Mini Review - (2022) Volume 14, Issue 7
Evaluation of spectrum of clinical presentation and role of Amh in women with PCOS attending the Gynae-Obs Opd of a tertiary care hospital
Ishita Mathur* and
Shivali Rana Manwatkar
Shri Guru Ram Rai Institute of Technology and Science, Dehradun, Uttarakhand, India
*Correspondence:
Ishita Mathur, Shri Guru Ram Rai Institute of Technology and Science,
Dehradun, Uttarakhand,
India,
Email:
Received: 25-Jun-2022, Manuscript No. ipaom-22-12570;
Editor assigned: 28-Jul-2022, Pre QC No. P-12570;
Reviewed: 17-Jul-2022, QC No. Q-12570;
Revised: 22-Jul-2022, Manuscript No. R-12570;
Published:
30-Jul-2022
Abstract
Background: Polycystic ovarian syndrome (PCOS) is an endocrine
disorder that affects reproductive females worldwide and has 10%
prevalence. The major endocrine disruption is hyperandrogenism,
oligo-anovulation and some women may also have abnormal insulin
activity.1 Various body systems are affected by polycystic ovarian
syndrome which results in health complications like menstrual
dysfunction, hirsutism, acne, obesity, and metabolic syndrome.
Aim: This study emphasizes on evaluating the spectrum of clinical
presentation of PCOS and Role of AMH in women with PCOS
attending the Gynae-Obs Out-patient department of a tertiary care
hospital.
Methodology: A prospective observational study was carried out
in the Gynecology & Obstetrics OPD at SMI Hospital, Dehradun. A
self-designed questionnaire-based study was conducted on subjects
with symptoms of Polycystic Ovarian Syndrome.
Data collection: The data collected included: Demographic details,
Family History, Gynecological History, Clinical features, Personal
Habits. Microsoft Excel and SPSS 25 software was used for the
calculations.
Results: The incidence rate of PCOS, the mean age of women
diagnosed with PCOS and mean of menarche were calculated. It
was found that 20% of PCOS women were obese and had a BMI
above 30 kg/m2. 37% of PCOS women were overweight and had
a BMI between 25.1-29.9 kg/m2. Global Acne Scoring Method and
Ferriman-Galleway method were used to assess occurrence of acne
and hirsutism. Part from the spectrum of clinical presentation, the
emerging role of AMH in PCOS was also evaluated. SPSS 25 software
was used for statistical analysis for evaluating the effects of risk
factors associated with PCOS on Serum AMH levels. Chi-square tests
were used for the assessment of co-relation among these factors.
P-value <0.05 was considered significant. The risk factors that were
significant to AMH levels were Duration of period cycle, Flow in
menses, History of DM, thyroid issues and hypertension, Family
history of DM, hypertension, thyroid issues, Gynecological history of
mother and sisters, and BMI.
Conclusion: In conclusion, the present study suggests that PCOS
is an emerging health concern among reproductive women and is
associated with many consequences like menstrual irregularities,
hirsutism, acne, alopecia, and infertility, which were common
endocrine disorders. Family history of diabetes and hypothyroidism
were important risk factors associated with PCOS. Women who
were overweight/obese were at a higher risk of developing PCOS.
History of menstrual irregularities and PCOD/PCOS in mother and
sisters of women also had significance in the occurrence of PCOS.
AMH levels will provide reliable information in diagnosing PCOS and
should be used in future along with Rotterdam or NIH criteria.
Keywords
Bariatric; Surgery; COVID-19
Introduction
Antibiotics Polycystic ovarian syndrome (PCOS) is an
endocrine disorder that affects reproductive females
worldwide and has a 10% prevalence. The major endocrine
disruption is hyperandrogenism, oligo-anovulation and
some women may also have abnormal insulin activity.
[1]. Various body systems are affected by polycystic
ovarian syndrome which results in health complications
like menstrual dysfunction, hirsutism, acne, obesity, and
metabolic syndrom [1]. PCOS also characterizes a risk of
dyslipidemia, Type-II diabetes, and cardiovascular disease.
There is a variable degree of expression in every case which
is why it is referred to as a Syndrome and not a disease.
[2] the most common risk factors associated with PCOS
are obesity, diabetes mellitus, thyroid issues, high intake
of fatty foods, lack of physical exercise, and family history
of diabetes, hypertension, thyroid, PCOD, and other
menstrual cycle irregularity disorders. In 2004, Rotterdam
established a diagnostic -criteria for PCOS, according to
which there should be a presence of at least two of the
following characteristics:
• Chronic anovulation
• Hyperandrogenism
• Polycystic ovaries on ultrasonography
In the pathophysiology of PCOS, the most common
finding is ovarian dysfunction. This ovarian dysfunction
is strongly affected by alteration in the Gonadotropinreleasing
hormone. This causes an increase in the Luteinising
hormone (LH), which in turn causes hyperandrogenism,
and infertility [3]. Alteration in insulin resistance leads
to increased insulin production, called hyperinsulinemia,
which might lead to complications like Diabetes mellitus
and exaggerates symptoms of PCOS. Environmental
factors and lifestyle also play an important role in the
pathophysiology of PCOS3.
Clinical Presentation and Symptomatology
The symptoms of PCOS include:
Menstrual irregularity: As compared to non-PCOS
women, women who have PCOS have irregular menstrual
cycles. This leads to oligomenorrhea, hypomenorrhea,
dysmenorrhea and, amenorrhea. [4]
Hirsutism: Hirsutism is defined as the excessive
terminal hair growth that usually takes up a male pattern
distribution. Hairs cover the entire surface of the human
body, except for the lips, palms of the hands, and soles of
the feet [2].
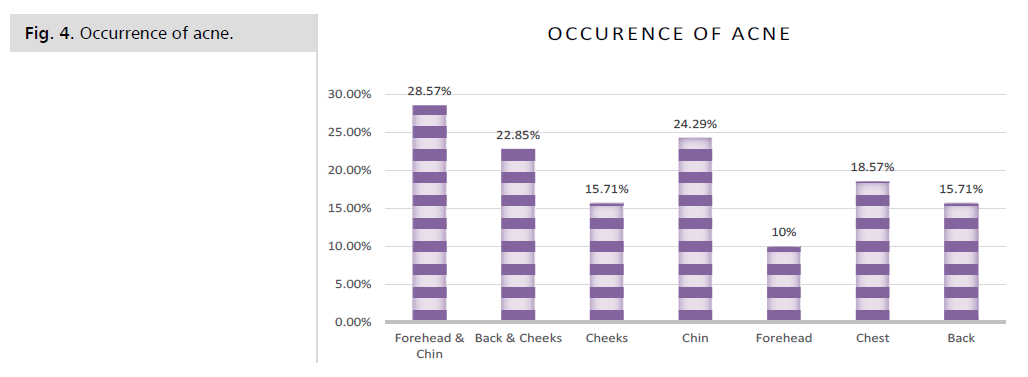
Oily Skin & Acne: Women with PCOS have
complaints of acne in areas of cheeks, chin, chest, forehead,
and back due to hormonal imbalances [4-13].
