Pondy Angele Hermine1,2, Djomgoue Molom Rodrigue3, Ngo Nonga Bernadette4* and Koki Ndombo Paul1,2
1 Faculty of Medicine and Biomedical Sciences, Department of Pediatrics, University of Yaounde, Cameroon
2 Mother and Child Center of the Chantal Biya‘s Foundation in Yaounde, Cameroon
3 Institute of Technology and Medical Sciences of Yaounde, Cameroon
4 Faculty of Medicine and Biomedical sciences, Department of Surgery and Specialties, University of Yaounde, Cameroon
*Corresponding Author:
Ngo Nonga Bernadette
Faculty of Medicine and Biomedical Sciences, Department of Surgery and Specialties, University of Yaounde, Cameroon.
Tel: +237 2 22 22 13 20
E-mail: ngonongab@yahoo.com
Received Date: August 08, 2016; Accepted Date: August 29, 2016; Published Date: August 31, 2016
Citation: Hermine PA, Rodrigue DM, Bernadette NN, Paul KN (2018) Evaluation of the Response to Chemotherapy in the Treatment of Hodgkin’s Disease at the Mother and Child Center of the Chantal Biya’s Foundation in Yaounde, Cameroon. Arch Cancer Res. Vol.6 No.1:2 doi: 10.21767/2254-6081.100168
Keywords
Hodgkin’s disease; Child; Treatment; Evaluation; Chemotherapy
Introduction
Hodgkin's disease (HD) is a malignant disease of the lymphatic tissue mainly affecting the lymph nodes and characterized by a very particular cell, called the Reed Sternberg cell (RSC) [1-3]. It is a pathology of the adolescent and the young adult. The annual incidence is estimated to be between 3 to 6 new cases per million children aged 0 to 15 years [4-6]. In developing countries, clinical, epidemiological and therapeutic data are poorly known, and many studies have shown a predominance of the mixed cellular form most often associated with a worse prognosis [5,7]. In Cameroon, Hodgkin's disease is not uncommon, so the authors have reported 70 cases of HD over a period of 11 years (1979-1989), or almost 6 cases/year [8]. Modern therapies, including those combining radiotherapy and chemotherapy, have significantly improved the prognosis of the condition in developed countries. In Cameroon, the lack of a suitable protocol in children and the difficulties or even the impossibility to access radiotherapy are the cause of the death of many children for lack of appropriate treatment. To treat children with HD, we have used the COPP/ABV hybrid protocol without radiotherapy. Thus, the purpose of our study was to evaluate the response to treatment of children with HD by this protocol.
Materials and Methods
This is the analysis of data from a child cohort monitored at the CME/FCB for HD. The study was carried out from 1st January 2007 to 31st December 2016. In all children, the diagnosis was confirmed by lymph node biopsy and the histological type was determined according to the WHO classification [9,10]. A pre-therapeutic assessment included a physical examination, laboratory tests (complete blood count, erythrocyte sedimentation rate and lactate dehydrogenase assay) and radiological examinations (chest x-ray and abdominopelvic ultrasound). The disease was classified according to the classification of Ann Arbor.
Initial staging and medications
The Ann Arbor was used for staging patients based on the absence (A) or presence (B) of: Fever >38°C for at least one week, weight loss (>10% body weight during the last 6 months) Night sweats (requiring the patient to change or waking him her at night). Thus, the patients were stratified into 2 prognostic groups according to the Ann Arbor classification: The favourable group=G1 (stage I and IIA, and mediastino-thoracic index <0.45 and lymph node’s tumor volume <6 cm and no contiguous lesion). Unfavourable group=G2: all patients not included in the favourable group: (IIB, III, IV with large mediastinum with mediastino-thoracic index superior or equal to 0.45 or adenopathy’s volume superior or equal to 6 cm or visceral involvements).
