Keywords
Africa, Breast cancer, Late presentation, Delayed diagnosis
Background
Breast cancer is becoming a major public health challenge in Africa and most countries do not have cancer registries, nevertheless, the World Health Organisation estimates that the incidence rate of breast cancer in Africa has steadily increased over the years [1]. There is also a higher mortality or a poorer survival rate among breast cancer patients in most African countries [2]. For example, the five year survival rate of breast cancer in Gambia is 12.5% [3]. Similarly, the incidence of breast cancer in Ghana is estimated to be 25 cases per 100,000 population compared to 93 per 100,000 in the USA but the mortality is 12 per 100,000 in Ghana compared to 15 per 100,000 in the USA [4].
Healthcare in Africa is delivered through orthodox and unorthodox systems. The orthodox healthcare system is made up of a majority public sector and a minority private sector. The public sector, which is usually financed by government, provides most of the basic and secondary healthcare as well as highly specialised health services in the teaching hospitals. As a consequence of political unrest, corruption, and economic situations in most African countries, the public sector is poorly resourced and managed. In Tanzania, 30% of the country’s healthcare professionals leave the health sector after receiving medical training because of poor incentives [5] and this situation may not be different from other African countries. It was reported that Zambia has less than 646 doctors and 6,096 nurses in a population of 15,526,871 [6]. Nevertheless, some countries, such as South Africa, Ghana, and Egypt, notwithstanding ongoing challenges, are making progress in strengthening their public healthcare system [7]. The private sector, which forms the minority in most African countries is operated by individuals, non-governmental organisations, and faith-based organisations. The healthcare facilities operated by individuals or non-governmental organisations are mostly accessed by the middle and high-income earners because of the high cost of services. The less privileged in society are unable to afford their services. Hospitals and health centres run by faithbased organisations have been reported to provide a significant portion of care in most African countries, usually reaching rural areas and underserved populations with subsidised cost of healthcare [8]. Unorthodox, or traditional healthcare systems, consist of spiritual therapies by priests and priestesses, herbal medicines, rituals, occultism and many others. Almost 80% of Africans use unorthodox healthcare [9]. Unorthodox medical services are easily accessible to all, including the poor, with highly committed and influential practitioners.
It is unsurprising, therefore, that many women with breast cancer present late and with advanced disease to orthodox healthcare systems.
Extensive reviews on factors influencing delay have been undertaken in developed countries, enabling them to implement policies to minimise late presentation or delayed diagnosis of breast cancer [10-14]. However, in Africa no review has been done. Knowledge about delay in breast cancer is based on assumptions and single studies; indicating a need for a comprehensive review. This study provided a review of studies focusing on patientrelated factors or reasons contributing to the late presentation or delayed diagnosis of breast cancer in Africa. The study aim was to answer the research question ‘what are the patients’-related factors contributing to the late presentation or delayed diagnosis of breast cancer in Africa?’
Methods
This review was conducted in line with the Methodological Guidelines for Review Papers as described by Weed [15]. The review involved the following major stages: literature search, articles selection, data extraction, data analysis/synthesis and critical appraisal of included articles.
Literature search
A systematic search of peer-reviewed, published literature in English from 1990 to 2014 was conducted between 7th April 2014 and 18th July 2014 to identify the factors contributing to the late presentation or delayed diagnosis of breast cancer in Africa. The following selected electronic databases were searched; African Index Medicus (AIM) hosted by the World Health Organisation, Cumulative Index to Nursing and Allied Health Literature (CINAHL) hosted by EBSCO, Medical Literature On-Line (MEDLINE) hosted by EBSCO, Web of Science and Psychology Information (PsycINFO) hosted by EBSCO. These electronic databases were selected because of the wide range of academic disciplines they cover and their credibility as well as those most likely to be publishing about issues relevant to Africa. The terms used were “Breast Neoplasms” AND “Late Presentation” OR “Delayed Diagnosis” AND “Africa” OR “the name of any of the African countries”. Additional hand searching of reference lists of included articles was conducted.
Article selection and data extraction
Articles were selected based on pre-defined inclusion and exclusion criteria. Articles were included in the review if only they were primary evidence, published in English between 1990 and 2014, conducted in any of the African countries, all or a majority of the participants were female breast cancer patients and focused on patient-related factors contributing to the late presentation or delayed diagnosis of breast cancer. Articles were excluded if they were expert opinions or commentaries, unpublished articles or studies not published in English.
Initially, titles and abstracts of articles identified through the electronic database search were scrutinised and included or excluded based on the pre-defined selection criteria. Full manuscripts of studies meeting the inclusion criteria were retrieved. Hand searching of reference lists to identify other relevant studies was performed on the included studies from the electronic databases searched. Similarly, full manuscripts of studies identified through hand searching of reference lists were also retrieved. Articles that did not meet the inclusion criteria were eliminated. Discussion meeting was organised with research team to settle any disagreement.
