Keywords
Cervical disc; Cervical disc arthroplasty; Anterior cervical decompression and fusion
Introduction
Cervical disc herniation and degenerative disease of the cervical spine are the most common causes of cervical cord and nerve root dysfunction. It is found that after the age of 40 almost age of 65, 95% of men and 70% of women have radiographic evidence of degenerative changes [1]. Since the first description of the anterior cervical discectomy with fusion by Cloward and Smith in 1958 respectively in 1955, and the cervical anterior discectomy without fusion in 1960 by Hirsch a debate is started which of both methods is the best. While this discussion is still not closed, the advent of the cervical disc prosthesis has contributed to extra confusion. Instead of two possibilities, nowadays three possible treatments concur with each other: anterior cervical discectomy without implantation of any structure, anterior cervical discectomy with fusion, and finally, cervical discectomy with implantation of disc prosthesis [2].
Now-a-days anterior cervical discectomy and fusion (ACDF) may be considered the standard procedure for treatment of degenerative disc disease of the cervical spine. However, there is evidence that ACDF may result in progressive degeneration of the adjacent segments [3]. Total intervertebral disc replacement (TDR) is designed to preserve motion, avoid limitations of fusion, and allow patients to quickly return to routine activities. The primary goals of the procedure in the cervical spine are to restore disc height and segmental motion after removing local pathology. A secondary intention is the preservation of normal motion at adjacent cervical levels, which may be theorized to prevent later adjacent level degeneration. It avoids the morbidity of bone graft harvest, it also avoids complications such as pseudarthrosis, and issues caused by anterior cervical plating and cervical immobilization side effects [4].
Patients and Methods
This is a dual center clinical trial comparing the treatment of 20 patients with degenerative cervical disc disease by anterior cervical discectomy were operated and evaluated over a period of 1 year at the department of Neurosurgery Assiut University Hospital and Gamal Abd El Naser Hospital, Alexandria. The patients were classified into three groups. Group A (1-level fusion): where the anterior decompression was accomplished by single level cervical discectomy, and then insertion of cervical cage at this level. Group B (2-level fusion): where the anterior decompression was accomplished by double level cervical discectomy, and then insertion of cervical cage at both levels. Group C (hybrid construct): where the anterior decompression was in the form of one level cervical discectomy, followed by cage implantation at this level and another level cervical discectomy followed by insertion of cervical disc prosthesis at the same time. The former was filled with spongy bone. Artificial cervical disc devices used in this study is Prestige LP
All cases were subjected to thorough history taking, general and neurological examination and investigations [routine laboratory and imaging studies included plain X-rays of cervical spine (A-P, Lateral and dynamic films: flexion, extension and oblique) and MRI cervical spine. Nerve conduction study was done to exclude peripheral compression neuropathy and to confirm radiculopathy in selected cases where double entrapment phenomena suspected. The inclusion criteria are degenerative disc disease within levels between C3-C7 at single or double level causing neck pain and/or brachialgia; neurologic deficit (some patients included will have signs of myelopathy); age between 18-70 years; failure of conservative treatment for more than 6 weeks or with progressive pain/ neurologic deficit. The exclusion criteria are marked cervical instability eg: translation > 3 mm and/or Segmental angulation >11˚ higher than adjacent levels.; compromised vertebral bodies due to prior surgery or fracture at the affected level; patients with recurrent cervical disc disease; ossification of the posterior longitudinal ligament or diffuse hyperostosis; unknown etiology for neck and/or arm pain.; metabolic bone disease; Paget’s disease; malignant bone diseases and active infection.
The patients were followed up for 1 year. Functional outcome was assessed according to Odom’s criteria. Patient satisfaction: with postoperative results, is evaluated using a patient satisfaction index (PSI). This index is a modified sub item of the North American Spine Society outcome questionnaire. The main outcome measure was pain intensity (neck pain and arm pain) over a 12-month period. Other outcome measures were; duration of operation, length of hospital stay, and complications. The overall effectiveness of the treatment was assessed as using PSI and Odom’s Scale. The mean improvement in pain amongst the treatment groups were first compared with an analysis of variance followed by multiple comparisons tests based on the Bonferroni method. Multiple linear regressions weren’t used to analyze the effect of the treatment since there were no statistically significant baseline characteristics.
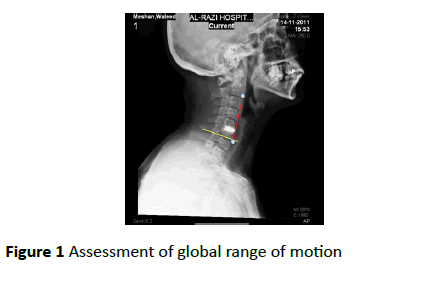
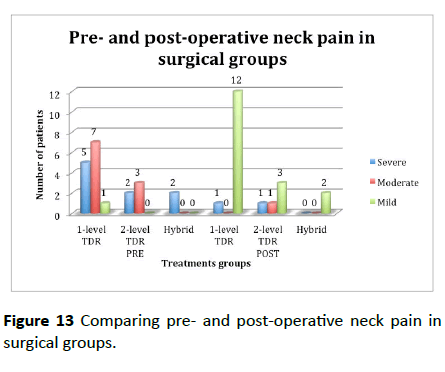
Postoperative plain X-rays of cervical spine (A-P and Lateral) were done at follow-up visits (immediate postoperative, 3 months, 6 months 12 month postoperatively) for evaluation of cervical spine alignment; cervical spine stability; position of the implanted prosthesis; maintenance of cervical motion at operated level in artificial disc group; assessment of global range of motion and fusion of the operated level in case of hybrid cases. Assessment of global range of motion (from C2- C7) is done manually by measuring the difference, in flexion and extension, between an angle formed between a line parallel to the superior end plate of C7 and a line joining the anterior edge of the superior end plate of C7 to the anterior edge of the inferior end plate of C2 (Figure 1).