Alopecia: Due to hormonal imbalances, several women
with PCOS presents with hair fall issues that are more than
norma [14].
Weight gain: Sudden weight gain in PCOS women is
an important clinical finding [4].
Role of Anti-Mullerian Hormone in the pathophysiology
of PCOS:The ovarian follicle consists of the oocytes which
are responsible for the reproductive function in women.
With age, the size of the ovarian follicle and the number of
oocytes decreases, causing a decrease in the ovarian reserve
[7]. The ovarian follicle is developed at the fetal age, with
about a million oocytes present at the time of birth. The
number decreases during childhood and at menarche, there
are about 3-5 lac oocytes present [7]. From the follicle pool,
they enter into the growing pool with the help of FSH. From
this growing pool, only one follicle becomes dominant and
ovulates under the LH influence. This process continues
till menopause when all the follicles are exhausted [7,8].
For the assessment of ovarian reserve in an individual,
serum FSH is measured by assessing the inhibin B and E2
concentrations, which are produced in response to FSH7.
These serum values have relative changes according to
reproductive age and are not independent of each other. So
far ultrasonography best predicts the Antral Follicle Count
in the ovaries but is not feasible all the time, so a serum
marker is required for this and Anti-Mullerian hormone
does the job effectively [9,10]. An Anti-Mullerian hormone
is produced by the cells of the antral follicles and its levels
can be assessed in the serum [7]. AMH levels can be used
for determining ovarian aging. It is exclusively secreted by
the growing follicles, so it gives an indirect measurement of
the follicle pool. Since elevated FSH levels are not detected
in the serum till the cycles become irregular, so serum
AMH values are more reliable [7,6,10].
In conditions like PCOS, serum AMH levels can
provide information on ovarian pathophysiology. In PCOS,
there is a disruption in the selection of a dominant follicle
to be ovulated, which results in anovulation [7,8]. As a
result of this, several small growing follicles produce AMH,
and so AMH levels are increased in women suffering from
polycystic ovaries. Sometimes, there is a small number of
follicles present that are not detected in ultrasonography,
but they contribute to the secretion of AMH, which is why
serum AMH levels are elevated giving a clear diagnosis
of PCOS [7,8,10]. Serum AMH levels in PCOS women correlate with other clinical features like mean ovarian
volume, testosterone levels, free androgen, cycle duration [7].
Purpose of study
Saunhagya Kumar Jena, et al. (2020) conducted a
study to find the perception and awareness of PCOS and
its prevalence among young women [11]. The period taken
for the study was about 2 years, a validated questionnaire
was formed, descriptive analysis was used. Most aware
women were from urban areas [11]. The study conclusion
suggests awareness and knowledge about PCOS in women
in rural areas were very low and need to be improved [11].
As PCOS is a very common condition nowadays, there is
a need for awareness regarding PCOS among reproductive
women. according to the present scenario, a major risk
factor for the occurrence of PCOS is the lifestyle of women.
Nowadays most women in the urban areas are consuming
junk foods and high fatty foods, with less or no physical
activity, which increases obesity and hence the risk. The
benefit of conducting this study is that we get a closer
outlook on the health issues regarding PCOS, as it is an
emerging health concern among young girls. It will provide
access to information about clinical features and biological
problems related to a patient directly. PCOS is considered
a syndrome, due to its diversity of clinical presentation
in various patients. The various manifestation that is
presented is irregular cycles of menstruation, scanty flow,
hirsutism, acne, hair-fall, acanthosis nigricans, etc. These
symptoms are also accompanied by metabolic irregularities
like diabetes mellitus, or thyroid issues, hypertension, and
infertility. This study will help to differentiate between these
complications and will help to find out the association of
them with the occurrence and severity of PCOS. Until now,
only the Rotterdam criteria are being used to diagnose the
PCOS condition. As per the review of literature conducted,
we found that Anti- Mullerian hormone levels also have a
close association with PCOS. The AMH level shows signs
of anovulation, which leads to polycystic ovarian disease.
AMH levels also correlate with the severity of PCOS. So,
in this study, we are aiming at finding a correlation of
AMH levels in PCOS, thereby establishing AMH levels as
a biomarker of PCOS and possibly a new diagnostic tool
in PCOS.
Objective
• To assess the incidence of PCOS patients coming to
the Gynecology-Obstetrics OPD
• To evaluate the clinical presentation of PCOS
• To assess the role of Anti-Mullerian hormone levels
among PCOS patients
• To assess the role of genetic predisposition in PCOS
Ethical approval
The study was duly approved by the Institution Ethics
Committee ahead of the start of the work.
Methodology
Study Design
It is a prospective observational study.
Study Site
Department of Gynecology and Obstetrics OPD at
SMI Hospital, Dehradun.
Study Duration
Approx. 8 months
Sampling methods
Inclusion criteria:
• Females of reproductive age having symptoms of PCOS
• Females who have relevant biochemical data values
suggestive of PCOS
• Females who have ultrasound suggestive of
Polycystic ovaries
• Females who have elevated Anti-Mullerian
Hormone levels
Exclusion criteria:
• Pre-adolescent females
• Post-menopausal females
• Psychiatric patients who have PCOS
• Pregnant females
A prospective observational study was carried out
in the Gynecology & Obstetrics OPD at SMI Hospital,
Dehradun. A self-designed questionnaire-based study
was conducted on subjects with symptoms of Polycystic
Ovarian Syndrome. The study proposal was approved by
the Institutional Ethics Committee. The consent of the
subject was taken according to the Informed Consent
Form prior to the data collection. The eligibility criteria
were: Females of reproductive age having symptoms of
PCOS, Females who have relevant biochemical data
values suggestive of PCOS, Females who have ultrasound
suggestive of polycystic ovaries, Females who have elevated
Anti-Mullerian hormone levels. Rotterdam criteria were
used for the diagnosis of PCOS. The following details were
obtained from the subjects: Demographic details(name,
age, marital status, address), Family history (Diabetes
mellitus, thyroid, Hypertension, mother’s and sister’s
menstrual history, PCOS history, infertility, and other
relevant details), Social history, Gynecological history(age
of menarche, duration of the menstrual cycle, length of
menses, and flow in the menses) Clinical features(acne,
hirsutism, hair fall, mood swings), and Personal habits(teadrinking
habits, alcohol intake, junk-food intake, and
physical activity).