Data analysis and synthesis
Given the heterogeneity of the studies included in the review, a meta-analysis was not feasible. These studies had different sample sizes (from 66 to 535) and analytic approaches (simple descriptive to bivariate designs). It was therefore decided to conduct a narrative analysis of the data. Thematic synthesis was conducted as described by Dixon-Woods et al. [16]. Discrepancies on the themes were discussed among authors AD, JL and SW, and consensus was reached.
Critical appraisal of included studies
The included studies were critically appraised using the appraisal tool developed by Coughlan et al. [17]. The studies were assessed for their reliability and validity, the two crucial aspects of the quality of a quantitative research. The reliability of a quantitative research is associated with the consistency, repeatability, reproducibility, stability, agreement, and homogeneity. However, the validity is how well a study or an instrument measures what it professes to measure [18].
The included studies came from varied backgrounds, all the authors of the included studies were qualified enough to ask credible questions associated with the late presentation or delayed diagnosis of breast cancer based on their educational background. The professional background of the authors’ ranged from general practitioners, surgeons, medical oncologists, medical statisticians, nurses to epidemiologists. However, none of the studies used a theoretical framework. All the studies were quantitative design with small sample sizes. Similarly, all the studies used a non-probability sampling method which maybe have introduced selection bias. Also, all the studies were hospital based with a retrospective information, hence a high potential of recall bias. Authors also failed to use validated standardised questionnaires. Therefore, both internal and external validity of the questionnaires used are debatable. However, majority of the authors used a bivariate analysis, so they were unable to report on the statistical significance and clinical relevance of variables such as age, employment status, marital status, religious status and educational status.
Despite the reliability and validity issues identified within the studies, they provided significant information regarding reasons why African women delay in seeking medical help after noticing symptom of breast cancer. Future studies should utilise qualitative study design based on theories such as, sociocultural, trust, cognitive-behavioural and health belief models, and be conducted across multiple sites so that appropriate comparisons can be made across nations.
Results
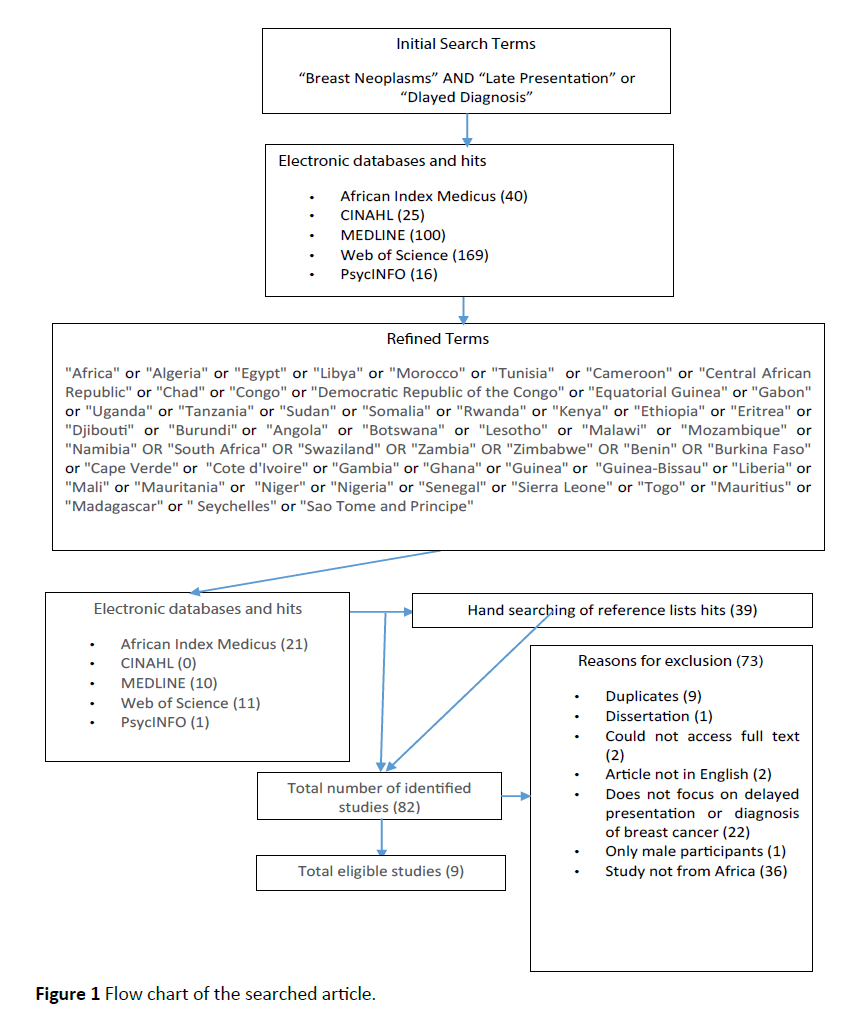
The literature search yielded eighty-two publications (Figure 1). Articles were screened and excluded for the following reasons: duplicates (9), dissertation (1), could not access full text (2), article not in English (2), does not focus on delayed presentation or diagnosis of breast cancer (22), only male participants (1) and study not from Africa (36). A total of nine studies were included in this review. Three studies were conducted in Egypt [19-21], three in Nigeria [22-24], one in Ghana [25], one in Kenya [26] and one in Libya [27]. Tables 1 and 2 summarises the characteristics of the included studies. Six themes were identified – negative symptom interpretation (unserious, absence of pain and ignorance), fear (fear of cancer, surgery, embarrassment, divorce and death), belief in alternative medicine (local and foreign based therapies), social relations and networks (social influence and social control), lack of trust and confidence in orthodox medicine, and access to healthcare (physical access and economic access).