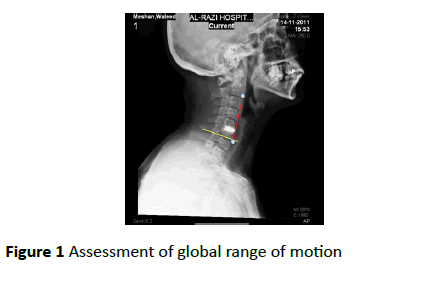
Figure 1: Assessment of global range of motion
MRI or CT of the cervical spine is done for patients routinely and for patients not improving or with persistent preoperative complaint or any new neurologic deficit. The study was approved by the local research ethics committee and informed consent was obtained from all patients prior to their inclusion in the study.
Results
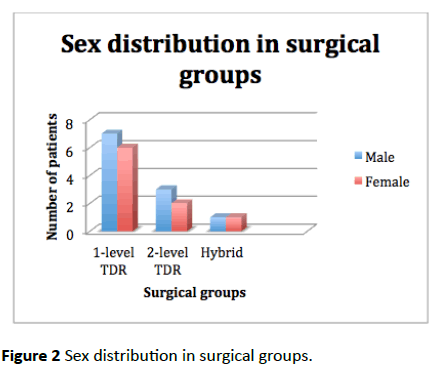
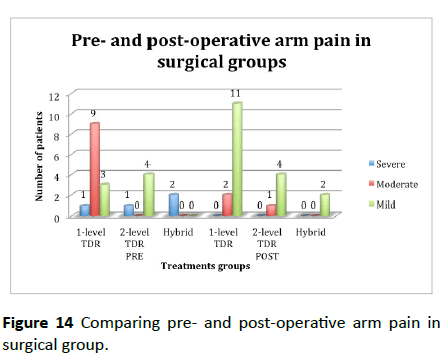
Mean age for all groups was =40 ± 5.9 Years (range: 30-50 years), the mean age ±SD for group of single level was 40 ± 6.6; double level was 37.8 ± 5.5 and 45 ± 7.1 for the hybrid group. Eleven out of the twenty patients (55%) were males, and 9/20 (45%) were females. There were 13 patients in single level group, 5 patients in double level group and 2 patients in hybrid group, 7 males and 6 females in the single level group, 3 males and 2 females in the double level group, and one male and one female in the hybrid group (Figure 2 and Table 1).
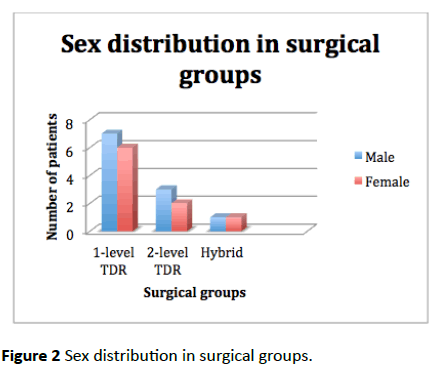
Figure 2: Sex distribution in surgical groups.
| Variables |
Total |
1-level group |
2-level group |
Hybrid group |
| No of patient |
20 |
13 |
5 |
2 |
| AGE/Years Mean(SD) |
40 (5.9) |
40 (6.6) |
37.8 (5.2) |
45 (7.1) |
| Sex |
20 |
13 |
5 |
2 |
| Male n (%) |
11 |
7 (53.8) |
3 (60) |
1 (50) |
| Female n (%) |
9 |
6 (46.2) |
2 (40) |
1 (50) |
| Medical History |
5 |
3 (23.1) |
1 (20) |
1 (50) |
| SMOKING |
2 |
2 (15.4) |
0 (0) |
0 (0) |
| Patients’ clinical features |
| a- Radiculopathy |
20 |
13 (100) |
5 (100) |
2 (100) |
| b-Myelopathy |
0 |
0 (0) |
0 (0) |
0 (0) |
| c- Axial neck pain |
11 |
5 (38.5) |
4 (80) |
2 (100) |
| Duration of symptoms/months |
|
31.8 (10.6) |
31.4 (4.9) |
32 (11.3) |
| Preoperative neck and arm VAS |
| Neck Pain VAS |
| Mild Pain n (%) |
|
1 (7.7) |
0 (0) |
0 (0) |
| Moderate Pain n (%) |
7 (53.8) |
3 (60) |
0 (0) |
| Severe Pain n (%) |
|
5 (38.5) |
2 (40) |
2 (100) |
| Arm Pain VAS |
| Mild Pain n (%) |
|
3 (23.1) |
4 (80) |
0 (0) |
| Moderate Pain n (%) |
9 (69.2) |
0 (0) |
0 (0) |
| Severe Pain n (%) |
|
1 (7.7) |
1 (20) |
2 (20) |
| Patients’ radiological disc level |
| C3-4 n (%) |
|
0 |
0 |
0 |
| C4-5 n (%) |
|
4 (30.8) |
5 (100) |
2 (100) |
| C5-6 n (%) |
|
9 (69.2) |
5 (100) |
2 (100) |
| C6-7 n (%) |
|
0 |
0 |
0 |
Table 1: Patients demography.
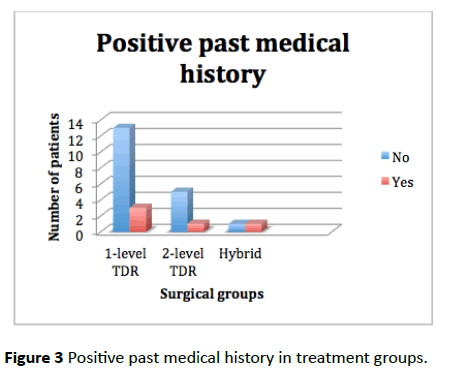
Regarding the past medical history, 4/20 (20%) patients were hypertensive. 3/20 (15%) patients were diabetic. In 16/20 (80%) patients, there was no associated medical diseases. There were 3 patients in the single level group with medical problems (1 was diabetic, 1 was hypertensive, and 1 was diabetic and hypertensive), while in the double level group there was 1 patients with past medical problems (diabetic and hypertensive) and there was 1 patient in the hybrid group with medical problems (diabetic and hypertensive).