Weight and height were measured by standard protocol and calibrated instruments to calculate the BMI.
Calibrated sphygmomanometer was used to measure the
blood pressure to assess hypertension. Hirsutism was
assessed bases on the hair growth in upper lips, chest, chin,
upper and lower abdomen, thighs, upper and lower back,
and upper arms. This is referred to as the Ferriman-Gallwey
method. The severity of acne was assessed by the Global
acne scoring method. Blood test reports of biochemical
estimation of hormones like LH, FSH, and serum AMH
were collected. Ultrasonography reports indicating PCOS
morphology were collected. After the data collection,
the data was entered into Microsoft Excel and further
calculations were done. All the mean values and standard
deviations were calculated by appropriate methods in Excel.
For the calculation of correlation between the risk factors
and serum AMH levels, Chi-square test was used in SPSS
25 software and results were calculated accordingly [13-20].
Results
A total number of 2500 women were screened and
evaluated for PCOS during the study period. According
to the study conducted, the incidence of PCOS among
patients attending the Gyne-Obs OPD was calculated.
Out of 2500 women, 600 was found to have PCOS, as
diagnosed by the Rotterdam criteria. By this, we concluded
that the incidence rate of PCOS was 0.24 cases per persontime
at risk, the age group with the highest number
of PCOS patients was 21-25 years and the mean age of
women diagnosed with PCOS was 24± 4.96 years. The
risk- factors taken into consideration were (Tab. 1- 5):
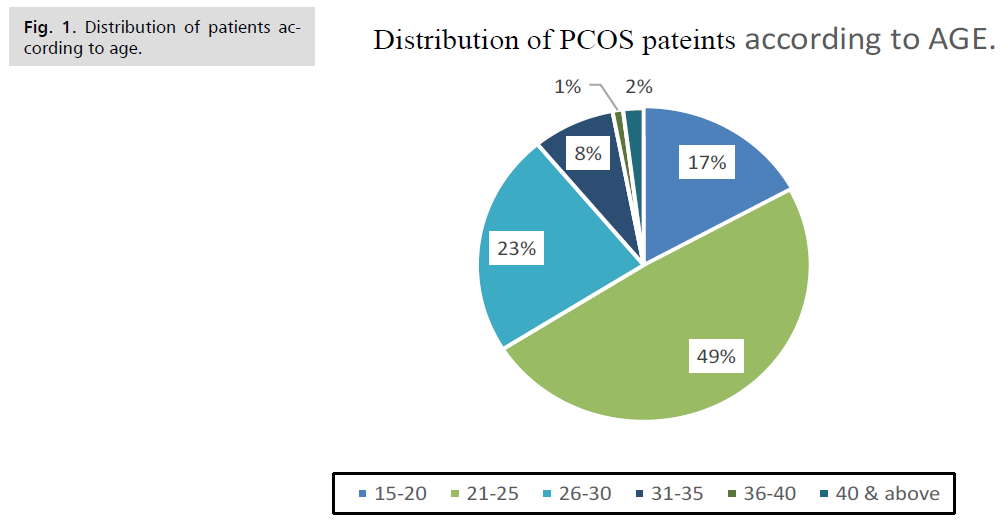
| Age Group (years) |
Number of Patients |
Percentage (%) |
| 15-20 |
102 |
17% |
| 21-25 |
294 |
49% |
| 26-30 |
138 |
23% |
| 31-35 |
48 |
8% |
| 36-40 |
6 |
1% |
| 41 and above |
12 |
2% |
Tab 1: Distribution of patients according to age.
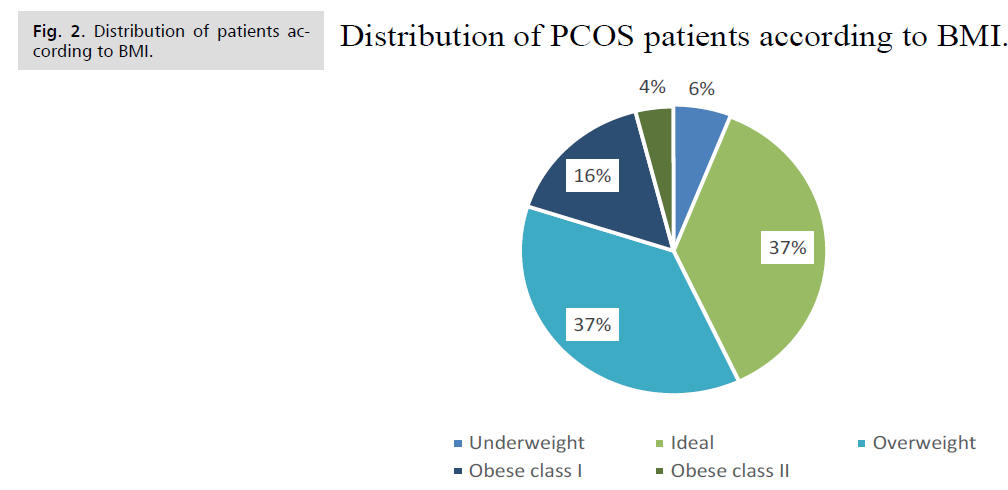
| BMI (kg/m2) |
Category |
Number |
Percentage (%) |
| <18.0 |
Underweight |
36 |
6% |
| 18.1-24.9 |
Ideal |
222 |
37% |
| 25.0-29.9 |
Overweight |
222 |
37% |
| 30.0-34.9 |
Obese class I |
96 |
16% |
| 35.0-39.9 |
Obese class II |
24 |
4% |
| >40.0 |
Obese class III |
- |
- |
Tab. 2. Distribution of patients according to BMI.