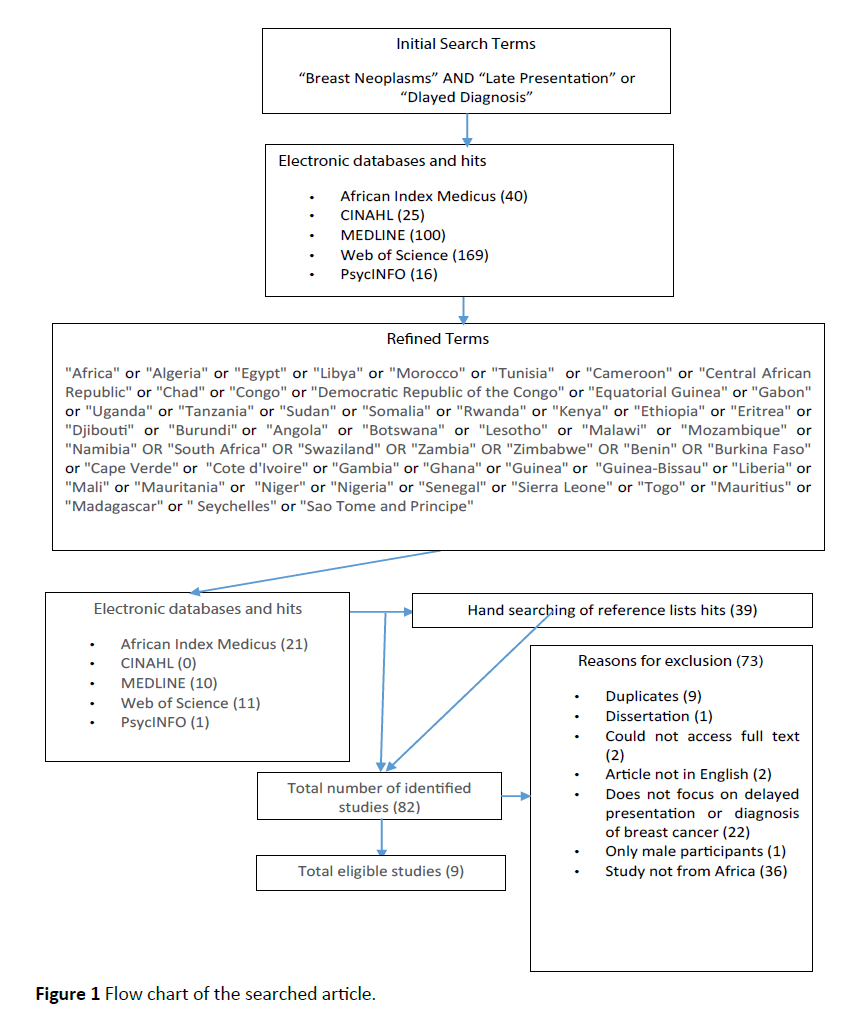
Figure 1 Flow chart of the searched article.
