to be 5 folds more with co-morbid anxiety (Exp β = 4.964), 2.5 folds more with depression (Exp β = 2.562). While prolonged TTH was found to be 5 folds more in unmarried individuals (Exp β = 4.878) and 2 folds more with large number of children (Exp β = 1.967). The odds ratio of having CTTH was found to be 11.8 folds more in individuals with severe attacks (Exp β = 11.771), 6 folds more in unmarried individuals (Exp β = 6.177), 3.3 folds more with prolonged attacks (Exp β = 3.341) and 1.2 folds more in each additional age (Exp β = 1.176).
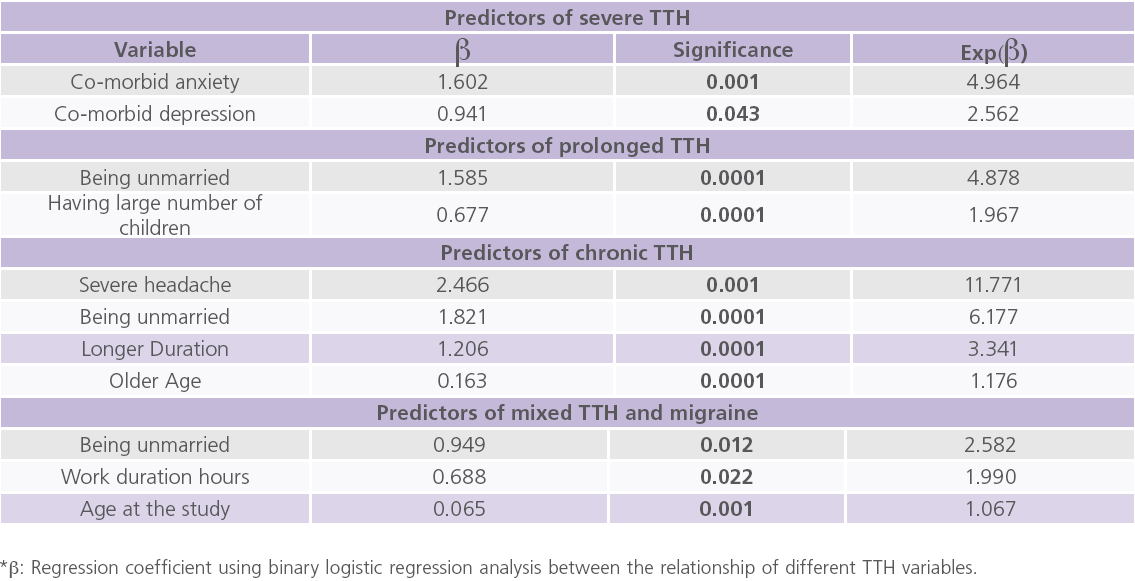
Table 6: Predictors related to variables of TTH.
We reported that the mean of HDI of all individuals with headache was 53.9 ± 18.3. The mean of its emotional component (27.8 ± 10.1) was higher than its functional component (26.4 ± 9) but did not reached a statistically significant level (P = 0.849).
Discussion
This is the first study done in our country on a cohort sample sized population to estimate the prevalence of TTH across various age groups. Although exhausting and time consuming, however, we believe that our door-to-door population-based study (which mainly depends on structured personal interview by a specialist (neurologist) is much more accurate than other related studies; for example: selfreport questionnaires, data collected from medical records, hospital-based studies, etc [1-10, 21, 22, 23, 24, 26-28]. Non-population based studies were observed to be less sensitive to detect risk factors and co-morbidities and are more susceptible to statistical and data bias. This is supported by our finding that the majority of individuals with headache (99.6%) never sought proper medical care for their headache or being self-medicated with OTC headache relieving pills (50.4%). Thus we believe that the work done in this study provided informative observation and accurate prevalence estimation for the epidemiology of primary headaches in general and TTH in particular.
After puberty, TTH was found to be more frequent in females compared to males. In females, it was found to have two peaks; the first was at puberty and throughout marriage (20-25 years) (21.7%) and the second was after menopause between 55-60 years (42.6%). While in males, TTH prevalence had one peak after sixty years old (i.e. age of retirement) (26.9%) [2, 4, 5, 6, 7, 9, 10, 18, 23]. In accordance, in the study of Lyngberg et al. [13] in Denmark, the male to female ratio for TTH was 4:5. In this study, most of males with TTH had 1-3 attack/month (50%) while most of female with TTH had 4-8 attack/ month (41.2%). The relative increased frequency of TTH among females after puberty could be explained by stress of social restrictions in relation to personal freedom, choices, peer relations, marital challenges, emotional factors, depression, anxiety and educational pressures. Winkler et al. [33] in their study on children with headache in rural Tanzania, the authors reported a low 1-year prevalence of TTH (0.04%) in the age group less than 10 years and 1.3% between the ages of 11 and 20 years, while Rasmussen [21] observed that the prevalence of TTH was increased until the 5th decade, with a minor decline with increasing age.