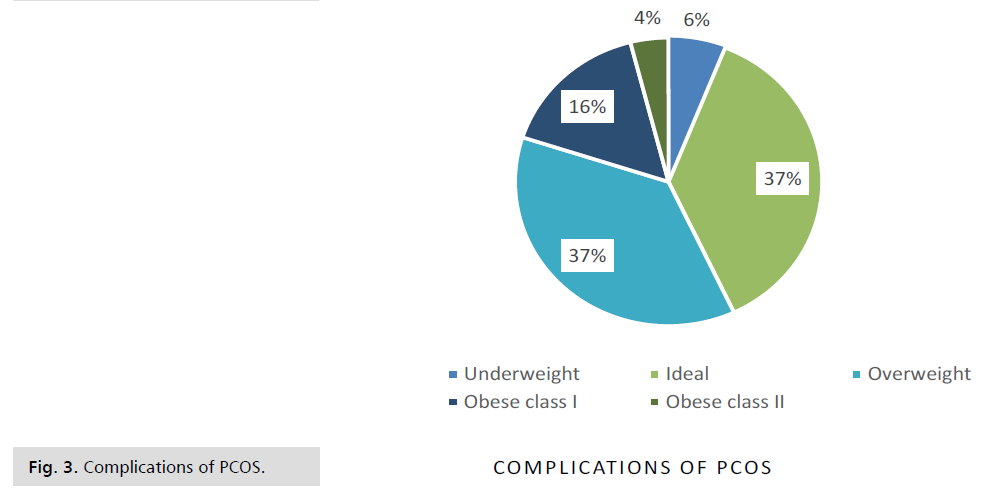
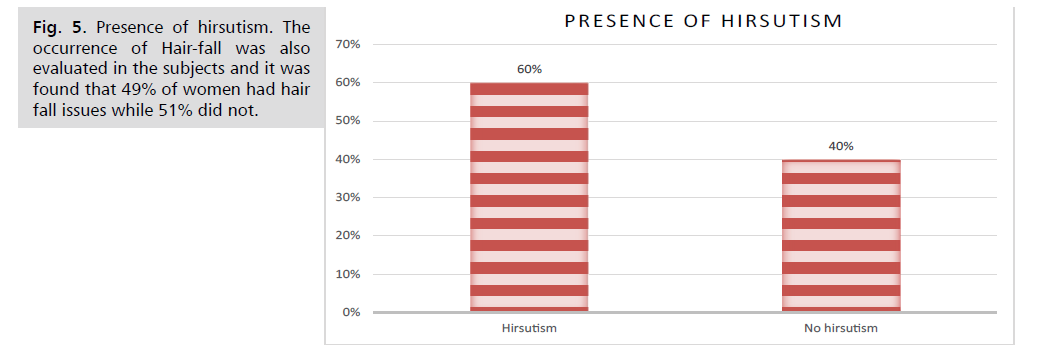
| Conditions/Complications |
Number |
Percentage (%) |
| Oily skin |
498 |
83% |
| Acne |
420 |
70% |
| Hirsutism |
360 |
60% |
| Alopecia |
294 |
49% |
| Acanthosis nigricans |
126 |
21% |
Tab. 3. Complications of PCOS.
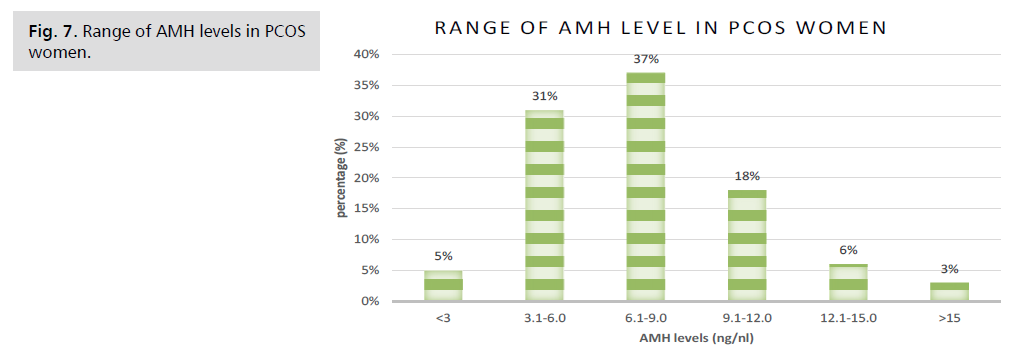
| Range of AMH levels (ng/ml) |
Percentage of women (%) |
| <3 |
5% |
| 3.0-6.0 |
31% |
| 6.1-9.0 |
37% |
| 9.1-12.0 |
18% |
| 12.1-15.0 |
6% |
| >15 |
3% |
Tab. 4. Range of AMH levels in PCOS women.
| Risk-factor |
p-value |
Coefficient |
Remarks |
| Duration of period cycle |
p<0.001 |
1.404 |
Significant |
| Flow in menses |
p<0.001 |
1.608 |
Significant |
| History of Diabetes Mellitus |
p<0.001 |
1.005 |
Significant |
| History of Hypertension |
p<0.001 |
1.004 |
Significant |
| History of thyroid |
p<0.001 |
1.03 |
Significant |
| Family history of diabetes mellitus |
p<0.001 |
1.013 |
Significant |
| Family history of hypertension. |
p<0.001 |
1.079 |
Significant |
| Family history of thyroid issues |
p<0.001 |
1.034 |
Significant |
| Gynecological history in mother/sisters |
p<0.001 |
1.393 |
Significant |
| Caffeinated drinks |
0.304 |
0.52 |
Non-significant |
| Junk-food habits |
0.763 |
0.593 |
Non-significant |
| Physical exercise |
0.293 |
0.682 |
Non-significant |
| Body Mass Index (BMI) |
p<0.001 |
1.132 |
Significant |
Tab. 5. Chi-square analysis.
Duration of the period cycle
• Junk-food habits
• Flow in menses
• Physical exercise
• History of diabetes mellitus
• Body mass index (BMI)
• History of hypertension
• History of the thyroid
• Family history of diabetes mellitus
• Family history of hypertension
• Family history of thyroid issues
• Gynecological history in mother/sisters
• Tea-drinking habits
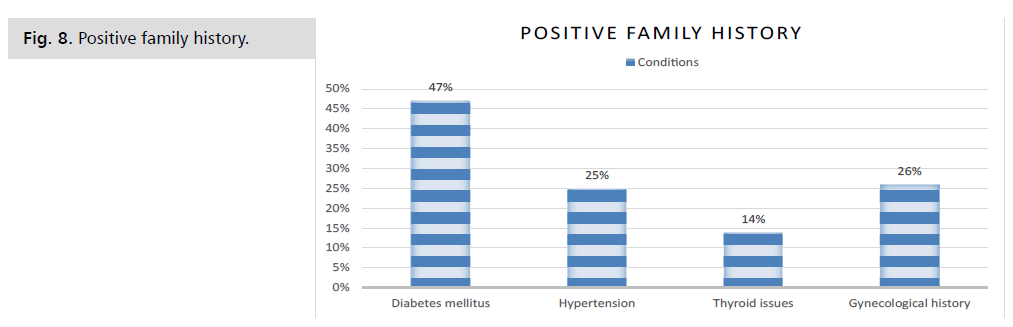
As per the significance value calculated by the Chisquare
test, the duration of the period cycle has a direct
effect on the serum AMH levels, and therefore, on the
occurrence of PCOS. The p<0.05 and the correlation
coefficient was 1.404. This shows that the irregular
menstrual cycle accounts for the occurrence of PCOS.