| Authors (year) |
Study aim |
Location,
Sample size (N) |
Type of study |
Data collection methods |
Data collection duration |
| Stapleton et al. [19] |
To investigate patient-mediated determinants for the late-stage presentation of breast cancer |
Egypt (Chemotherapy outpatient clinic) N=343 |
Quantitative |
Face-to-face patient interview using a structured questionnaire |
July 2007-August 2008 |
| Ismail et al. [20] |
To assess factors that hinder early detection of breast cancer in females |
Egypt (Surgical outpatient and inpatient clinic) N=120 |
Quantitative |
Face-to-face patient interview using a structured questionnaire |
March 2012-August 2012 |
| Abdel-Fattah et al. [21] |
To evaluate the avoidable risk factors related to diagnostic delay of breast cancer |
Egypt (Patients on hospital admission) N=565 |
Quantitative |
Face-to-face patient interview using a pre-coded standardized forms |
July 1997-June 1998 |
| Ezeome et al. [22] |
To assess the delays and define the causes of delay in presentation and treatment of breast cancer patients in Enugu, Nigeria |
Nigeria (Surgical Oncology outpatient) N=164 |
Quantitative |
Face-to-face patient interview with a semi-structured questionnaire |
June 1999-May 2005 |
| Ibrahim and Oludara[23] |
To evaluate the effects of selected socio-demographic factors on late presentation and reasons why breast cancer patients delay reporting for treatment. |
Nigeria (Surgical outpatient clinic)N=201 |
Quantitative |
Face-to-face patient interview using a structured questionnaire |
January 2009-December 2010 |
| Ukwenya et al. [24] |
To investigate the extent and reasons for the delay between onset of symptoms and admission for treatment of symptomatic breast cancer |
Nigeria (Patients on hospital admission) N=111 |
Quantitative |
Face-to-face patient interview with a structured open-ended questionnaire |
July 2003-June 2005 |
| Clegg-Lamptey et al. [25] |
To determine the causes of delayed presentation in breast cancer patients |
Ghana (Surgical outpatient clinic) N=66 |
Quantitative |
Face-to-face patient interview with a structured questionnaire |
September 2007-July 2008 |
| Otieno et al. [26] |
To determine the extent and nature of delayed presentation of patients treated for breast cancer |
Kenya (Surgical wards and breast clinic) N=166 |
Quantitative |
Face-to-face patient interview using a structured questionnaire |
October 2003-March 2006 |
| Ermiah et al. [27] |
To study the diagnosis delay and its impact on stage of disease among women with breast cancer |
Libya (Outpatient clinic) N=200 |
Quantitative |
Face-to-face patient interview using a structured questionnaire |
January 2008-December 2009 |
Table 1: Description of included studies.
| Themes |
Sub-themes |
Factors from included studies |
| Negative symptom interpretation |
Absence of pain
Unserious
Ignorance |
No pain[19];
Lack of awareness about breast cancer, denied having breast cancer and thought it was only a simple mass which would go away[20];
Underestimation of the importance of the presence of a breast lump, ignorance[21];
Did not consider it serious/hope it will disappear, ignorance, painless, thought it was pregnancy/effect of lactation, no ulcer[22];
Ignorance of the nature of illness, no pain[23];
Patient not aware of seriousness of a lump in the breast[24];
Ignorance[25];
Painless lump, not aware of the disease [26];
Symptoms not considered serious[27] |
| Fear |
Fear of cancer
Fear of surgery
Fear of embarrassment
Fear of divorce
Fear of death |
Fear of cancer, fear of divorce, fear of embarrassment [20];
Fear to seek medical advice[21];
Fear of surgery/breast removal, fear she will die, fear because her elder sister had breast cancer [22];
Fear of mastectomy[23];
Did not want mastectomy as treatment[24];
Fear of diagnosis, fear of mastectomy[25];
Worried they would be diagnosed with cancer[26];
Fear, fear of shame[27] |
| Belief in alternative medicine |
Local based therapies
Foreign based therapies |
Alternative treatment or prayer[22];
Belief in spiritual healing, belief in herbal treatment [23];
Alternative (traditional/spiritual) treatment[24];
Herbal treatment, food supplements, homeopathy, Chinese medicine/acupuncture, organic foods[25];
Alternative and complementary medicine use[26];
Alternative therapy[27] |
| Social relations and networks |
Social influence
Social control |
Social[19];
Was preoccupied by family/domestic/social problems, discouraged by friends and relations [22];
Family refused hospital treatment[24] |
| Lack of trust and confidence in orthodox medicine |
|
False reassurance by medical doctor as a benign tumour, seeking different opinion [22];
Reassurance by non-medical health worker[23];
Searching for appropriate hospital/doctor, industrial action by teaching hospital/lab test delay[25];
Reassurance that the condition was benign[26]; |
| Access to healthcare |
Physical access
Economic access |
Financial and time constraints, longer travel time [19];
Financial problems[20];
Financial problem[22];
Lack of funds[23];
Could not initially afford hospital treatment[24];
Financial incapability[25] |
Table 2: Factors contributing to late presentation of breast cancer among african women.
Discussion
This review is the first to be conducted to assess patient-related factors contributing to the late presentation or delayed diagnosis of breast cancer among African women. The findings of the review provide different understanding about patient-related factors of late presentation or delayed diagnosis of breast cancer. The review identified that there was no single specific factor, but rather a complex integration of factors contributed to the late presentation or delayed diagnosis of breast cancer among African women. These complex factors were negative symptom interpretation, fear, belief in alternative medicine, social relations and networks, lack of trust and confidence in orthodox medicine, and access to healthcare.
