Keywords
Diabetes; gluconeogenesis; ketoacidosis
Introduction
Hyperglycemic diabetic emergencies include diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state [1]. Management of these conditions requires a careful hydration strategy to restore volume and improve perfusion, intravenous insulin therapy, and electrolyte monitoring [1].
DKA diagnostic criteria include presence of blood glucose > 250 mg/dL, arterial pH ≤ 7.30, bicarbonate level ≤ 18 mEq/L, and adjusted for albumin anion gap of more than 10–12 [2]. Positive serum and urine ketones may further support the diagnosis of DKA [2]. DKA was a fatal entity before the discovery of insulin in 1920.
Euglycemic DKA (euDKA), defined as DKA without marked hyperglycemia, is classically considered rare but this is perhaps a result of under-recognition and underreporting [3]. EuDKA is thought to be facilitated by factors such as partial treatment of DKA, food restriction, alcohol intake, and inhibition of gluconeogenesis [3].
Sodium glucose co-transporter type 2 (SGLT2) inhibitors, such as dapagliflozin, canagliflozin, and empagliflozin, decrease renal glucose reabsorption, which results in enhanced urinary glucose excretion and subsequent reductions in plasma glucose and glycosylated hemoglobin concentrations [4]. Several metaanalyses have demonstrated a significant improvement of glycemic control in patients with T2DM who were treated with SGLT2 inhibitors [4]. SGLT2 inhibitors are nowadays used as a novel add-on therapy in type II and in type I diabetes [4].
SGLT2 inhibitors have been recently described to be associated with euDKA more so in type I diabetes. Here, we describe a case of a poorly nourished patient with diabetes type II, on SGLT 2 inhibitor who developed euDKA. We also review the literature on euDKA, including its latest association with SGLT2 inhibitors.
Case Presentation
Mr. J.H. is a 59 year old man with Diabetes Mellitus type II (DMII) for 10 years, maintained on Sitagliptin and Metformin combination 50/1000 twice daily, Glimeperide 4 mg daily and Canagliflozin 100 mg daily that was added 1 month ago for poorly controlled glycemia reflected by an HbA1C of 10%.
He denied hyperglycemic and hypoglycemic symptoms. He does not take his sugar regularly at home and does not report any documented micro or macro-vascular complication. One month prior to initiating Canagliflozin, he started complaining of early satiety, decrease oral intake, abdominal pain and distension as well as 10 kilograms unintentional weight loss requiring reduction in his oral hypoglycemic agents over the last 2 weeks and admission through the emergency department (ED).
Upon presentation to the ED, he looked cachectic with prominent muscle wasting. His blood glucose level was 256 mg/dl (dropped in 1 hour to 180 mg/dl with IV fluids only). His labs showed a measured serum osmolality of 277 mosm/kg and serum sodium of 132 mmol/L. Urine ketones were positive and serum ketones were 44.2 mg/dl.
His arterial blood gases showed a PH of 7.38, PCO2 of 29 mmHg and PO2 of 79 mmHg and his serum bicarbonate was 14 mmol/L. His anion gap (AG) was 23 (corrected to Albumin 35 g/ L= 24.25): pure high anion gap metabolic acidosis compensated by respiratory alkalosis with Δanion gap/ Δbicarbonate of 1.4. He also had significant leukocytosis (19200) and was admitted for IV antibiotics and workup of ascites.
In-Hospital Management
The ketonemia was considered due to starvation and not diabetic ketoacidosis because blood glucose was mostly less than 200. At first, he only received IV fluids.
The next day, bicarbonate improved to 16mmol/L with AG of 20 and ketones of 36,8 mg/dl.
On day 3, bicarbonate was 19mmol/L with an AG of 19.
On day 4, despite IV hydration and acceptable oral intake post ascitic fluid drainage, bicarbonate dropped to 16 mmol/L, and AG was 27, and the glucose was always below 200 mg/dl.
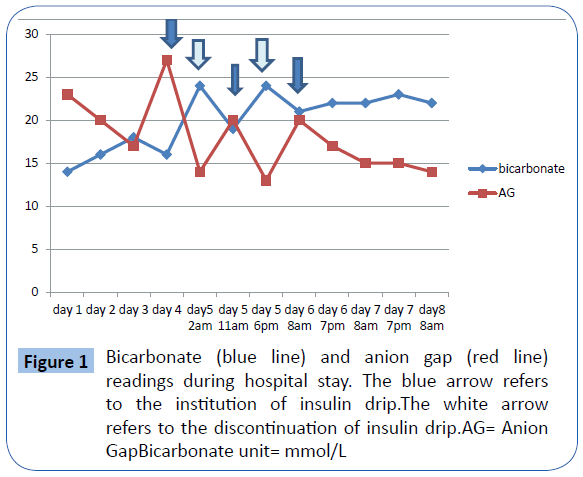
At that point, in view of the worsening acidosis and AG despite adequate hydration, he was considered to have possible euDKA exacerbated by decreased PO intake and Canagliflozin. He was started then on IV Insulin drip, and repeat labs showed dramatic improvement in AG [14] and bicarbonate (24 mmol/L) after 6h of insulin drip and IV glucose (Figure 1).