The cycles are considered to be irregular if the number of
days is 30 ± 7 days. Most women who had elevated AMH levels also had a history of irregular cycles. Similarly, the
menstrual flow was also significant to AMH changes in
PCOS women (Fig. 1-8). The p-value was p<0.05 and
the correlation coefficient was 1.608. Most women with
PCOS had scanty flow during their menses. Some even had
spotting. History of disorders like hypertension, diabetes
mellitus, and thyroid are also significant to PCOS. It
was found that women, who had these conditions, were
at a higher risk of development of PCOS, as they all had
a significant correlation with serum AMH levels. The
percentage of women who had diabetes mellitus was 4%,
3% of women were hypertensive and 24% of women had
thyroid issues.
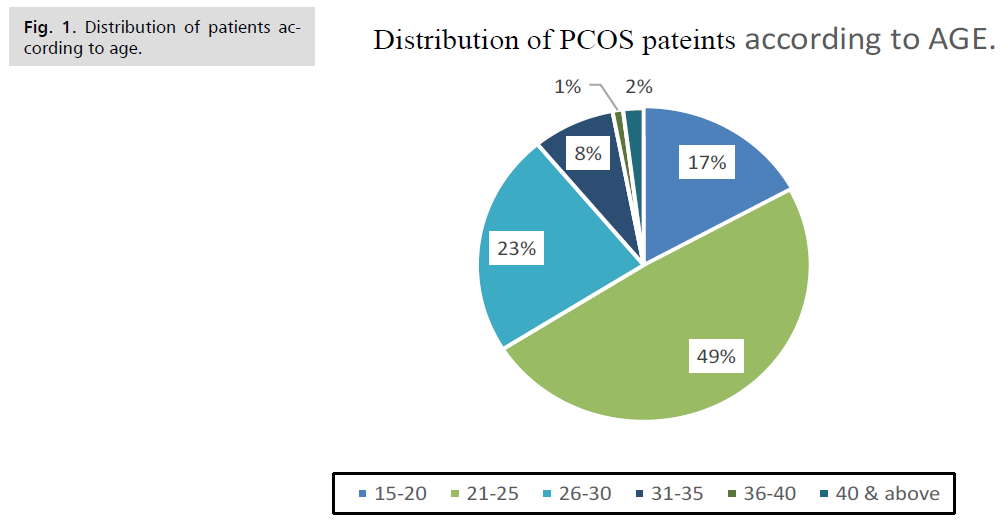
Figure 1: Distribution of patients according to age.
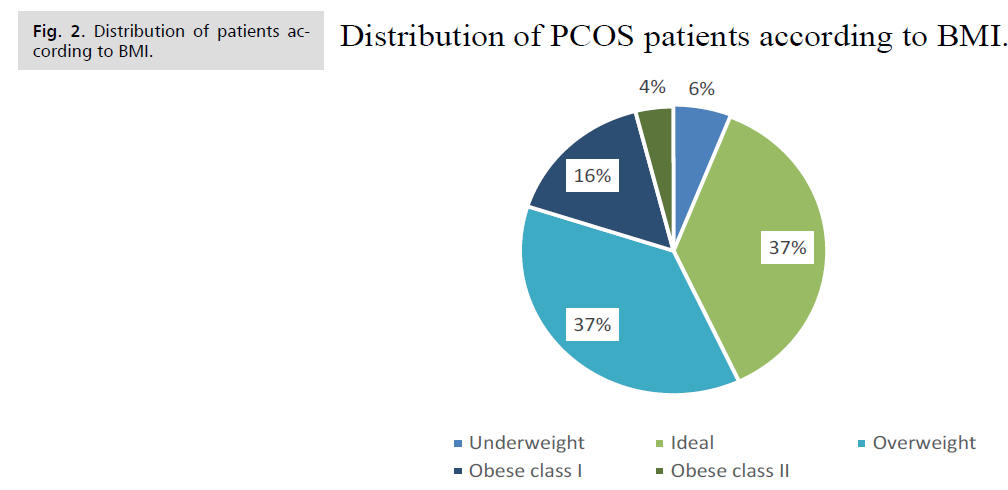
Figure 2: Distribution of patients according to BMI.
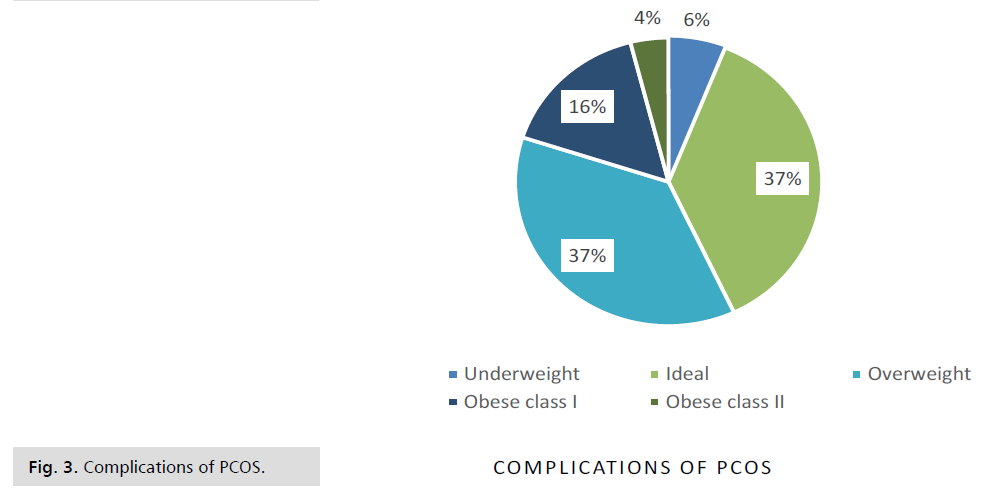
Figure 3: Complications of PCOS.