Negative symptom interpretation: According to Teel et al. symptoms are signals or body changes that individuals observe about themselves. Symptom interpretation is a cognitive process, and an integral factor for initiating actions. A positive symptom interpretation may initiate help seeking behaviour while a negative symptom interpretation may result in ignoring seeking help.
All the nine studies included in the review identified negative symptom interpretation as a factor for delayed presentation [19-27]. From the review, there were three sub-themes identified under negative symptom interpretation-absence of pain, unserious, and ignorance. Ermiah et al. reported that 27.0% of the participants delayed because they perceived that their symptoms were not serious [27]. Similarly, Ezeome acknowledged that 27.8% of breast cancer patients delayed because they believed that symptoms would disappear over time. Also, 3.2% of breast cancer patients were not keen to seek medical help for a trivial breast abnormality that could be due to pregnancy or lactation [22]. However, a higher percentage (47.5%) was stated by Ukwenya for patients not considering symptom to be serious [24]. Symptoms were considered to be serious based on preconceived thought about the nature of breast cancer, that is, the presence of cancer in the breast should cause pain. In Nigeria and Kenya, 12.0% and 23.5% of breast cancer patients respectively delayed because the lump they noticed was painless [22,26]. In addition, individuals (breast cancer patients) could not interpret the symptom because they were ignorant about the breast cancer signals [21-23,25,26]. Although patient ignorance was a regional issue, studies from Nigeria reported a higher percentage of ignorance among breast cancer patients. For example, Ezeome, and Ibrahim and Oludara reported 23.3% and 34.1% respectively [22,23]. However, in Kenya only 7.8% of breast cancer patients delayed because of ignorance [26].
From the current review, it is clear that women have difficulties in identifying or recognising symptoms of breast cancer resulting in the negative symptom interpretation of any breast abnormality. According to Burgess et al. women mostly keep their symptoms under personal review. In contrast to African women, most European women are able to recognise symptom changes and they take action by seeking medical help. This indicates that knowledge about breast cancer symptoms is an important factor in initiating contact with a healthcare professional after identifying breast abnormalities.
Fear: Fear is a unique emotional state of an individual. According to Barlow et al., fear is an instantaneous reaction to a threat or danger, which is characterised by desires to escape [27]. In most African countries, the disastrous nature of breast cancer is intensified because of poor or limited resources, such as radiotherapy facilities, resulting in increased mortality rate [28]. Therefore, cues of breast cancer trigger different forms of fear.
From the review, fear was the major contributing factor causing late presentation or delayed diagnosis of breast cancer in Africa. All but one of the nine studies included in the review identified fear as a factor for delayed presentation [20-27] In Kenya, 19.9% of breast cancer patients presented late, mainly because of fear that they will be diagnosed with cancer [26]. Heterogeneous statistics of fear were found in West Africa: from 6.8% to 29.3% in Nigeria [22-24] compared to 34.8% in Ghana [25]. On the other hand, in the United Kingdom, only 4.9% of breast cancer patients considered fear to be a reason for late presentation or delayed diagnosis [29]. This may be due to government initiatives and cancer survivor groups embarking on numerous campaign which in Africa, hardly or barely exist. Most importantly, the few breast cancer survivors are reluctant to share their experiences openly because of stigmatisation, embarrassment, and superstition undermining survivors’ self-worth, positive self-image, and sense of completeness.
Fear is embedded in defence, for example individuals are more likely to fear events and conditions that caused threats to the survival to themselves and to friend or relative [30]. These events leave thoughtful imprints. Basic logic should have been protection and early presentation to avoid any unwanted outcomes, but fear stimulation is less vital in motivating precautionary action [31]. This explains why most women avoid clinical breast examination and early medical help even though they are aware of the seriousness of breast cancer and rather focus on different issues. Ezeome reported that 5.6% of the breast cancer patients avoided visiting a healthcare professional because they preoccupied themselves with family, domestic, and social problems after observing breast cancer symptoms [22].
There is overwhelming evidence in the field of oncology supporting fear as a contributing factor to the late presentation or delayed diagnosis of cancer [32,33]. From the review, fear of cancer, surgery, embarrassment, divorce, and death were identified. Three of these fears, fear of death, embarrassment, and divorce can also be called ‘fear of cancer outcome’. Globally, being diagnosed of breast cancer is bad news and associated with high rates of morbidity and mortality, hence the majority of people do not want to know the medical diagnosis of any observed breast abnormalities. Otieno et al. noted that several breast cancer patients delayed because they were worried they would be diagnosed of cancer [26]. Fear of surgery, tomophobia is mainly caused by previous personal or a relative’s surgical ordeal [34]. From the review, individuals were afraid that mastectomy would leave a dreadful cosmetic deformity, lymphedema, arm pain, chest tightness, financial burden, and sexuality issues, which could result in divorce, and embarrassment. However, studies from Europe have shown that divorce is not associated with breast cancer diagnosis and rather experienced increased intimacy and support [35,36] compared to what pertains in Africa.