The next day, because of normal bicarbonate and lower AG [14], it was decided to stop insulin drip and to switch to the subcutaneous form. However, there was a relapse in acidosis (19 mmol/L) and AG [20], so insulin drip was resumed (Figure 1).
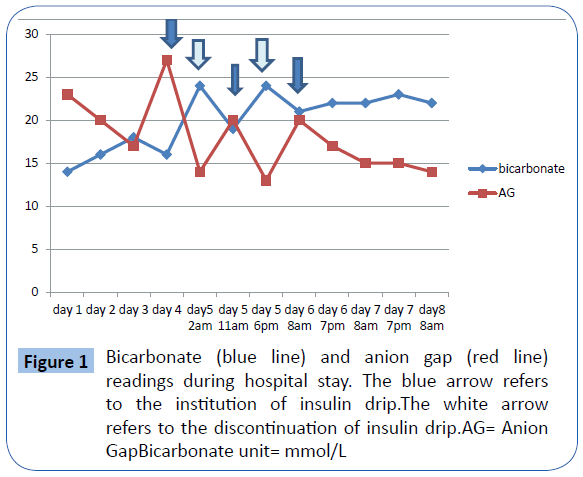
Figure 1: Bicarbonate (blue line) and anion gap (red line) readings during hospital stay. The blue arrow refers to the institution of insulin drip.The white arrow refers to the discontinuation of insulin drip.AG= Anion GapBicarbonate unit= mmol/L
The same scenario re-occurred with improvement of the previous parameters after reinstitution of insulin drip (Figure 1).
However, after 48 hours of insulin drip, patient had to leave the hospital for personal reasons. He was discharged off Canagliflozin.
Workup of Ascites showed peritoneal metastasis, and gastric adenocarcinoma as a possible primary malignancy.
Discussion
Illness, a reduction in food intake and glycosuria lead to the development of euDKA in the reported patient.
In fact, Dr. J.F. Munro et al. first described euDKA in 1973 postulating that the pathogenesis lies in greater urinary loss of glucose [5]. They observed that some of the identified patients have a massive urinary loss of sugar and a greater tendency to a low renal threshold to glucose than in others [5].
Although euDKA is rare, low caloric intake, starvation, persistent vomiting, and pregnancy can be contributory factors in its development [6]. Moreover, euDKA is also reported in insulindependent diabetics with depression, alcoholics, glycogen storage diseases, and chronic liver disease apart from pregnant cases [7].
Burge et al.in 1992 studied the effect of a 32-hour fast on the rate of metabolic deterioration in 10 healthy subjects with type I diabetes mellitus and concluded that a fast of moderate duration, predisposes patients with type I diabetes to euglycemic ketoacidosis during periods of insulin deficiency [8]. Furthermore, decreased rates of hepatic glucose production are responsible for the lower plasma glucose values observed during a fast [8]. Moreover, the accelerated development of ketosis may be attributable to the effects of elevated levels of glucagon and/or catecholamines on lipolysis [8].
In 2008, Joseph et al. reported the case of a type I diabetes patient presenting with euDKA secondary to anorexia and starvation from underlying depression [9].
EuDKA is mainly described in type I diabetes. In fact, Thawabi et al. described in June 2015 two cases of euDKA in otherwise healthy patients with type 1 diabetes mellitus who had decreased carbohydrate intake in the presence of adequate hydration and a degree of insulin intake. Triggers were Bartholin gland abscess and pancreatitis [10].
EuDKA can also be the presenting feature of unrecognized diabetes.
Prater et al. in 2015 presented the case of a 36 year-old patient with a known history of alcoholism admitted with metabolic acidosis and acute pancreatitis and not known to have diabetes. She was subsequently diagnosed with euDKA and improved upon institution of the treatment protocol [11]. Similarly, and to emphasize on the importance of fasting as a trigger for euDKA, Bas et al. reported in 2014 a case of euglycemic DKA that resulted from long-lasting starvation during Ramadan fasting in a newly diagnosed 14-year-old male patient [7].
In the literature, pregnancy was found to be associated with euDKA [type I, II, gestational diabetes or previously undiagnosed diabetes and precipitated by starvation] especially in the second and third trimesters. The occurrence of DKA in pregnancy is an urgent complication that compromises both the fetus and the mother, with a perinatal mortality rate of approximately 35% [12].
The reduction in buffering capacity, the relative insulin resistance, the enhanced lipolysis, the elevated free fatty acids, the ketogenesis, and the production of placental lactogen, progesterone, cortisol, and insulinase, all contribute to a diabetogenic state and predispose to the development of DKA [12].
On the other hand, the normoglycemia in the pregnant patient with DKA seems to have several plausible explanations including increased metabolic rate and therefore risk of ketosis, glycosuria from increased GFR unmatched with increased tubular absorption, increased glucose utilization and physiologic hemodilution [12].