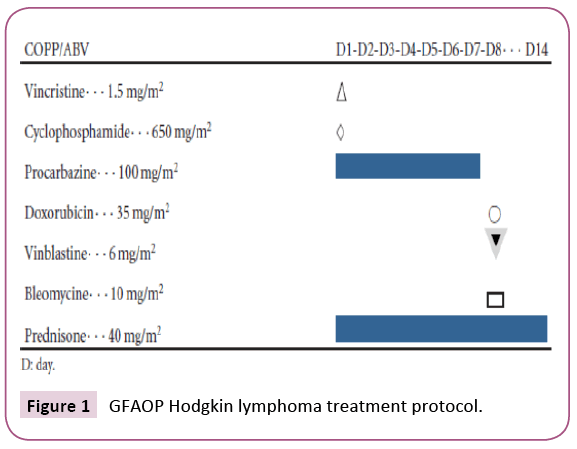
At the end of this stratification the patients were treated according to the following regimen: Vincristine 1.5 mg/m² (max 2 mg) on the first day, Cyclophosphamide 650 mg/m² on the first day, Procarbazine 100 mg/m² from 1st to 7th day, Adriamycin 35 mg/m²; The 8th day, Vinblastine 6 mg/m² on the 8th day, Bleomycin 10 mg/m² on the 8th day, Prednisone 40 mg/m² from the 1st to the 14th day.
Premedication (25-50 mg of hydrocortisone hemisuccinate) was administered slowly intravenously before bleomycin cures. The cures were done every 28 days shown in Figure 1.
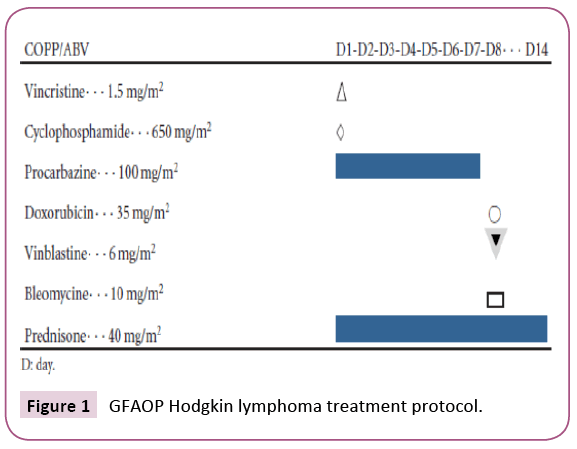
Figure 1: GFAOP Hodgkin lymphoma treatment protocol.
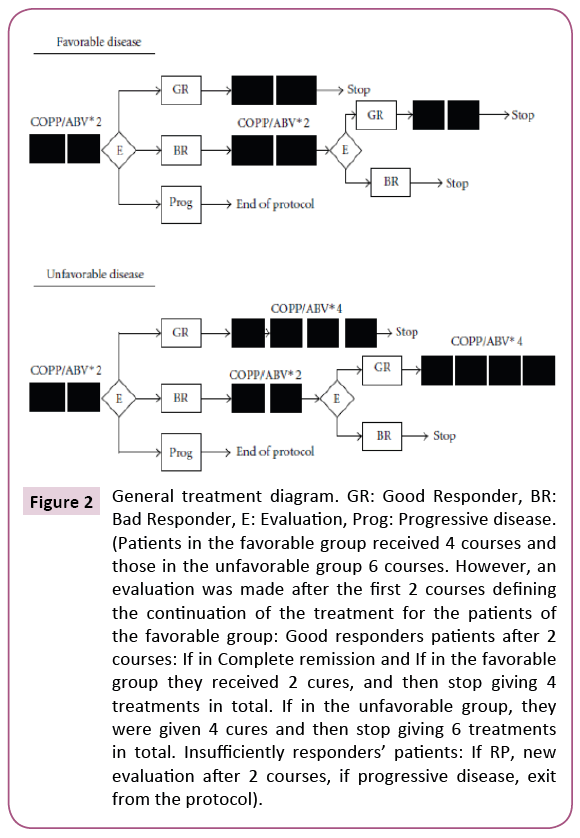
Evaluation of the response
It was done according to the following criteria: A good response was defined as a clinical, biological and radiological response ranging from 70% to 100% (complete remission), a partial response was defined as a response between 50% and 70%. Failure was defined as either a lack of response or a response of less than 50%, or a clinical, biological or radiological progression of the disease. Survival was assessed using the Kaplan-Meier method from the date of initiation of treatment to the date of last consultation (Figure 2).