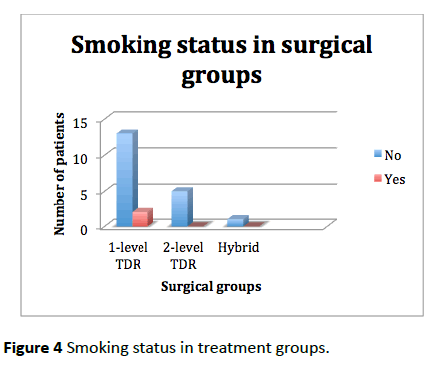
Regarding smoking habits 2/20 (10%) patients were habitual smokers, while 18/30 (90%) were non-smokers There were 2 smokers (15.4%) in the single level group, while in the double level and hybrid groups there were no smokers (Figures 3 and 4).
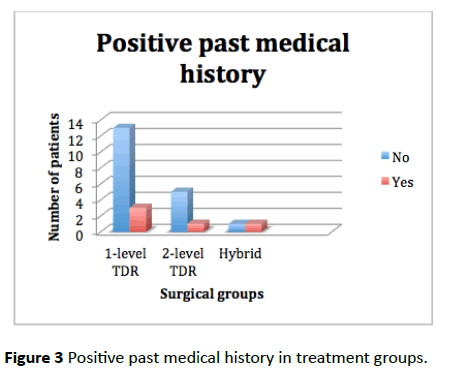
Figure 3: Positive past medical history in treatment groups.
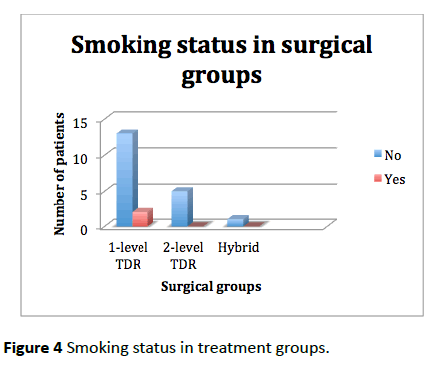
Figure 4: Smoking status in treatment groups.
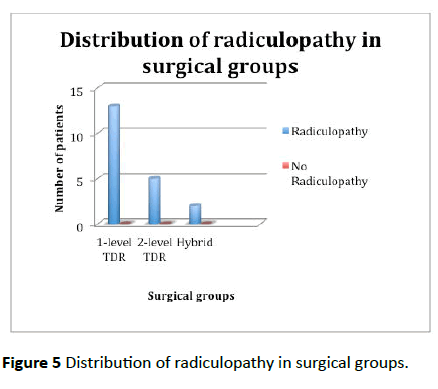
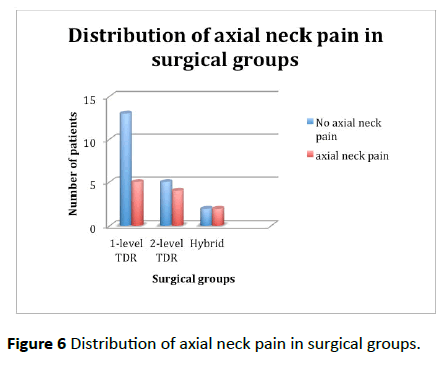
As regards the pre-operative clinical presentations, 13 (100%) patients in the single level group, 5 (100%) patients in the double level group, and 2 (100%) patients in the hybrid group had radiculopathy, and 5 (38.5%) patients in single level group, 4 (80%) patients in the double level group versus 2 (100%) in the hybrid group had axial neck pain.
The mean duration of symptoms was 31.8 months for single level group, 31.4 months for double level group and 32 months in hybrid group. The duration of symptoms ranged from 20 to 60 months in the single level group, while it ranged from 27 to 40 months in the double level group and it ranged from 24 to 40 in the hybrid group (Figure 5).
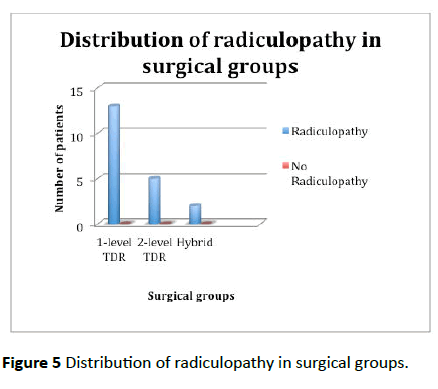
Figure 5: Distribution of radiculopathy in surgical groups.
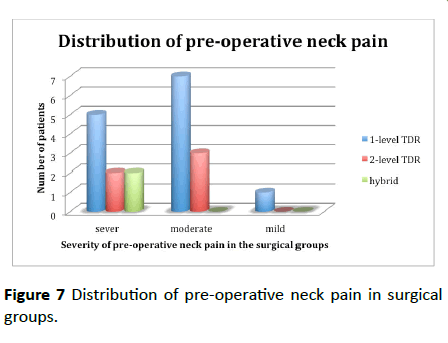
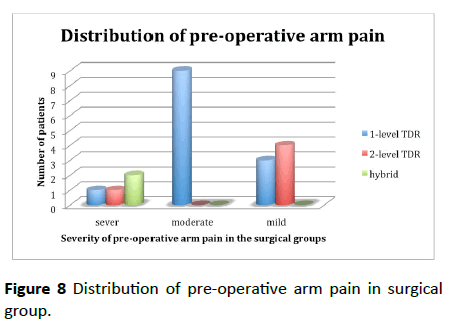
7 (53.8%) of patients in single level group had moderate neck pain versus 3 (60%) in double level group and 0 in hybrid group, while as regards arm pain 9 (69.2%) of patients in the single level group had moderate arm pain versus 1 (7.7%) in the double level group and 2 (100) in the hybrid group had sever arm pain (Figures 6-8).