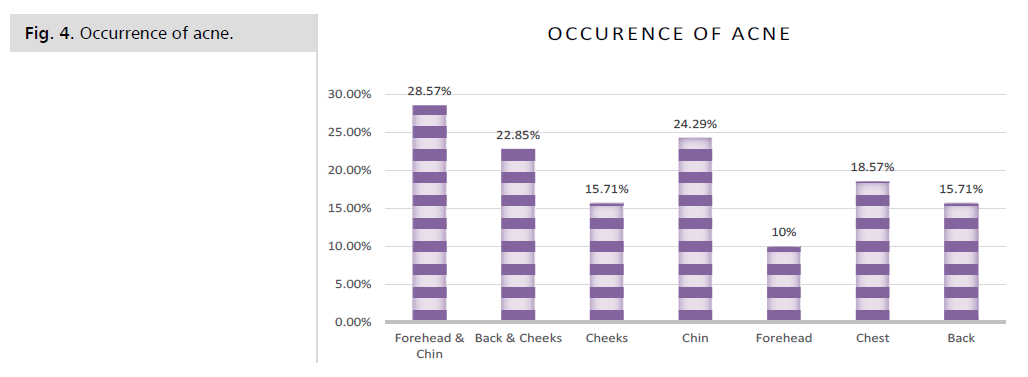
Figure 4: Occurrence of acne.
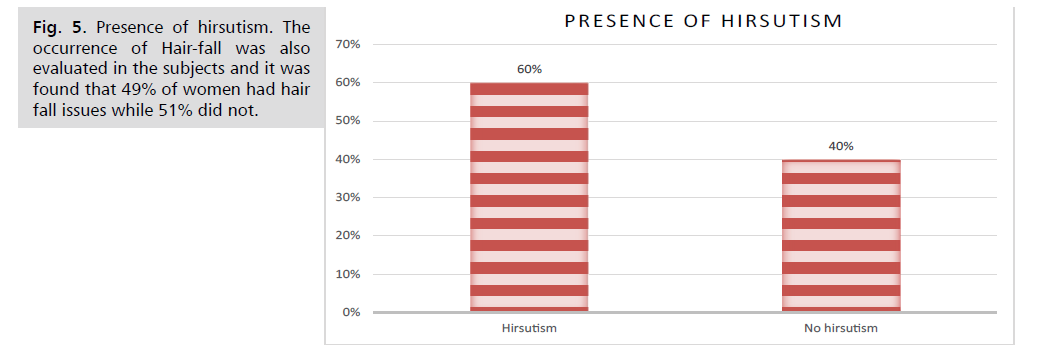
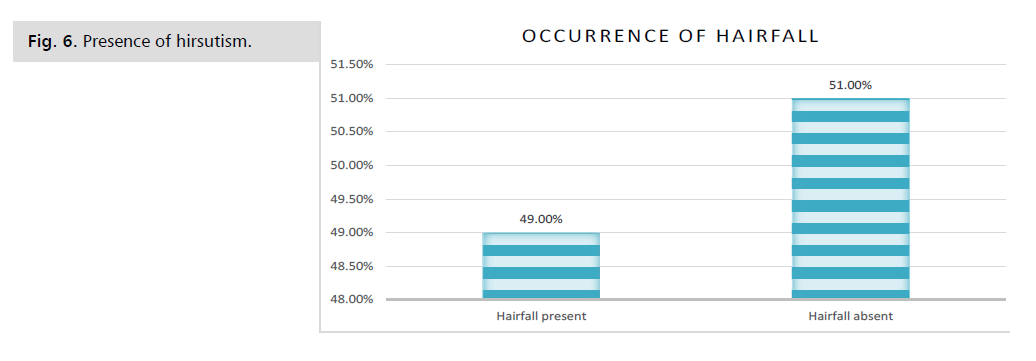
Figure 5: Presence of hirsutism. The occurrence of Hair-fall was also evaluated in the subjects and it was
found that 49% of women had hair fall issues while 51% did not.
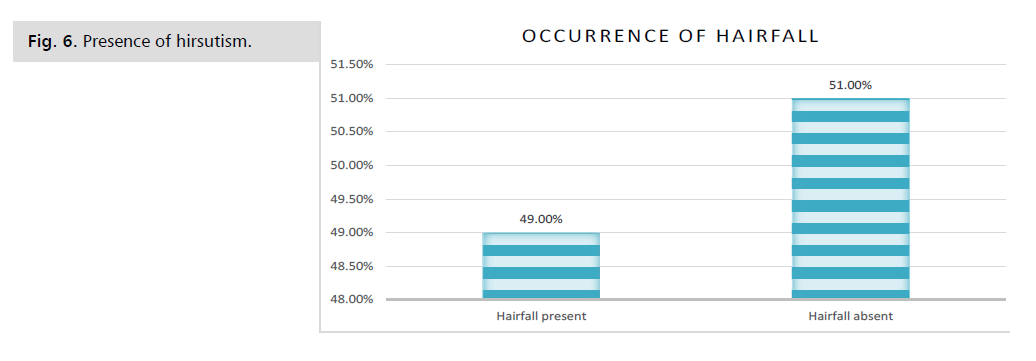
Figure 6: Presence of hirsutism.
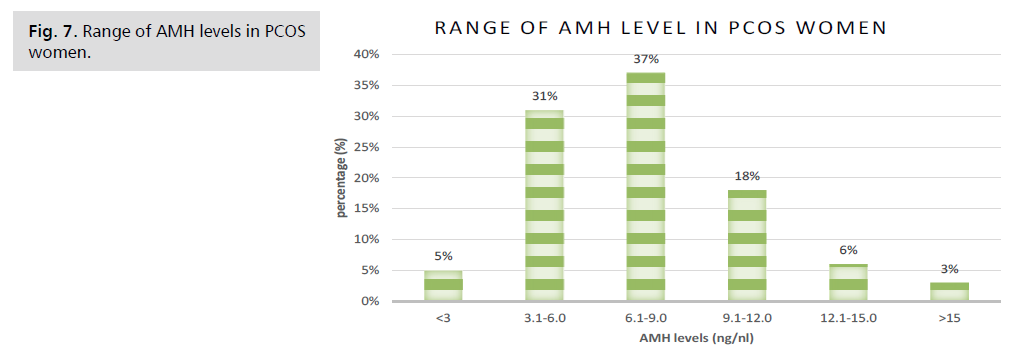
Figure 7: Range of AMH levels in PCOS women.