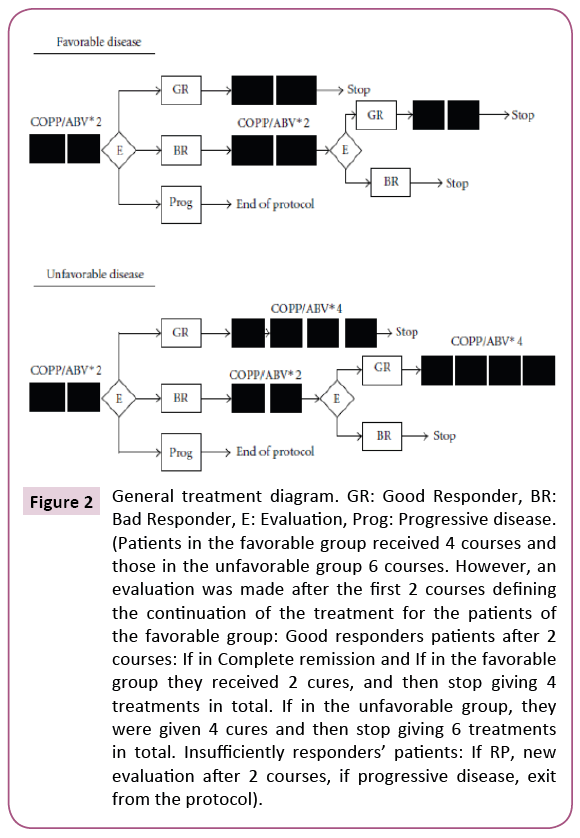
Figure 2: General treatment diagram. GR: Good Responder, BR: Bad Responder, E: Evaluation, Prog: Progressive disease. (Patients in the favorable group received 4 courses and those in the unfavorable group 6 courses. However, an evaluation was made after the first 2 courses defining the continuation of the treatment for the patients of the favorable group: Good responders patients after 2 courses: If in Complete remission and If in the favorable group they received 2 cures, and then stop giving 4 treatments in total. If in the unfavorable group, they were given 4 cures and then stop giving 6 treatments in total. Insufficiently responders’ patients: If RP, new evaluation after 2 courses, if progressive disease, exit from the protocol).
The study was approved by the institutional committee on ethics and research of the University of Douala, the National Ethics committee of Cameroon and the administrative authorities of the Center for the Mother and Child Center of the Chantal Biya Foundation.
Results
Population characteristics
Out of a total of 1325 cases of childhood cancers at CME-FCB during the study period, 26 children had Hodgkin's disease, giving a hospital’s prevalence of 1.96%. The mean age of patients at diagnosis was 11.5 years with extremes of 7 and 16 years. The most represented age group was 10 to 14 years (57.7%, 15/26). The sex ratio 1.88 (17 boys and 9 girls). The mean consultation time was 11.05 months with extremes of 1 and 48 months. Eleven patients (42.3%) consulted after more than 12 months after the beginning of symptoms. The most common presenting clinical sign was the presence of peripheral adenopathies of the cervical region in 20 patients (76.9%). At pathology, the scleronodular, mixed cellular and the lymphocyte-rich forms were found in the respective proportions of 38.4%, 34.6% and 27%. Biologically, the erythrocyte sedimentation rate was done in 12 patients and revealed a rise of more than 30 mm at the first hour in 11 of them and anemia (hemoglobin less than 12 g/dl) was observed in 11 children. Bone marrow biopsy was performed in 3 patients. The chest radiograph showed enlargement of the mediastinum in 8 patients out of 17 who did the exam (47.05%). Abdominal Ultrasound (of the abdomen was done in 20 patients; it revealed retroperitoneal adenopathies in 13 patients, splenomegaly in 10 patients and hepatomegaly in 12 of them. After the physical, biological and radiological work-up, 7/26 (26.9%) patients had localized Hodgkin's disease (two stage I and five stage II) and 19/26 (73.67%) patients had advanced stage III and stage IV disease at the time of diagnosis. Of these, 16 patients had clinical signs of progression shown in Table 1.