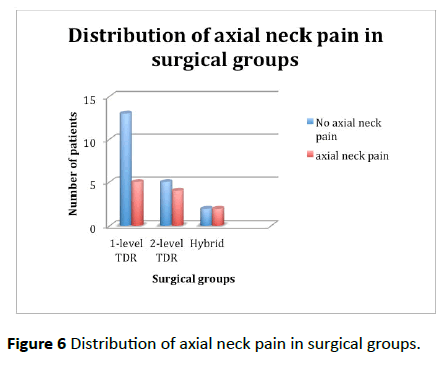
Figure 6: Distribution of axial neck pain in surgical groups.
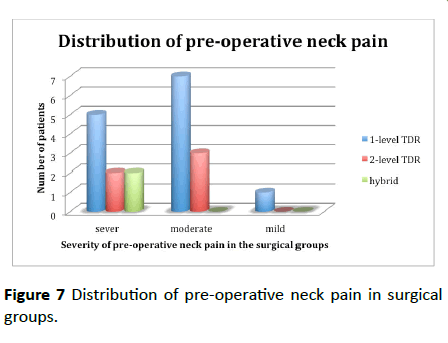
Figure 7: Distribution of pre-operative neck pain in surgical groups.
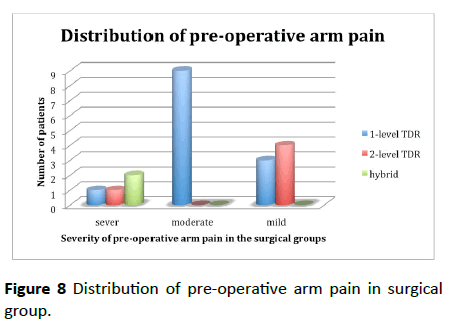
Figure 8: Distribution of pre-operative arm pain in surgical group.
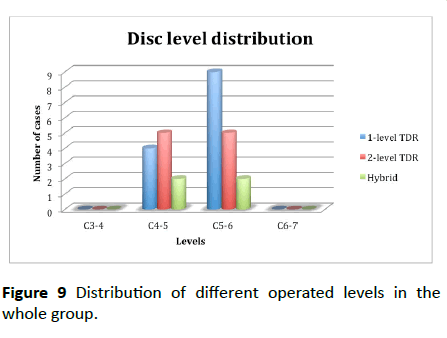
The most common operated level was C5-C6, where it include 9 patients (69.2%) in the single level group, 5 patients (100%) in double level group and 2 patients (100%) in the hybrid group, followed by C4-C5 level including 4 patients (30.8%) in the single level group, 5 patients (100%) in the double level group and 2 patients (100%) in the hybrid group (Figure 9).
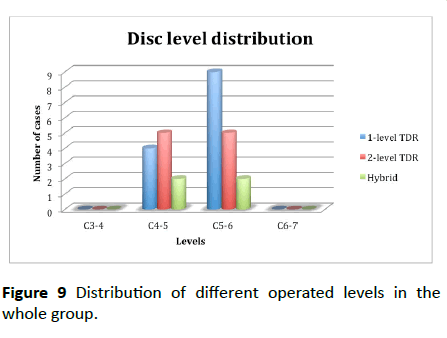
Figure 9: Distribution of different operated levels in the whole group.
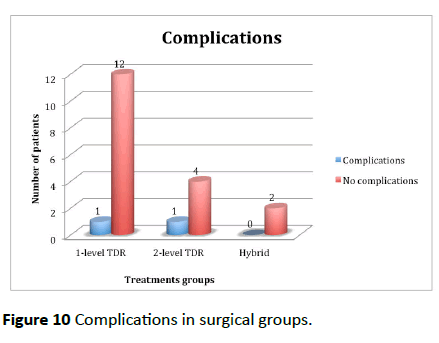
The mean operative time in the single level group was 71.5 minutes, while in the double level group it was 110 minutes and in the hybrid group it was 105 minutes. Regarding the mean duration of hospital stay it was 2.4 days in the single level group while it was 3.8 days in the double level group and 4 days in the hybrid group. For the follow-up duration it ranged from 1 month to 12 months (mean 8.6) in the single level group, while it ranged from 9 months to 12 months (mean 10.4) in the double level group and 9 months in the hybrid group (Figure 10 and Table 2).
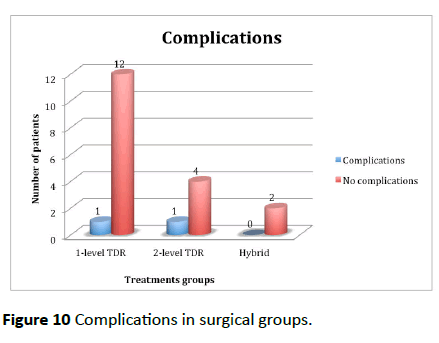
Figure 10: Complications in surgical groups.