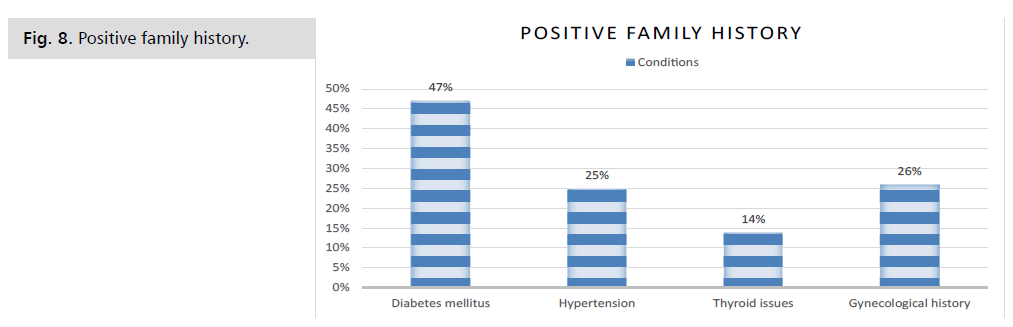
Figure 8: Positive family history.
Discussion
Beyond The association between obesity and COVID-19
can be assessed in various aspects. First obesity causes
respiratory system dysfunctions like decreased chest wall
elasticity (fat in the abdomen pushes up on the diaphragm,
which presses on the lungs and restrict airflow) lung
compliance, and expiratory reserve volume (this reduced
lung volume causes collapse of airways in the lower lobes of
the lungs, where more blood arrives for oxygenation than
in the upper lobes) [7]. Second, obesity is associated with
disorders such as type 2 diabetes mellitus, atherosclerosis,
cardiovascular diseases, hypertension and cancer [8].
Which are also identified as risk factors for COVID-19.
These comorbidities may exacerbate COVID-19 and
increase the probability of hospitalization in the intensive
care unit (ICU) and also increase mortality [9]. Third, it leads to hyper coagulopathy state and hyper inflammation,
and it is well known that venous thromboembolism is
a complication of severe COVID-19 infection as well,
thus these 2 conditions when present together produce hypercoagulability and thromboembolism in a synergistic
way. Inflammatory markers such as IL-6 and C-reactive
protein are increased in obese patients [10,11]. These may
become so severe that they can cause clots in vital organs and cytokine storm. In all these 3 conditions, the disease is
severe and the risk of admission to the ICU and mortality
is high. On the other hand, COVID-19 also has an impact
on obesity as it increases social constraints and impedes mobility, which thus increases the weight and prevalence
of obesity in society, and this gives way to a vicious cycle
that is repeated all over again and again. Although there are
ample advantages of bariatric surgery in the COVID-19
patient, there are certain limitations that are worthy of
mention. Bariatric surgery, specifically bypass surgery, is
likely to have an effect on the absorption of medications
that are administered orally to COVID-19 patients. In case
of hydroxychloroquine, a case report of three post-RYGB
(Roux-en-Y procedure) patients with autoimmune disease
was done (taking standard hydroxychloroquine doses), all
three patients had sub therapeutic hydroxychloroquine
blood levels and active disease; it was only after increasing
their doses above the recommended 400 mg/day dosing
that they were able to have therapeutic drug levels as
well as better disease control. Thus hydroxychloroquine
has inadequate absorption post-RYGB (and potentially
other bariatric procedures), and COVID-19 bariatric
patients may need higher doses of hydroxychloroquine
than recommended [12]. For azithromycin a single-dose
pharmacokinetic study involving 14 post-gastric bypass
patients showed that bioavailability was reduced by 1/3rd
in gastric bypass patients, when compared with matched
controls [13]. Since maximal absorption of azithromycin
occurs in proximal gut. During RYGB (Roux-en-Y
procedure) the stomach is dissected, that leads to less acidic
gastric pouch. Azithromycin with its basic nature (alkaline;
pKa=8.5) and low water solubility, the dissolution of the
large (500 mg) drug dose of azithromycin can be severely
affected post-surgery thus affecting the absorption and
bioavailability of azithromycin. In case of corticosteroids,
the pharmacokinetics of dexamethasone and related steroids
may be affected especially post-gastric bypass surgery. These
drugs are mainly absorbed via the proximal gut which is
hampered during the bariatric procedure. These are some
of the limitations of the bariatric surgery procedure that
need to be considered in a COVID-19 patient.
Conclusion
In In conclusion, the present study suggests that PCOS
is an emerging health concern among reproductive women
and is associated with many consequences like menstrual
irregularities, hirsutism, acne, alopecia, and infertility,
which were common endocrine disorders. Family history
of diabetes and hypothyroidism were important risk factors
associated with PCOS. Women who were overweight/ obese were at a higher risk of developing PCOS. History of
menstrual irregularities and PCOD/PCOS in mother and
sisters of women also had significance in the occurrence of
PCOS. Special attention should be paid to overweight and
obese girls as they were having the highest possibility of
PCOS but it could be treated by lifestyle modification. Thus,
early detection of the syndrome based on clinical findings
(mainly oligo- or amenorrhea) offers an opportunity
for early intervention to prevent or limit the impact of
cutaneous and reproductive symptoms, and the long-term
effects of metabolic disturbances. Further, the emerging
role of Anti-Mullerian Hormone should be recognized
in the diagnosis of PCOS along with other suggestive
features. AMH levels are the most reliable measure of
follicle count in the ovaries. In PCOS, the ovaries fail to
select a dominant follicle to ovulate and a number of small
follicles are developed, which are filled with fluid and are
called cysts. These cysts produce AMH and so the levels of
AMH increases in PCOS. AMH levels will provide reliable
information in diagnosing PCOS and should be used in
future along with Rotterdam or NIH criteria. Awareness
of earlier diagnosis of PCOS and interventions must be
increased among health care providers and adolescent girls
because it could provide an opportunity to treat this disease
and prevent future morbidities.
Conflicts of Interest
All authors declare that they have no conflict of interest.
Data Availability
All data generated or analyzed during study are included
in this review.
Funding
The study was not funded by any person/organization.
Acknowledgments
Upon completion of our project work, it is a pleasure to
utilize the opportunity of acknowledging all those people
who have helped in accomplishing our project. Foremost,
we want to offer this endeavour to our God Almighty for
the wisdom he bestowed upon us, the strength, peace of
mind and, good health to finish this project.
We would like to express our sincere regards to Shri
Mahant Devendra Das Ji Maharaj, Chancellor, Shri Guru
Ram Rai Education Mission, Dehradun, Uttarakhand, for
providing us the facilities required for the project work.