| Variables |
Number |
(%) |
| Age |
| 5-9 years |
7 |
26.90% |
| 10-14 years |
15 |
57.70% |
| >14 years |
4 |
15.40% |
| Gender |
| Male |
17 |
65.40% |
| Female |
9 |
34.60% |
| Adenopathy Localisation |
| Cervical |
20 |
76.90% |
| Inguinal |
11 |
42.30% |
| Axillar |
9 |
34.60% |
| Maxillar |
5 |
19.20% |
| Extra-ganglionicsigns |
| Splenomegaly |
14 |
53.80% |
| Hepatomegaly |
13 |
50.00% |
| General state alteration |
16 |
61.53% |
| Stage and sign of disease progression |
| I A |
2 |
7.69% |
| II A |
3 |
11.53% |
| II B |
2 |
7.69% |
| III A |
4 |
19.23% |
| III B |
13 |
50% |
| IV B |
1 |
3.86% |
| Fever (n=16) |
16 |
100.00% |
| Weightloss (n=16) |
12 |
75.00% |
| Sweats (n=16) |
8 |
50.00% |
| Histological type ganglionicsigns |
| Lymphocyte rich |
10 |
38.40% |
| Scleronodular |
9 |
34.60% |
| Mix cellularity |
7 |
27% |
| A : Absence of signs of improvement ;B:Presence of signs of improvement |
Table 1: Characteristics of the population.
Response to treatment
Of the 7 patients with localized Hodgkin's disease (stages I-II), 6 cases were in complete remission and 1 case was in partial remission. While in those with advanced stages 73.1% (19/26) (stages III-IV) 12 cases were in complete remission, 2 cases relapsed, 3 cases died, and 2 cases were lost to follow-up.
Distribution of patients by causes of death
Analysis of the causes of death revealed greater imputability to the natural course of the disease in 2 patients out of 3 (66.70%), while the other causes of death were unrelated to the disease or its treatment in one case (33.3%). The later died secondary to renal failure prior to diagnosis of the 3 patients who died, one had relapse meanwhile, the other two never had remission. Social factors: Common reasons for delayed time from diagnosis to treatment
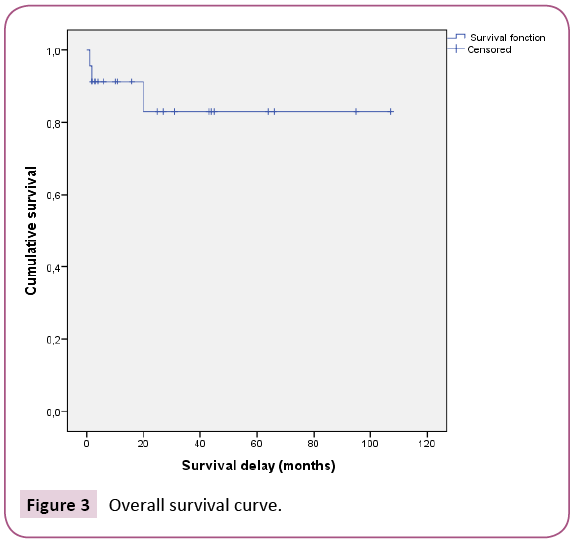
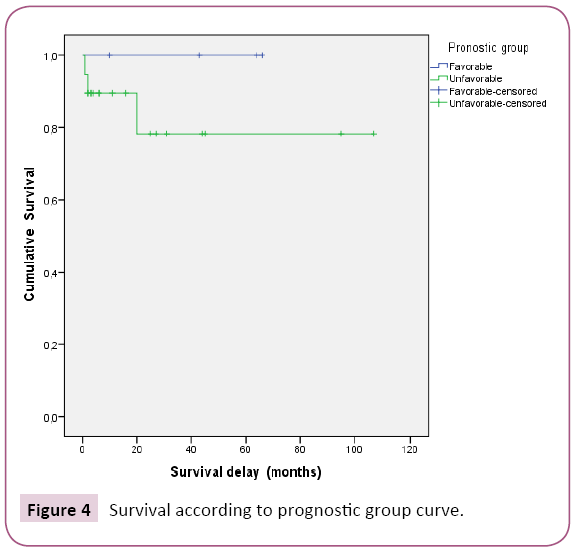
Study of survival and prognostic factors
The five-year overall survival rate was estimated to be 82% (Figure 3). This five-year overall survival rate was 100% in patients ranked prognosis favourable to initiation of treatment and 78% in patients ranked prognosis Unfavourable (Figure 4). The analysis of survival according to age, sex, histological type, stage, clinical and biological signs of evolution did not find any significant impact on these parameters on overall survival. However, advanced stages were associated with greater mortality.