In this study, the majority suffered from mild/moderate (32.66%/59.22%) to moderate headache, while only 8.12% suffered from severe headache. Hilton et al. [34] reported that 33% of individuals with TTH experienced mild attacks, 56% had moderate attacks and 11 % had severe attacks. In this study, the frequency TTH was significantly higher in married males (16.6%) and in unmarried females (23.2%). These findings could be explained by the high burden of family responsibilities that urge many of married males to have multiple jobs. In females, socio-cultural restrains on unmarried females and worries about marriage and increasing age are the main causes of increasing the frequency of TTH. In general, cross-sectional studies observed that the gender difference is not quite as profound for TTH compared to migraine [13, 18, 21]. We also observed an increase in the frequency of TTH with low socioeconomic class (60.94%), and low educational level (51.25%), sleep disturbance and stress [12, 35, 36-38].In this study, family trouble (69.5%) was the most common precipitating factor of TTH. We also reported that the most important predictors of severe attacks were co-morbid anxiety and depression. In this study, we reported that anxiety (31.7%), depression (30.9%) and hypertension (26.8%) were the common co-morbid conditions with TTH [12, 36-38]. Holroyd et al. [39] reported that individuals with CTTH were 3 to 15 times more likely to receive a diagnosis of an anxiety or mood disorder than their matched controls. Matta and Moreira [36] in Brazilian patients with TTH reported that nearly 60% had symptoms of anxiety and 32%, had depression. In the population-based data done by Lyngberg et al. [13], it was observed that TTH but not pure migraine was the main predictor for depression and anxiety after adjustment of TTH. In this study, we reported TTH (17.7%), hypertension (7.5%) and diabetes (5.6%) in family members of individuals with TTH. In accordance, in the study of Russell et al. [40], a family history of headache was found in 40% of individuals with TTH and the firstdegree relatives had a 2.1- to 3.9-folds increased risk of CTTH compared to the general population.
In this study we reported an overall prevalence of primary headache to be 31.11%, among which 13.62% for TTH. In general, the prevalence of TTH was found to vary considerably, across studies. Hagen et al. [2] in Norway reported that the overall 1-year prevalence of non-migrainous headache was 26%. In cross-sectional studies, it was found to range between 9%-78% [41]. Queiroz et al. [42] in Brazil reported that the prevalence of TTH was 22.9%. Katsarava et al. [43] in Georgia, United States of America (USA) reported that the overall 1-year prevalence of TTH was 20.4%. Stovner et al. [10] reported that the prevalence of TTH was 38%. In contrast, in the community-based studies done by the World Health Organization (WHO) [44] in Africa, the prevalence of TTH was estimated to be 1.7%.
In this study, nearly 19.6% of males with TTH had prolonged attacks (more than one day), while in females 20.5% had prolonged attacks and 19.3% their headache become persistent within 4.4 ± 2.7 years. In this study we reported a prevalence of mixed migraine and TTH to be 0.91%. Migraine and TTH commonly coexist, especially in chronic headache, as patient can be diagnosed with both CTTH and chronic migraine [45]. In this study, increasing age particularly after age of 40 (28.2% in males and 49.6% in females), being unmarried, having large number of children were found to be predictors for prolonged TTH. In this study we reported the prevalence of chronic and daily headache to be 10.47%, (7.59% without medication overuse headache and 2.87% with medication overuse headache). We reported transformation of episodic TTH to CTTH in 4.15%, of them 31% had chronic or daily attacks. In a 12-year longitudinal epidemiologic study done in Denmark by Lyngberg et al. [46], the authors reported that 45% of subjects with TTH experienced remission, 39% had unchanged frequent episodic TTH, and 16% had newly developed chronic TTH at follow-up.
Conclusions
TTH is the most common neurological disorder and chronic (TTH) is one of the most neglected and difficult type of headache to treat. The results of this work indicate that TTH is prevalent in our population. Both the episodic or chronic TTH forms does not receive appropriate attention from health authorities, clinical researchers, or industrial pharmacologists, owing to the fact that most people with infrequent or frequent TTH do not consult a doctor but treat themselves with OTC headache relieving pills e.g. non-steroidal anti-inflammatory drugs (NSAIDs). Poor living conditions, financial and social stressors result in increased risk of headache. Moreover lower socioeconomic level causes difficulty to reach an appropriate headache care and the use of self-medication. All result in social isolation, depression, anxiety and poor quality of life and thus increase the prevalence of TTH, mixed TTH and migraine and transformed chronic TTH.