Belief in alternative medicine: Globally, complementary and alternative medicine is common amongst cancer patients with numerous reasons for its usage [37-40]. Six studies identified the use of alternative medicine as a reason for women delaying seeking medical help and presenting late [22-27]. Two forms of alternative medicine were identified in the review – local based therapies (spiritual/prayer/traditional healer/herbal therapy), and foreign-based therapies (acupuncture/homoeopathy/Chinese medicine) [22-27]. Regional trends of alternative medicine use were also observed, related to spirituality, and cultural diversity. The highest use of alternative medicine was found in studies from West Africa. According to Ibrahim and Oludara, 61.6% of the participants relied mainly on alternative medicine after detecting breast cancer symptoms to heal or cure the disease [23]. A similar conclusion was made by Clegg-Lamptey et al. [25]. In East Africa, Otieno et al. reported 9.6% of breast cancer patients in Kenya relied on alternative medicine [26]. This percentage was slightly below that of Libya, which was 13.0% [27].
The cultural model of disease is a cognitive model which posits that healthcare seeking is influenced by cultural perceptions about the cause of a particular disease, the different effective treatments available and coping behaviour to eliminate the disease [41,42]. Africans have different beliefs, which are rooted in their cultural forces, individual experiences, and perceptions. Many cultures in Africa associate cancer with a supernatural rather than a biological basis. Symptoms of cancer are attributed to a curse, bewitching, God or god’s punishment due to personal or family atrocity or demons, which can lead to death [43]. Therefore, treating a spiritually caused illness with physical therapies, such as surgery, chemotherapy, or/and radiotherapy will only worsen the condition. Hence, individuals prefer to rely on their faith in sorcerers, witch doctors, herbalists, priests/ priestesses, pastors, and other spiritualists to treat cancer. This partly explains why women may visit an alternative medicine practitioner for cure after observing breast cancer symptoms. These women strongly believe it is a waste of time, money, greater harm, and physical destruction of the body to receive orthodox treatment [124,26,27]. A similar belief was identified among Chinese and South Indian women [44-48].
Social relations and networks: As identified, breast cancer is mostly communicated in a culturally situated context – a disease acquired through cursed or bewitchment. Culturally, no individual is an island in his or her society. According to social theory, behaviour and actions of individuals are shaped by norms, values, social relations, and networks [49]. Social relations and networks refer to the various social relationships, either formal or informal, that surround individuals. Social relations and networks impact health through social support, social influence, social control, companionship, and social comparison [50].
Three of the studies included in the review identified social relations and networks as contributing factor to late presentation or delayed diagnosis of breast cancer among African women [19,22,24]. Two forms of social relations and networks were recognised –social influence and social control. Social influence is the change in an individual’s attitude, cognition or behaviour, which is caused by another individual or group of people [51].
In Nigeria, Ezeome highlighted that 3.2% of breast cancer patients delayed seeking medical help because they were discouraged by friends and relatives [22]. Family, friends, co-workers, and religious members are individuals who exert their influence through caring, financial support and persuasion. They provide direct and immediate interpersonal information on health, which is able to discourage patients from making healthcare decisions.
In most African society, social relationships are webbed or well connected. Individuals are ready to accept certain conditions or issues because of the power or authority the society has on them [52]. This is termed as social control. From the review, 25.3% of breast cancer patients delayed in seeking medical support because their families refused hospital treatment [24]. The review’s finding was similar to Kawar’s study outcome among Jordanian and Palestinian women [53]. Individuals such as family heads, husbands, and religious leaders are highly respected, and trusted in the society. Hence, a woman with breast abnormality has no other option than to accept alternative suggestions from the society, which usually advise on the usage of herbal medicines, prayers, sorcery, and other alternative therapies. Family chaos and neglect are some of the outcomes when an individual goes contrary to the social authorities. This finding confirms the control the society has on the individual.
Lack of trust and confidence in orthodox medicine: Trust forms a central component of healthcare practice. Moorman et al. defined trust as the willingness to entirely depend on an exchange partner in whom an individual has sureness or confidence [54]. According to the commitment-trust theory, which is mostly used in relationship marketing, the cornerstone of any partnership is trust, which is a relational exchange [55]. Similarly, individuals will seek and commit to only partners who are trustworthy, reliable, and credible with high integrity [56]. This is equally true in healthcare. As healthcare becomes more complex and breast cancer incidence rate continues to increase in Africa, trust becomes more important.