| Variables |
Total |
1-level group |
2-level group |
Hybrid group |
| No of patient |
20 |
13 |
5 |
2 |
| AGE/Years Mean(SD) |
40 (5.9) |
40 (6.6) |
37.8 (5.2) |
45 (7.1) |
| Sex |
20 |
13 |
5 |
2 |
| Male n (%) |
11 |
7 (53.8) |
3 (60) |
1 (50) |
| Female n (%) |
9 |
6 (46.2) |
2 (40) |
1 (50) |
| Medical History |
5 |
3 (23.1) |
1 (20) |
1 (50) |
| SMOKING |
2 |
2 (15.4) |
0 (0) |
0 (0) |
| Patients’ clinical features |
| a- Radiculopathy |
20 |
13 (100) |
5 (100) |
2 (100) |
| b-Myelopathy |
0 |
0 (0) |
0 (0) |
0 (0) |
| c- Axial neck pain |
11 |
5 (38.5) |
4 (80) |
2 (100) |
| Duration of symptoms/months |
|
31.8 (10.6) |
31.4 (4.9) |
32 (11.3) |
| Preoperative neck and arm VAS |
| Neck Pain VAS |
| Mild Pain n (%) |
|
1 (7.7) |
0 (0) |
0 (0) |
| Moderate Pain n (%) |
7 (53.8) |
3 (60) |
0 (0) |
| Severe Pain n (%) |
|
5 (38.5) |
2 (40) |
2 (100) |
| Arm Pain VAS |
| Mild Pain n (%) |
|
3 (23.1) |
4 (80) |
0 (0) |
| Moderate Pain n (%) |
9 (69.2) |
0 (0) |
0 (0) |
| Severe Pain n (%) |
|
1 (7.7) |
1 (20) |
2 (20) |
| Patients’ radiological disc level |
| C3-4 n (%) |
|
0 |
0 |
0 |
| C4-5 n (%) |
|
4 (30.8) |
5 (100) |
2 (100) |
| C5-6 n (%) |
|
9 (69.2) |
5 (100) |
2 (100) |
| C6-7 n (%) |
|
0 |
0 |
0 |
Table 2: Operative and post-operative follow up.
There were 2 complications in this study, one (7.7%) in the single level group and one (20%) in the double level group. In the single level group 1 patient had removal of prosthesis due to device failure and hypermobility. In the double level group, one patient had temporary dysphagia and dysphonia.
At the 12-month follow up; regarding neck pain; 12 patients (92.3%) had mild pain, and 1 patients (7.7%) had severe pain in the single level group versus 3 patients (60%) had mild pain, one patient (40%) had moderate pain and one patient (20%) had severe pain in the double level group, and all patients in the hybrid group had mild pain. Regarding arm pain; 11 patients (84.6%) had mild pain and 2 patients (15.4%) had moderate pain in the single level group, versus 4 patients (80%) had mild pain and 1 patients (20%) had moderate pain in the double level group and all patients in the hybrid group had mild pain, no patients had severe pain among all groups.
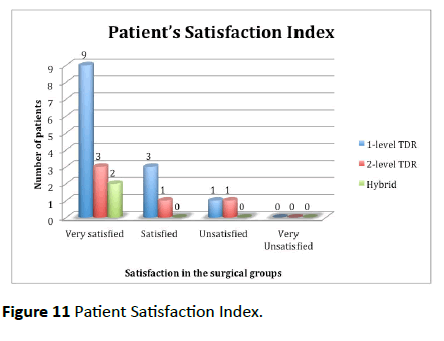
As regard patient satisfaction; 9 patients (69.2%) were very satisfied in the single level group versus 3 patients (60%) In the double level group and 2 patients (100%) in the hybrid group, while there were 3 patients (23.1%) who were satisfied in the single level group and 1 patient (20%) In the double level group, finally only one patient was unsatisfied in the single level group and 1 patient in the double level group (Figure 11).
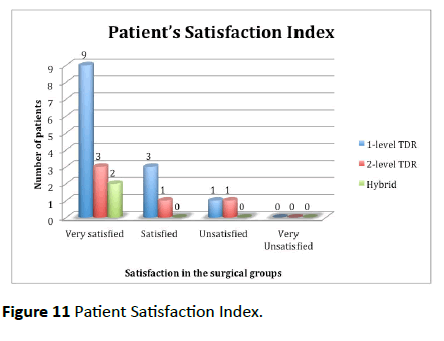
Figure 11: Patient Satisfaction Index.
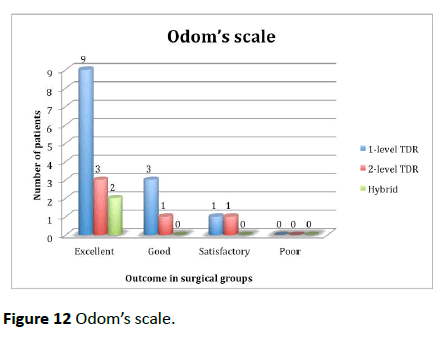
Regarding the functional outcome 9 patients (69.2%) had excellent outcome in the single level group versus 3 patients (60%) In the double level group and 2 patients (100%) in the hybrid group, while there were 3 patients (23.1%) who had good outcome in the single level group and 1 patient (20%) In the double level group, finally only one patient in the single level group and 1 patient in the double level group who had satisfactory outcome (Figure 12 and Table 3).
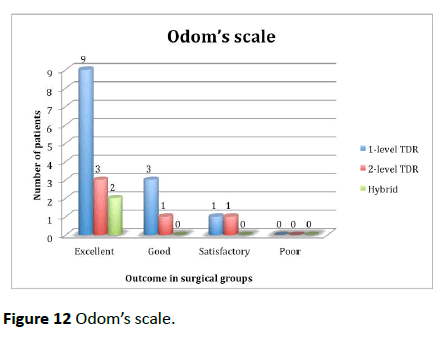
Figure 12: Odom’s scale.
| Treatment groups |
1-level group (n=13) |
2-level group (n=5) |
Hybrid group (n=2) |
| Pre-op |
Post-op
(12 months) |
Pre-op |
Post-op
(12 months) |
Pre-op |
Post-op
(12 months) |
| Neck Pain |
| Mild Pain: n (%) |
1 (7.7) |
12 (92.3) |
0 (0) |
3 (60) |
0 (0) |
2 (100) |
| Moderate Pain: n (%) |
7 (53.8) |
- |
3 (60) |
1 (20) |
0 (0) |
- |
| Severe Pain: n (%) |
5 (38.5) |
1 (7.7) |
2 (40) |
1 (20) |
2 (100) |
- |
| Arm Pain |
| Mild Pain: n (%) |
3 (23.1) |
11 (84.6) |
4 (80) |
4 (80) |
- |
2 (100) |
| Moderate Pain: n (%) |
9 (69.2) |
2 (15.4) |
- |
1 (20) |
- |
- |
| Severe Pain: n (%) |
1 (7.7) |
- |
1 (20) |
- |
2 (100) |
- |
Table 3: Mean improvement in VAS (post-operative at 12 months vs. pre-operative) change in VAS in all groups.