Conflicts of interest
None
1981
References
- Abu-Arafeh, I. Chronic tension-type headache in children and adolescents. Cephalalgia 2001; 21 (8): 830-836.
- Hagen, K., Zwart, J., Vatten, L., Stovner, L., Bovim, G. Prevalence of migraine and non-migrainous headache-head HUNT, a large population-based study. Cephalalgia 2000; 20 (10): 900-906.
- Milovanovic, M., Jarebinski, M., Martinovic, Z. Prevalence of primary headaches in children from Belgrade, Serbia. EJPN 2007; 11 (3): 136- 141.
- Unalp, A., Dirik, E., Kurul, S. Prevalence and clinical findings of migraine and tension-type headache in adolescents. Pediatr Int 2007; 49 (6): 943-949.
- Jensen, R., Stovner, L. Epidemiology and comorbidity of headache. Lancet Neurol 2008; 7 (4): 354-361.
- Alzoubi, K., Mhaidat, N., Azzam, S., Khader, Y., Salem, S., Issaifan, H., Haddadin, R. Prevalence of migraine and tension-type headache among adults in Jordan. J Headache Pain 2009; 10 (4): 265-760.
- Katsarava, Z., Dzagnidze, A., Kukava, M., Mirvelashvili, E., Djibuti, M., Janelidze, M., Jensen, R., Stovner, L., Steiner, T. Primary headache disorders in the Republic of Georgia: Prevalence and risk factors. Neurology 2009; 73 (21): 1796-1803.
- Milde-Busch, A., Heinrich, S., Thomas, S., Kühnlein, A., Radon, K., Straube, A., Bayer, O., von Kries, R. Quality of life in adolescents with headache: Results from a population-based survey. Cephalalgia 2010; 30 (6): 713-721.
- Vukovic, V., Plavec, D., Pavelin, S., Janculjak, D., Ivankovic, M., Demarin, V. Prevalence of migraine, probable migraine and tension-type headache in the Croatian population. Neuroepidemiology 2010; 35 (1): 59-65.
- Stovner, L., Andree, C. Prevalence of headache in Europe: A review for the Eurolight project. J Headache Pain. 2010; 11 (4): 289-299.
- Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004; 24 (1): 9-160.
- Zwart, J., Dyb, G., Hagen, K., Odegard, K., Dahl, A., Bovim, G. Depression and anxiety disorders associated with headache frequency: The Nord-Trondelag Health Study. Eur J Neurol 2003; 10 (2): 147-152.
- Lyngberg, A., Rasmussen, B., Jørgensen, T., Jensen, R. Incidence of primary headache: A Danish epidemiologic follow-up study. Am J Epidemiol. 2005a; 161 (11): 1066-1073.
- Pilarska, E., Olszewska, A. Temperament traits of children with episodic tension-type Headaches. Eur J Paediatr Neurol. 2009; 13 (4): 327-331.
- Ulrich, V., Russell, M., Jensen, R., Olesen, J. A comparison of tensiontype headache in migraineurs and in non-migraineurs: A populationbased study. Pain 1996; 67 (2-3): 501-506.
- Fernández-de-las-Peñas, C., Cleland, JA., Palomeque-del-Cerro, L., Caminero, AB., Guillem-Mesado, A., Jiménez-García, R. Development of a clinical prediction rule for identifying women with tension-type headache who are likely to achieve short-term success with joint mobilization and muscle trigger point therapy. Headache 2011; 51 (2): 246-261.
- Russell, M., Rasmussen, B., Brennum, J. Presentation of a new instrument: The diagnostic headache diary. Cephalalgia 1992; 12 (6): 369-374.
- Stovner, L., Hagen, K., Jensen, R., Katsarava, Z., Lipton, R., Scher, A., Steiner, T., Zwart, J. The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia 2007; 27 (3): 193-210.
- Arnaud, F., Jean S. Tension-type headache: Current research and clinical Management. Lancet Neurol. 2008; 7 (1): 70-83.
- Bendtsen, L. Central sensitization in tension-type headache – possible pathophysiological mechanisms. Cephalalgia 2000; 20 (5): 486-508.
- Rasmussen, B., Jensen, R., Schroll, M., Olesen, J. Epidemiology of headache in a general population. A prevalence study. J Clin Epidemiol. 1991; 44 (11): 1147-1157.