Findings from this review indicate that some women delayed in seeking medical help because of lack of trust in the healthcare system. Many general practitioners are losing their credibility because they gave false reassurance that the lump was noncancerous [23,26,27]. Trust encourages patients to preserve a relationship with their service provider and cooperate with them. According to Ezeome, patients were compelled to search for other hospitals or doctors and seek a different opinion concerning their self-identified breast abnormalities [22]. Similarly, breast cancer patients delayed because of strike actions by healthcare professionals. Public trust in healthcare system is highly affected by rapid occurrence of industrial unrest and lack of modern facilities. At the individual level, patients want to maintain commitment, social, and psychological contract with healthcare service providers.
Access to healthcare: Individuals living further away, mostly in rural areas, are more unlikely to access healthcare facilities [57,58]. Women’s inability to access healthcare was recognised as a contributing factor to the late presentation or delayed diagnosis of breast cancer in Africa.
Two main dimensions of access identified were physical access and economic access to healthcare. Stapleton et al. discovered that the majority of Egyptian women delayed because of the location of the cancer centre [19]. Women had to travel long distance to access healthcare facility. Geographical inequalities in healthcare service provision and utilisation is a major concern in Africa. Longer travel time deters women from seeking medical help. This situation is compounded by the poor road networks and transportation system in most African countries. Individuals usually walk or use public transport in accessing healthcare, but public transport availability differs from area to area [59].
The second dimension of access identified was economic access to healthcare. Six of the nine studies included in the review identified the cost of healthcare as a factor for late presentation or delayed diagnosis of symptomatic breast cancer [19,20,22,25]. This finding is in agreement with other studies from Asia [60,61]. In most African countries, since healthcare is expensive, individuals are required to pay out of pocket [62]. Therefore, financial barriers prevent the poor in the society from seeking medical help.
Limitations
The findings of the review must be interpreted with caution as all the included studies demonstrated numerous methodological weaknesses such as the use of unstandardized questionnaires for data collection, small sample size, recall bias, and selection bias. Also, studies published in other languages such as French were excluded. Readers of this review should compare the findings with other comprehensive reviews before making any policy decision. Despite these limitations, the study maintained both rigorous and extensive approaches of reviewing a research paper.
Conclusion
The review has identified that late presentation or delayed diagnosis of breast cancer among African women is influenced by complex matrix of factors. While improved access to affordable healthcare, particularly in rural areas, would undoubtedly improve the uptake of orthodox medicine by women with early breast cancer, this review shows that there are many other factors that need to be addressed in order to address delay in presentation. Widespread, government backed education, on the signs and symptoms of breast cancer, and clear messages of the treatability of the disease, are crucial to the understanding, not only of the individual, but also of their social networks. An increase in trust in healthcare systems is important and this may be addressed by developing partnerships with alternative and traditional healthcare practitioners. Extending the roles of nurses and allied health professionals may also be a way of stretching resources and developing collaborative working across orthodox and traditional boundaries.
Competing Interest
The authors declare that they have no competing interests.
Authors’ contribution
AD: Concept formulation, searching and selection of articles, articles evaluation and analysis, and drafting of manuscript
JL: Searching and selection of articles, articles evaluation and analysis, and drafting of manuscript
SW: Searching and selection of articles, articles evaluation and analysis, and drafting of manuscript
VV: Drafting of manuscript and articles evaluation
DF: Drafting of manuscript and articles evaluation
JY: Drafting of manuscript
SYO: Drafting of manuscript
WA: Drafting of manuscript
KAK: Drafting of manuscript
Acknowledgement
I appreciate Dr. Sue Duke for internally reviewing the paper, Dr. Katherine Hunt and Dr. Richard Wagland for the academic support they provided throughout the study. Finally, I would like to thank Erica Naa Kwardua Quarcoo and Pearl Lawson for proof reading the manuscript.
8456
References
- Ferlay J, Soerjomataram I, Ervik M (2013) Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 1.
- Anderson BO,Jakesz R (2008) Breast cancer issues in developing countries: an overview of the Breast Health Global Initiative. World J Surg 32: 2578-2585.
- World Health Organisation (2011) Cancer survival in Africa, Asia, the Caribbean and Central America.
- Bryan L, Conway M, Keesmaat T, McKenna S, Richardson B (2010) Strengthening sub-Saharan Africa’s health systems: a practical approach.
- Castro-Leal F, Dayton J, Demery L, Mehra K (2000) Public spending on health care in Africa: do the poor benefit? Bull World Health Organ 78: 66-74.
- Vogel JP, Betrán AP, Widmer M, Souza JP, Gülmezoglu AM, et al. (2012) Role of faith-based and nongovernment organizations in the provision of obstetric services in 3 African countries. Am J Obstet Gynecol 207: 495.