Development of euDKA in patients with Duchenne muscle dystrophy was also reported in patients with type I and II diabetes [13,14]. Incriminated factors were reduced muscle mass, increased body fat, and starvation [14].
Throughout the years, euDKA was mostly associated with type I diabetes. With the advent of SGLT2 inhibitors promoting glycosuria, more cases of type II diabetes are presenting with euDKA.
Peters et al.in July 2015 described nine patients on SGLT2 inhibitors who developed euDKA [seven type I and two with type II diabetes] [3]. This is the first case series relating this association. Prior to that, Hayami et al. reported the case of a diabetic woman with Prader–Willi syndrome and type II diabetes who developed severe ketoacidosis caused by SGLT2 inhibitor, during a strict lowcarbohydrate diet [15,16]. St Hilaire et al. also reported a man with type I diabetes and euDKA who was taking canagliflozin possibly with insulin.
Increased renal clearance of glucose mediated by the SGLT- 2 inhibitor leads to deceivingly low blood glucose levels in the setting of illness, and the reduced insulin doses at a time of heightened insulin resistance promotes ketosis resulting in euDKA [3]. In addition, the diuretic effect of SGLT2 inhibitors worsens the volume depletion state of patients with DKA. Hypovolemia drives elevations in glucagon, cortisol, and epinephrine, which further increase insulin resistance, lipolysis, and ketogenesis [3].
Conclusion
We believe that this case adds to the scarce reported cases of euDKA in type 2 diabetes on SGLT2 inhibitors further raising awareness for close monitoring of those patients when in critical illness, keeping an eye on urine and blood ketone levels. Therefore, in diabetic patients on SGLT2 inhibitors with poor oral intake, acidosis should raise a red flag for euDKA.
7707
References
- Beltran G (2014) Diabetic emergencies: new strategies for an old disease. Emerg Med Pract 16: 1-19.
- Rosival V1 (2014) Management of adult diabetic ketoacidosis. Diabetes MetabSyndrObes 7: 571-573.
- Peters AL, Buschur EO, Buse JB, Cohan P, Diner JC, et al. (2015) Euglycemic Diabetic Ketoacidosis: A Potential Complication of Treatment With Sodium-Glucose Cotransporter 2 Inhibition. Diabetes Care.
- Nauck MA (2014) Update on developments with SGLT2 inhibitors in the management of type 2 diabetes. Drug Des DevelTher 8: 1335-1380.
- Munro JF, Campbell IW, McCuish AC, Duncan LJ (1973) Euglycaemic diabetic ketoacidosis. Br Med J 2: 578-580.
- Akbay S, Yel A,YildirimerÜ, Can S, Dündar B(2013) Diabetic ketoacidosis presenting with pseudonormoglycemia in a 15-year-old girl with type 1 diabetes mellitus. J Clin Res PediatrEndocrinol 5: 133-135.
- Bas VN, Uytun S, Torun YA (2015) Diabetic euglycemic ketoacidosis in newly diagnosed type 1 diabetes mellitus during Ramadan fasting. J PediatrEndocrinolMetab. 28:333-335.
- Burge MR, Hardy KJ, Schade DS (1993) Short-term fasting is a mechanism for the development of euglycemic ketoacidosis during periods of insulin deficiency. J ClinEndocrinolMetab 76: 1192-1198.
- Joseph F, Anderson L, Goenka N, Vora J (2009) Starvation-induced true diabetic euglycemic ketoacidosis in severe depression. J Gen Intern Med 24: 129-131.
- Thawabi M,Studyvin S1 (2015) Euglycemic Diabetic Ketoacidosis, a Misleading Presentation of Diabetic Ketoacidosis. N Am J Med Sci 7: 291-294.
- Prater J,Chaiban J (2014) Euglycemic Diabetic Ketoacidosis with Acute Pancreatitis in a Patient Not Known to Have Diabetes. EndocrPract.
- Guo RX, Yang LZ, Li LX, Zhao XP (2008) Diabetic ketoacidosis in pregnancy tends to occur at lower blood glucose levels: case-control study and a case report of euglycemic diabetic ketoacidosis in pregnancy. J ObstetGynaecol Res 34:324-330.
- Braithwaite SS, Lange CF, Klamut M (1987) Euglycemic diabetic ketoacidosis in Duchenne's muscular dystrophy. Diabetes Care 10: 540-541.
- Lee SH, Park JH, Hong MK (2011) True euglycemic diabetic ketoacidosis in a person with type 2 diabetes and Duchenne muscular dystrophy. Diabetes Res ClinPract 92:e7-e8.
- Hayami T, Kato Y, Kamiya H (2015) Case of ketoacidosis by a sodium-glucose cotransporter2 inhibitor in a diabetic patient with a lowcarbohydrate diet. J Diabetes 6: 587-590.
- St Hilaire R, Costello H (2014) Prescriber beware: report of adverse effect of sodium-glucose cotransporter 2 inhibitor use in a patient with contraindication. Am J Emerg Med.