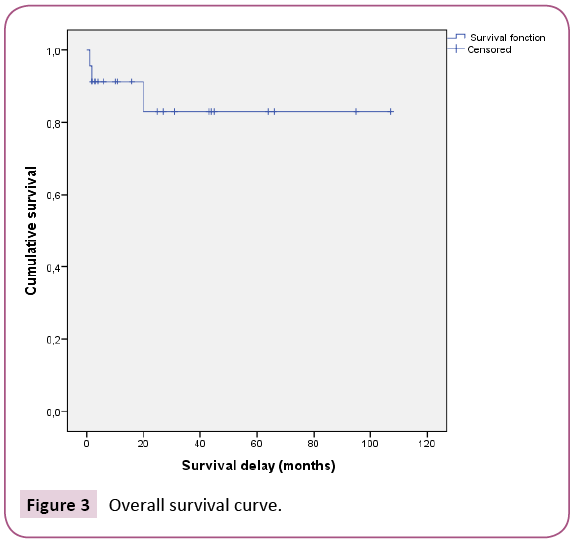
Figure 3: Overall survival curve.
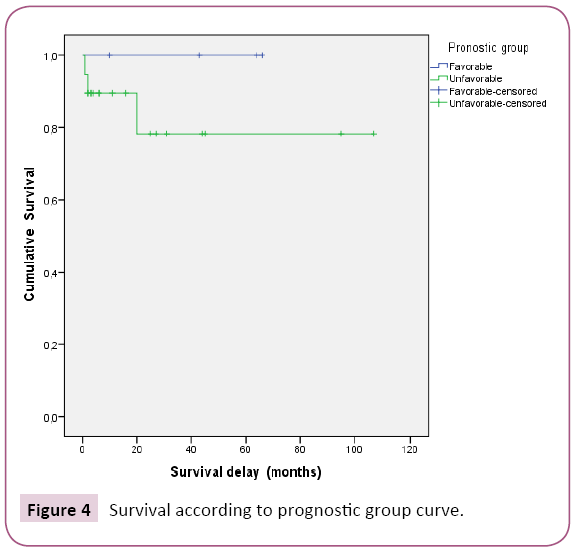
Figure 4: Survival according to prognostic group curve.
Discussion
The incidence of HD in Cameroon and especially in its pediatric form is not well known due to the scarcity of available data. Thus, during our study period at the MCC/CBF, we collected 26 cases of HD from 1325 cases of all pediatric cancers, giving a prevalence of 1.96%. Similar prevalence has been found in other developing countries [11,12]. However, this may be under-estimated, because of the unfavourable socio-economic context, which limits access to the public health system in general and to the country's only pediatric oncology unit.