Most of patients in the three groups were suffering from moderate to severe arm and neck pain, in the post-operative follow-up most of patients had mild to moderate pains, only 2 patients in single and double level groups had severe neck pain and no patients among all group had any severe arm pain (Figures 13 and 14).
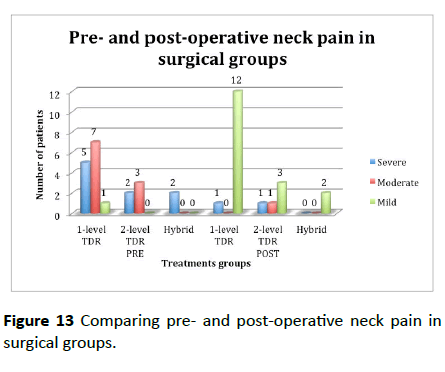
Figure 13: Comparing pre- and post-operative neck pain in surgical groups.
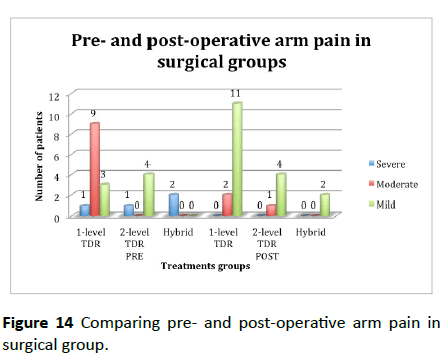
Figure 14: Comparing pre- and post-operative arm pain in surgical group.
The mean decrease in VAS neck was 3.2 in the single level group versus 2.8 in the double level group and 4.5 in the hybrid group (Table 4).
| Variables |
1-level group (n=13) |
2-level group (n=5) |
Hybrid group (n=2) |
| Pre-operative VAS neck |
7 |
7.2 |
8 |
| post-operative VAS neck |
3.8 |
4.4 |
3.5 |
| Decrease in VAS Neck |
3.2 ± 1.6 |
2.8 ± 1.8 |
4.5 ± 1.9 |
Table 4: Mean decrease in VAS neck.
Discussion
Cervical spine is unique in its biomechanics with a complex, wide range, and coupled motion aiming at providing a freedom of movement of the head in respect to the trunk while maintaining stability and protection to the neural structures. Degenerative disc disease results in three major manifestations of cervical disc herniation, depending on whether there is compression of a cervical nerve root or the spinal cord: neck pain, radiculopathy and cervical myelopathy. Diagnosis is achieved by thorough clinical assessment, plane radiography, MRI scans, and neurophysiological studies in selected cases. Surgical treatment of diseases affecting the anterior cervical spine was not safe and effective until 1950s when by Robinson and Smith, Cloward, Bailey and Badgley established the now-popular anterior approach. Surgical management depends on neural decompression followed by reconstruction of the motion segment.
Anterior cervical discectomy and fusion is considered the gold standard surgical management for degenerative cervical disc disease for many decades. But concerns regarding adjacent level accelerated degeneration, beside known complications due to fusion as symptomatic nonunion and donor site complications, raised the expectations to a novel technique to deal with the degenerated cervical motion segment following anterior discectomy [5,6]. Cervical disc replacement is a new treatment modality alternative to fusion; aiming to preserve motion after discectomy. The rationale for arthroplasty is that by maintaining motion, adjacent segment degeneration may be avoided. Other benefits include more rapid recovery and maintenance of function. Early results are encouraging, with success equal to or better than fusion with rare mechanical failures [7].
Cervical arthroplasty prostheses should aim to maintain the normal range and type of intervertebral segmental motion while transmitting axial loading forces from the vertebral body above to the one below [8]. Hypermobility is an indicator of increased stresses on adjacent segments following fusion. Many authors documented increased mobility in adjacent segments after cervical fusion [9-17]. Chronically elevated intradiscal pressures lead to deleterious metabolic degenerative changes followed by progressive adjacent level disease. This is because the cervical intervertebral disc is an avascular structure and nutrient exchange is primarily dependent on diffusion and osmotic pressure gradients [18] Many investigators recorded increased intradiscal pressure following cervical fusion (as an indicator of increased stresses) [12,17,18].
This study revealed that mean age for the three groups was=40 years (range: 30-50 Years), the mean age for group of single level fusion was 40; double level g was 37.8 and 45 for the hybrid group of fusion was 46.8 and 48.5 for the artificial disc group. Which are comparable to other related studies in literatures [19-21]. Regarding the Three studied groups, the single level group showed male predominance (53.8% males), while the double level group showed also male predominance (60% males) and the fusion group showed equal sex distribution (50% each).
Single and double level disc disease are only included in this study, the most common operated level was C5-C6; it represents 69.2% in the single level group, 100% in double level group and 100% in the hybrid group, followed by C4-C5 level; it represents 30.8% in the single level group, 100% in the double level group and 100% in the hybrid group. This goes nearly with all the related studies, as Ryu et al. [22] stated that the most common operated levels were C5-C6 (51%). while in Seok Woo Kim et al. [21] C5/6 represented 61.5% in the artificial disc group, followed by C6-C7 level including 21% in the artificial disc group. In Sekhon et al. [1], they stated that the frequency of C5-C6 was 88%.