- Laurell, K., Larsson, B., Eeg-Olofsson, O. Prevalence of headache in Swedish schoolchildren, with a focus on tension-type headache. Cephalalgia 2004; 24 (5): 380-388.
- Schwartz, B., Stewart, W., Simon, D. Epidemiology of tension-type headache. JAMA 1998; 279 (5): 381-383.
- Waldie, K., Poulton, R. Physical and psychological correlates of primary headache in young adulthood: A 26-year longitudinal study. J Neurol Neurosurg Psychiatry 2002; 72 (1): 86-92.
- Buchgreitz, L., Lyngberg, A., Bendtsen, L., Jensen, R. Frequency of headache is related to sensitization: A population study. Pain 2006; 123 (1-2): 19-27.
- Benamer, H., Deleu, D., Grosset, D. Epidemiology of headache in Arab countries. The Journal of Headache and Pain 2010; 11 (1): 1-3.
- Russell, M. Tension-type headache in 40-year-olds: A Danish populationbased sample of 4000. J Headache Pain 2005; 6 (6): 441-447.
- Gassmann, J., Morris, L., Heinrich, M., Kröner-Herwig, B. One-year course of paediatric headache in children and adolescents aged 8-15 years. Cephalalgia 2008; 28 (11): 1154-1162.
- Jacobson, G.P., Ramadan, N.M., Aggarwal, S.K., Newman, C.W. The Henry Ford Hospital Headache Disability Inventory (HDI). Neurology 1994; 44 (5): 837-842.
- Abdel-Tawab, M. Socioeconomic scale for family, revised edition. M.D. thesis in educational basics, Faculty of Education, Assiut University 1998; 3: 32-55.
- Winkle, A., Stelzhammer, B., Kerschbaumsteiner, K. The prevalence of headache with emphasis on tension-type headache in rural Tanzania: A community-based study. Cephalalgia 2009; 29 (12): 1317-1325.
- Hilton, M., Roberta, P., Simone, O., Carlos, A., José, G. Effect of episodic tension-type headache on the health-related quality of life in employees of a Brazilian public hospital. Arq Neuropsiquiatr. 2004; 62 (3-B): 769-773.
- Jennum, P., Jensen, R. Sleep and headache. Sleep Med Rev. 2002; 6 (4): 471-479.
- Matta, A., Moreira, P. Depressive symptoms and anxiety in patients with chronic and episodic tension-type headache. Arq Neuropsiquiatr. 2003; 61 (4): 991-994.
- Arruda, M., Guidetti, V., Galli, F. Frequent headaches in the preadolescent pediatric population: A population-based study. Neurology 2010; 74 (11): 903-908.
- Sara, B., Renata, A., Marcella, M., Roberto, Z., Marco, C. Chronic Tension- Type Headache in Adolescents. Clinical and Psychological Characteristics Analyzed Through Self-and Parent-Report Questionnaires. Journal of Pediatric Psychology 2009; 34 (7): 697-706.
- Holroyd, K., Stensland, M., Lipchik, G., Hill, K., O’Donnell, F., Cordingley, G. Psychosocial correlates and impact of chronic tension type headaches. Headache 2000; 40 (1): 3-16.
- Russell, M., Ostergaard, S., Bendtsen, L., Olesen, J. Familial occurrence of chronic tension-type headache. Cephalalgia 1999; 19 (4): 207-210.
- Jensen, R. Diagnosis, epidemiology, and impact of tension-type headache. Curr Pain Headache Rep. 2003; 7 (6): 455-459.
- Queiroz, L., Barea, L., Blank., N. An epidemiological study of headache in Florianopolis, Brazil. Cephalalgia 2006; 26 (2): 122-127.
- Katsarava, Z., Jensen, R. Medication-overuse headache: Where are we now? Curr Opin Neurol. 2007; 20 (3): 326-330.
- World Health Organization, Headache Disorders. Fact sheet N_277, March 2004.
- Headache Classification Committee, Olesen, J., Bousser, M.G., Diener, H.C., Dodick, D., First, M., Goadsby, P.J., Göbel, H., Lainez, M.J., Lance, J.W., Lipton, R.B., Nappi, G., Sakai, F., Schoenen, J., Silberstein, S.D., Steiner, T.J. New appendix criteria open for a broader concept of chronic migraine. Cephalalgia 2006; 26 (6): 742-746
- Lyngberg, A., Rasmussen, B., Jørgensen, T., Jensen, R. Prognosis of migraine and tension-type headache: A population-based follow-up study. Neurology 2005; 65 (4): 580-585.