The average age of our patients at the time of diagnosis was 11.5 years with extremes of 7 and 16 years, the age group of 10-14 years was the most represented 57.70%. These data are broadly similar in the series of developing countries [12-14] and lower than those reported by the western series, most often over 13 years. In 2002, Donaldson et al found an average age of 13 years in the USA [15-17]. We noted a male predominance with a sex ratio of 1.87 less than those reported by Togo et al in Mali in 2011, Khanfir et al. in Tunisia in 2007, who found a sex ratio of 6 and 3.6 respectively [12,18]. The advanced stages were predominant (73.67%). Patients in stages III and IV are more common in developing countries; their frequency may exceed 70%. Conversely, in Western countries, predominance of localized forms (stages I-II) is more common, the frequency of which often exceeds 60% [14,19]. This predominance of the advanced stages in our series is due to missed diagnosis: The patients being most often treated for another pathology, usually tuberculosis. The high frequency of advanced stages may as well be due to the wandering of these patients in hospitals and the delay of diagnosis due to financial constraints.
Histologically, the scleronodular, mixed cellular and lymphocyterich forms were found in the respective proportions of 38.4%, 34.6% and 27%. With a non-significant difference. However, it should be noted that the predominant histological type varies from country to country. Indeed, in western countries the scleronodular type is predominant with a frequency exceeding 60%. But in developing countries, the mixed cellular type is the most frequent (50% to 75% of the cases) [12,20-22]. However, due to the small size of our sample, we cannot draw any conclusions about the distribution of the histological types.
Chemotherapy was the only therapeutic modality. Thus, at the end of treatment, the complete remission rate was 61%, with 4% partial remission and 9% relapse 13% death and abandonment.
In our series, the overall 5-year survival rate for all stages was 82% with an average survival time of 90.6 months. This rate is close to those found in the literature, which ranged between 80 and 90% [18,19,23-25]. However, the survival rate varied according to the prognostic group. Thus, the 5-year survival of patients in the favourable group was 100%. Whereas the unfavourable group was 78%. Results like those of Baez et al. in Nicaragua in 1997, which found a three-year survival rate of 100% for stages (I, II and IIIa) and 74.9% for stages (IIIb and IV).
We deplored 3 cases of death due in two cases to the tumor progression and in one case to renal insufficiency. Deaths were associated with discontinuation of treatment due to multiple factors, including those impeding access to the treatment center.
Conclusion
Hodgkin's disease is a chemo-sensitive and radiosensitive disease whose management according to international recommendations is based on the combination of radio and poly chemotherapy. However, the virtually non-existent functional radiotherapy unit in our context limits the therapeutic options to chemotherapy alone. Thus, at the end of this work, we found a good feasibility of the COPP-ABV protocol in the treatment of children with HD with less toxicity. However, relapse analysis is difficult to evaluate due to multiple impediments, such as poor attendance during and after treatment, low availability of paraclinical data, and small number of patients. Availability of radiotherapy would increase the therapeutic outcomes.
Conflict of Interest
The authors declare that they have no conflict of interest that competes with any of the contents of the manuscript.
21723
References
- Cotran R, Kumar V, Collins T (200) Hodgkin's disease. Robbins, Pathological Anatomy Bases MorpholPhysiopathol Mal (6th edn), Philadelphia, Pennsylvania: Saunders Co, USA. pp. 813-818.
- Jacquillat C, Auclerc G, Auclerc M-F, Weil M (1984) Hodgkin's disease. Healing and its price Rev Prat34: 1075-1080.
- Landman-Parker J, Gorde-Grosjean S (2009) Hodgkin's lymphoma: Recent physiopathological data. Arch Pediatrics 16:667-668.
- Andon A, Vassal PG, Hartmann O, Couanet D, Oberlin O (2015) Hodgkin's disease. Inst Gustave-Roussy.
- Fagnou C, AF Ray, Leblanc T (1997) Hodgkin's disease of the child. Encyclical. Med chirElsevier, Paris Pediatrics 1997.
- Dinand V, Arya LS (2006) Epidemiology of childhood Hodgkin’s disease: Is it different in developing countries? Indian Pediatr43:141.
- Mbako A, EssameOyono JL, Michel G, Owono D, Fewou A, et al. (2012) Hodgkin's disease in Cameroon: Epidemiological and anatomo-pathological aspects. Arch AnatCytolPathol. 39: 116-119.
- Cogliatti SB, Schmid U (2002) Who is WHO and what was REAL? Swiss Med Wkly 13:607-617.
- Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, et al. (2000) The World Health Organization classification of neoplastic diseases of the haematopoietic and lymphoid tissues: Report of the Clinical Advisory Committee Meeting, Airlie House, Virginia, November 1997. Histopathology36:6986.
- Baez F, Ocampo E, Conter V, Flores A, Gutierrez T, et al. (1997) Treatment of childhood Hodgkin’s disease with COPP or COPP-ABV (hybrid) without radiotherapy in Nicaragua. Ann Oncol Off J EurSoc Med Oncol ESMOMars8:247250.
- Togo B, Traore F, Togo AP, Traore CB, Dumke K, et al. (2011) Hodgkin Lymphoma at the Paediatric Oncology Unit of Gabriel ToureTeaching Hospital, Bamako, Mali: 5-Year Experience. Adv Hematol 1-6.
- Omoti C, Olu-Eddo A (2011) Hodgkin lymphoma: Clinicopathologic features in Benin City, Nigeria and update on its biology and classification. Niger J ClinPract14:440.
- Sherief LM, Elsafy UR, Abdelkhalek ER, Kamal NM, Elbehedy R, et al. (2015) Hodgkin Lymphoma in Childhood: Clinicopathological features and therapy outcome at 2 Centers from a Developing Country. Medicine (Baltimore). avr;94:e670.
- Donaldson SS (2002) VAMP and low-dose, involved-field radiation for children and adolescents with favourable, early-stage Hodgkin’s disease: Results of a prospective clinical trial. J ClinOncol20:30813087.
- Friedmann AM (2002) Treatment of unfavourable childhood Hodgkin’s disease with VEPA and Low-dose, involved-field radiation. J ClinOncol20:30883094.
- Englund A, Hopstadius C, Enblad G, Gustafsson G, Ljungman G (2015) Hodgkin lymphoma -A survey of children and adolescents treated in Sweden 1985-2009. Acta Oncol54:4148.
- Khanfir A, Toumi N, Masmoudi A, Hdiji S, Elloumi M, et al. (2007) Hodgkin's disease of children in southern Tunisia: A study of 23 cases. Cancer/Radiotherapy11: 241-246.
- Seth R (2016) Clinical profile and chemotherapy response in children with Hodgkin Lymphoma at a Tertiary Care Centre. J ClinDiagn Res 2015.
- Alebouyeh M (2005) Successful ambulatory treatment of Hodgkin’s disease in Iranian children based on German-Austrian DAL-HD 85-90: single institutional results. Ann Oncol16:1936-1940.
- Gorde-Grosjean S, Oberlin O, Leblanc T, Pacement H, Donadieu J, et al. (2012) Outcome of children and adolescents with recurrent/refractory classical Hodgkin lymphoma, a study of the French Society for the Fight against Cancer of Children and Adolescents (SFCE). Br J Haematol 158: 649-656.
- Engel M, Essop MF, Close P, Hartley P, Pallesen G, et al. (2000). Improved prognosis of Epstein-Barr virus associated childhood Hodgkin’s lymphoma: Study of 47 South African cases. J ClinPathol53:182-186.
- Montoto S, Camos M, Lopez-Guillermo A, Bosch F, Cervantes F, et al. (2000) Hybrid chemotherapy consisting of cyclophosphamide, vincristine, procarbazine, prednisone, doxorubicin, bleomycin, and vinblastine (C-MOPP/ABV) as first-line treatment for patients with advanced Hodgkin disease. Cancer88:2142-2148.
- Shimabukuro-Vornhagen A, Haverkamp H, Engert A, Balleisen L, Majunke P, et al. (2005) Lymphocyte-rich classical Hodgkin’s lymphoma: Clinical presentation and treatment outcome in 100 patients treated within German Hodgkin’s study group trials. J ClinOncol 23:57395745.
- Laskar S, Gupta T, Vimal S, Muckaden MA, Saikia TK, et al. (2004) Consolidation radiation after complete remission in Hodgkin’s disease following six cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine chemotherapy: Is there a need? J ClinOncol22:62-68.