This prevalence can be explained by the concentration of forces at that level during neck flexion, or the decrease of canal diameter in relation to the cord diameter that makes this level more sensitive to disc prolapsed [23]. Standard anterior decompression was done followed by insertion of cervical cage, a variety of implant types sizes were used according to patients` varying anatomy, while in the hybrid group zeroprofile implant for stand-alone anterior cervical interbody fusion were used.
The mean operative time in the single level group was 71.5 minutes, while in the double level group it was 110 minutes and in the hybrid group it was 105 minutes. Rick C. Sasso et al. [4] stated that it was 70 minutes for the fusion group while it took 105 minutes in the artificial disc group, which was longer than our study. For the follow-up duration it ranged from 1 month to 12 months (mean 8.6) in the single level group, while it ranged from 10 months to 12 months (mean 10.4) in the double level group and 9 months in the hybrid group.
Regarding the clinical picture, the most common presentation was radiculopathy, 100% of patients in all groups had radiculopathy versus 38.5% patients in single level group, 80% patients in the double level group versus 100% in the hybrid group had axial neck pain. That was merely similar to that stated by other investigators. Seok Woo Kim et al. [21] reported in their series 92% patients in the artificial disc group had radiculopathy. In Lafuente et al. [24], 80% had radiculopathy.
In this study; all patients showed improvement in neck and arm pain, for the neck pain; mean decreased from 7 to 3.8 in the single level group while it decreased from 7.2 to 4.4 in the double level group and from 8 to 3.5 in the hybrid group. For the arm pain; mean decreased from 6.8 to 3 in the single level group while it decreased from 6.6 to 2.8 in the double level group and from 7.5 to 2 in the hybrid group. All patients showed postoperative improvement in neurologic deficit that was more rapid in the sensory deficit. Improvements of arm pain (radiculopathy) and in neurologic deficit are directly related to the adequacy of decompression. Thus, improvements in arm pain (radiculopathy) and in neurologic deficit in the three operated groups are similar to each other as all shares the same technique.
Regarding the functional outcome according to Odom’s criteria, in the single level group 92.3% of patients had excellent and good outcome, while the double level group 80% of patients had excellent and good outcome and in the hybrid group 100% of patients had excellent outcome. There was no significant statistical difference between groups. All these are comparable and agreed with results of other studies. As regard patient satisfaction; 69.2% were very satisfied in the single level group versus 60% in the double level group and 100% in the hybrid group, while there were 23.1% who were satisfied in the single level group and 20% in the double level group, finally only one patient was unsatisfied in the single level group and 1 patients in the double level group. In the singlelevel study 86% of patients evaluated at 1-year follow-up Odom’s scale was excellent, While In the bi-level study 82% of patients evaluated at 1-year follow-up Odom’s scale was excellent [25].
There were 2 complications in this study, one (7.7%) in the single level group and one (20%) in the double level group. In the single level group 1 patient had removal of prosthesis due to device failure and hypermobility. In the double level group, one patient had temporary dysphagia and dysphonia. In Lei Cheng et al. [20], there were no spontaneous fusions and no device failures in the artificial disc group. One patient has a deep vein thrombosis in the artificial disc group, and one patient has dysphagia in the control group. In Goffin et al. the single-level study, there were three reinterventions at the treatment level. They included an evacuation of a prevertebral hematoma, a posterior foraminotomy without device involvement to treat residual symptoms. While In the bi-level study, one patient experienced CSF leak while decompressing posteriorly. In addition, there were four reinterventions at the treatment level that included an evacuation of an epidural hematoma, an evacuation of a prevertebral hematoma, a repair of a pharyngeal tear/esophageal wound. There have been no device failures or device explants in either study [25].
The global range of movement increased by mean of 9.8 degrees in the single level group, on the other hand global range of movement increased my mean of 11.8 degrees in the double level group, while it is increased by mean of 9 degrees in the hybrid group. These goes in accordance with other related studies; Seok Woo Kim et al. [21] reported that global range of movement increased by 3.5 degrees in the artificial disc group. Coric D et al. [26] reported that it improved by 0.91 degrees in the combined arthroplasty group. In Goffin et al. At the 1-year follow-up, 88% of the patients in the single-level and 86% of the patients in the bi-level study exhibited motion equal to or greater than 2 degrees. At the 1-year follow-up, 93% of the patients in the single-level study exhibited motion equal to or greater than 2 degrees [26].
Cepoiu-Martin et al. [27], artificial cervical disc arthroplasty (ACDA) is a surgical procedure that may replace cervical fusion in selected patients suffering from cervical degenerative disc disease. Within 1 year of follow-up, the effectiveness of ACDA appears similar to that of cervical fusion. Weak evidence exists that ACDA may be superior to fusion for treating neck and arm pain. Richards et al. [28] documented that there is inadequate evidence to promote extensive use of artificial discs for cervical spondylosis, despite promising short-term and intermediate clinical outcomes. Despite the size of investment and research into arthroplasty outcomes, long-term follow-up has yet to be completed and has not convincingly demonstrated the effect of artificial discs on adjacent segment disease. While Coric et al. [26] stated that cervical total disc replacement allows for neural decompression and clinical results comparable to ACDF. Cervical disc replacement was associated with a significantly greater overall success rate than fusion while maintaining motion at the index level. Furthermore, there were significantly fewer disc replacement patients showing severe adjacent-level radiographic changes at the 1-year follow-up.