We are immensely grateful to our supervisor, Dr Prashant
Mathur, Professor & HOD, Dept. Of Pharmacy Practice,
SGRRITS for his guidance, patience, insightful comments,
helpful information, and ideas that helped us at all times in
our research and writing of this thesis. We would also like
to express our thanks to our Co-supervisor, Mrs. Monika,
Assistant Professor, School of Pharmaceutical Sciences,
SGRRU for her guidance and support. We are immensely
grateful to Dr Arti Sharma, Professor, Dept of Obs &Gynae
and Dr Anjali Chaudhary, Professor, Obs & Gynae,
SGRRIM & HS, Dehradun for their constant support as
our Co-Supervisors. Their immense knowledge, profound
experience, and professional expertise in Gynae-Obs
have enabled us to complete this successfully. We express
our sincere gratitude to our Vice-Chancellor Prof (Dr) U.S Rawat and Dr Alka N Choudhary, Dean, School of
Pharmaceutical Sciences, SGRRU, Dehradun for providing
us the facilities to complete our work and all the faculty and
staff members of Department of Pharmaceutical Sciences,
SGRRU for their support throughout our thesis work.
Our heartfelt gratitude goes to Medical Superintendent of
SMI Hospital, Dr Anil Kumar Dhawan Sir for granting
us permission to sit in the OPD to collect our cases. We
are very much thankful to Dr Monika Ramola, Dr Neeta
Bansal and all the PG students of Gynae & Obs for guiding
and helping us with our work. We also thank Attendant
Sanju, Beena and Indu for providing us the instruments
and other requirements for our work. Our thanks and
appreciation also goes to all our friends and colleagues who
have willingly helped us out with their abilities. We owe a
big thanks to our parents, without their love and support
this project would not have been completed.
REFERENCES
- Witchel SF, Oberfield SE, Peña AS. Polycystic ovary syndrome: pathophySiology, presentation, and treatment with emphasis on adolescent girls. J Clin Endocrinol Metab.2019; 3:1545-1573.
Google Scholar, Crossref, Indexed at
- Macut D, pfeifer M, yildiz O, et al. Polycystic ovary syndrome novel insights into causes and therapy preface.Polycystic ovary syndrome: Novel insight into causes and therapy. Front Horm Res. Basel.2013; 40:1-21.
Google Scholar, Crossref, Indexed at
- Adam Balen. “ The pathophysiology of polycystic ovary syndrome: Trying to understand PCOS and its endocrinology.” Best Pract Res Clin Obstet Gynaecol. 2004;18:685-706.
Google Scholar, Crossref, Indexed at
- Sirmans SM, Pate KA. Epidemiology diagnosis and management of polycystic ovary syndrome. Clin Epidemiol.2014; 6:1.
Google Scholar, Crossref, Indexed at
- Broekmans FJ, Knauff EA, Valkenburg O, et al. PCOS according to the Rotterdam consensus criteria: change in prevalence among WHO‐II anovulation and association with metabolic factors. BJOG.2006;113:1210-1217.
Google Scholar, Crossref, Indexed at
- Artini PG, Di Berardino OM, Simi G, et al. Best methods for identification and treatment of PCOS. Ginecol. 2010; 62:33.
Google Scholar, Crossref
- Visser JA, de Jong FH, Laven JS, et al. Anti-Mullerian hormone: a new marker for ovarian function. Reproduction. 2006;131:1-9.
Google Scholar, Crossref
- Josso N, Cate RL, Picard JY, et al. Anti-Müllerian hormone: The Jost factor. Recent Prog Horm Res. 1993:1-59.
Google Scholar, Crossref, Indexed at
- Pigny P, Merlen E, Robert Y, et al. Elevated serum level of anti-mullerian hormone in patients with polycystic ovary syndrome: Relationship to the ovarian follicle excess and to the follicular arrest. J. Clin Endocr. 2003; 88:5957-5962.
Google Scholar, Crossref, Indexed at
- Durlinger AL, Gruijters MJ, Kramer P, et al. Anti-Mullerian hormone attenuates the effects of FSH on follicle development in the mouse ovary. Endocrinol. 2001;142:4891-4899.
Google Scholar, Crossref, Indexed at
- Jena SK, Mishra L, Naik SS, et al. Awareness and opinion about polycystic ovarian syndrome (PCOS) among young women: A developing country perspective. Int J Adolesc Med Health. 2021;33:123-126.
Google Scholar, Crossref, Indexed at
- Joshi B, Mukherjee S, Patil A, et al. A cross-sectional study of polycystic ovarian syndrome among adolescent and young girls in Mumbai, India. Int J Adolesc Med Health. 2014;18:317.
Google Scholar, Crossref, Indexed at
- De Leo V, Musacchio MC, Cappelli V, et al. Genetic hormonal and metabolic aspects of PCOS: An update. Reprod Biol Endocrinol. 2016;14:1-7.
Google Scholar, Crossref
- Hachey LM, Kroger-Jarvis M, Pavlik-Maus T, et al. Clinical implications of polycystic ovary syndrome in adolescents. Nurs Women's Health. 2020;24:115-126.
Google Scholar, Crossref
- Bahadur A, Mundhra R, Kashibhatla J, et al. Prevalence of metabolic syndrome among women with different PCOS phenotypes–a prospective study. Gynecol Endocrinol. 2021;37:21-25.
Google Scholar, Crossref, Indexed at
- Damone AL, Joham AE, Loxton D, et al. Depression, anxiety, and perceived stress in women with and without PCOS: a community-based study. Psychol Med. 2019;49:1510-1520.
Google Scholar, Crossref, Indexed at
- DokrasAnuja, Sarwer B David, Allison Kelly, et al. “Weight Loss and lowering androgens predict improvements in health-related quality of life in women with PCOS. J Clin Endocr. 2016;10:2966-2974.
Google Scholar, Crossref, Indexed at
- Thannickal A, Brutocao C, Alsawas M, et al.Eating, sleeping and sexual function disorders in women with polycystic ovary syndrome (PCOS): A systematic review and meta‐analysis. Clin Endocrinol. 2020;92:338-349.
Google Scholar, Crossref, Indexed at
- Bharathi RV, Swetha S, Neerajaa J, et al . An epidemiological survey: Effect of predisposing factors for PCOS in Indian urban and rural population. Middle East Fertil Soc J. 2017;22:313-336.
Google Scholar, Crossref, Indexed at
- Sahmay S, Mathyk BA, Sofiyeva N, et al. Serum AMH levels and insulin resistance in women with PCOS. Eur J Obstet Gynecol Reprod Biol. 2018;224:159-164.
Google Scholar, Crossref, Indexed at