Conclusion and Recommendations
Ideal treatment for cervical degenerative disc disease must deal with and improve its three components (axial neck pain, radiculopathy, and myelopathy), normalize cervical spine biomechanics so not to act as a nidus accelerating the degenerative process, and improves the functional outcome of the patient without serious complications. Anterior cervical discectomy with either cervical fusion in one level, two levels or hybrid construct nearly provide similar clinical outcome results, short hospital stays and patient satisfaction. There is no remarkable difference in clinical post-surgery outcome among the three groups. No major complications reported with cervical arthroplasty regarding subsidence, migration and breakage except in the single level group, one patient had removal of prosthesis due to device failure and hypermobility followed by fusion. It is believed that cervical disc replacement will demonstrate the potential to play an increasingly prominent role in the treatment of degenerative cervical disc disease but long-term study with a wider patient population is needed to confirm results of this study.
21846
References
- Phillips FM, Garn SR (2005) Cervical disc replacement. Spine 30: 27-33.
- Bartels RHMA, Donk R, Van der Wilt GJ, Grotenhuis A, Venderink D (2006) Design of the PROCON trial: a prospective, randomized multi – center study comparing cervical anterior discectomy without fusion, with fusion or with arthroplasty. BMC Musculoskeletal Disorder 7: 85.
- Nabhan A, Ahlhelm F, Shariat K, Pitzen T, Steimer O, et al. (2007) The proDisc-C prosthesis: Clinical and radiological experience 1 year after surgery. Spine 32: 1935-1941.
- Sasso RC, Smucker JD, Hacker RJ, Heller JG (2007) Artificial disc versus fusion: A prospective, randomized study with 2-year follow-up on 99 patients. Spine 32: 2933-2940.
- McAfee PC (2004) The indications for lumbar and cervical disc replacement. Spine J 4: 177S-181S.
- Albert TJ (2004) Eichenbaum MD: Goals of cervical disc replacement. Spine J 4: 292S-293S.
- Pracyk JB, Traynelis VC (2005) Treatment of the painful motion segment: Cervical arthroplasty. Spine 30: S23-S32.
- Porchet F, Metcalf NH (2004) Clinical outcomes with the Prestige II cervical disc: Preliminary results from a prospective randomized clinical trial. Neurosurgical Focus 17: E6.
- Kienapfel H, Koller M, Hinder D, Georg C, Pfeiffer M, et al. (2004) Integrated outcome assessment after anterior cervical discectomy and fusion: Myelocompression but not adjacent instability affect patient-reported quality of life and cervical spine symptoms. Spine 29: 2501-2509.
- Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, et al. (1993) Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine 18: 2167-2173.
- Wigfield C, Gill S, Nelson R, Langdon I, Metcalf N, et al. (2002) Influence of an artificial cervical joint compared with fusion on adjacent level motion in the treatment of degenerative cervical disc disease. Journal of Neurosurgery 96: 17-21.
- Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG (2002) Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Journal of Spinal Disorders & Techniques 27: 2431-2434.
- Dingell DJ, Roberston JT, Metcalf NH (2003) Biomechanical testing of an artificial cervical joint and an anterior cervical plate. Journal of Spinal Disorders & Techniques 16: 314-323.
- Schwab JS, DiAngelo DJ, Foley KT (2006) Motion compensation associated with single-level cervical fusion: Where does the lost motion go? Spine 31: 2439-2448.
- Hwang SL, Hwang YF, Lieu AS, Lin CL, Kuo TH, et al. (2003) Outcome analyses of interbody titanium cage fusion used in the anterior discectomy for cervical degenerative disc disease. Spine 28: 314-323.
- Ragab AA, Escarcega AJ, Zdeblick TA (2006) A quantitative analysis of strain at adjacent segments after segmental immobilization of the cervical spine. J Spinal Disorder Tech 19: 407-410.
- Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, et al. (2007) Range of motion change after cervical arthroplasty with ProDisc-C and prestige artificial discs compared with anterior cervical discectomy and fusion. J Neurosurg Spine 7: 40-46.
- Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, et al. (2005) Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: An in vitro human cadaveric model. journal of neurosurgery spine 30: 1165-1172.
- Kawashima M, Tanriover N, Rhoton AL, Matsushima T (2003) The transverse process, intertransverse space, and vertebral artery in anterior approaches to the lower cervical spine. J Neurosurgery (Spine) 98: 188-194.
- Cheng L, Nie L, Zhang L, Hou Y (2009) Fusion versus Bryan cervical disc in two-level cervical disc disease: A prospective, randomized study. International Orthopedics 33: 1347-1351.
- Kim SW, Limson MA, Kim SB, Arbatin JJ, Chang KY, et al. (2009) Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Euro Spine J 18: 218-231.
- Ryu SI, Mitchelle M, Kim DH (2006) A prospective randomized study comparing a cervical carbon fiber cage to the Smith-Robinson technique with allograft and plating up to 24 months follow up. European Spine Journal 15: 157-164.
- Vavruch L, Hedlund R, Javid D, Lesziewski W, Shalabi A (2002) A prospective randomized comparison between the cloward procedure and a carbon fiber cage in the cervical Spine: a clinical and radiologic study. Spine 27: 1694-1701.
- Lafuente J, Casey ATH, Petzold A, Brew S (2005) The Bryan cervical disc prosthesis as an alternative to arthrodesis in the treatment of cervical spondylosis. J Bone Joint Surg 47: 508-512.
- Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, et al. (2004) Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 17: 79-85.
- Coric D, Cassis J, Carew JD, Boltes MO (2010) A prospective study of cervical arthroplasty in 98 patients involved in 1 of 3 separate investigational device exemption studies from a single investigational site with a minimum 2-year follow-up. J Neurosurgery Spine 13: 715-721.
- Cepoiu-Martin M, Faris P, Lorenzetti D, Prefontaine E, Noseworthy T, et al. (2011) Artificial cervical disc arthroplasty: A systematic review, Spine 36: 1623-1633.
- Richards O, Choi D, Timothy J (2011) Cervical arthroplasty: The beginning, the middle, the end? Br J Neurosurgery 26: 2-6.