- Elujoba AA, Odeleye OM, Ogunyemi CM (2005) Traditional medicine development for medical and dental primary health care delivery system in Africa.
- Hansen RP, Olesen F, Sorensen HT, Sokolowski I, Sondergaard J (2008) Socioeconomic patient characteristics predict delay in cancer diagnosis: a Danish cohort study.
- Ramirez AJ, Westcombe AM, Burgess CC, Sutten S, Littlejohns P,et al. (1999) Factors predicting delayed presentation ofsymptomatic breast cancer: a systematic review. Lancet 353: 1127-1131.
- Burgess CC, Ramirez AJ, Richards MA, Love SB (1998) Who and what influences delayed presentation in breast cancer? Br J Cancer 77: 1343-1348.
- Unger-Saldaña K,Infante-Castañeda C (2009) Delay of medical care for symptomatic breast cancer: a literature review. Salud Publica Mex 5 Suppl 2: s270-285.
- Facione NC(1993) Delay versus help seeking for breast cancer symptoms: a critical review of the literature on patient and provider delay. SocSci Med 36: 1521-1534.
- Weed DL (1997) Methodologic guidelines for review papers. Journal of the National Cancer Institute 89: 6-7.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A (2005) Synthesising qualitative and quantitative evidence: a review of possible methods. Journal of Health Services Research and Policy 10: 45-53.
- Coughlan M, Cronin P, Ryan F (2007) Step-by-step guide to critiquing research. Part 1: quantitative research. Br J Nurs 16: 658-663.
- Stapleton JM, MullanPB, Dey S, (2011) Patient-mediated factors predicting early and late stage presentation of breast cancer in Egypt. Psycho-Oncology20: 532-537.
- Ismail GE, Abd El Hamid AA, Abd El Naby AG (2013) Assessment of factors that hinder early detection of breast cancer among females at Cairo University Hospital. World Applied Sciences Journal. 23: 99-108.
- Abdel-Fattah MM, Anwar MA, Mari E, El-Shazly MK (1999) Patient-and system-related diagnostic delay in breast cancer: evidence from Alexandria, Egypt. European Journal of Public Health 9: 15-19.
- Ezeome ER (2010) Delays in presentation and treatment of breast cancer in Enugu, Nigeria. Niger J ClinPract 13: 311-316.
- Ibrahim NA, Oludara MA (2012) Socio-demographic factors and reasons associated with delay in breast cancer presentation: a study in Nigerian women. Breast 21: 416-418.
- Ukwenya AY,Yusufu LM, Nmadu PT, GarbaES, Ahmed A (2008) Delayed treatment of symptomatic breast cancer: the experience from Kaduna, Nigeria. S Afr J Surg 46: 106-110.
- Clegg-Lamptey J,Dakubo J, AttobraYN (2009) Why do breast cancer patients report late or abscond during treatment in ghana? A pilot study. Ghana Med J 43: 127-131.
- 26. OtienoES, Micheni JN, Kimende SK, Mutai KK. Delayed presentation of breast cancer patients. East African Medical Journal. 2010; 87(4): 147-150.
- Ermiah E,Abdalla F, Buhmeida A, Larbesh E, Pyrhönen S, et al. (2012) Diagnosis delay in Libyan female breast cancer. BMC Res Notes 5: 452.
- Abdel-Wahab M, Bourque JM, Pynda Y, Iżewska J, Van der Merwe D, et al. (2013) Status of radiotherapy resources in Africa: an International Atomic Energy Agency analysis. Lancet Oncol 14: e168-175.
- Nosarti C, Crayford T, Roberts JV, Elias E, McKenzie K, et al. (2000) Delay in presentation of symptomatic referrals to a breast clinic: patient and system factors. British Journal of Cancer 83: 742-748.
- Ohman A, MinekaS (2001) Fears, phobias and preparedness: toward an evolved module of fear and fear learning. Psychological Review 108: 483-522.
- Ruiter RAC, Abraham C, Kok G (2001) Scary warnings and rational precautions: a review of the psychology of fear appeals. Psychology and Health 16: 613-630.
- Tod AM, Joanne R (2010) Overcoming delay in the diagnosis of lung cancer: a qualitative study. Nurs Stand 24: 35-43.
- Smith LK, Pope C, Botha JL (2005) Patients' help-seeking experiences and delay in cancer presentation: a qualitative synthesis. Lancet 366: 825-831.
- Schmid M, Wolf RC, FreudenmannRW, Schönfeldt-Lecuona C (2009) Tomophobia, the phobic fear caused by an invasive medical procedure - an emerging anxiety disorder: a case report. J Med Case Rep 3: 131.
- Cassileth BR, Deng G (2004) Complementary and alternative therapies for cancer. Oncologist 9: 80-89.
- Dorval M,Maunsell E, Taylor-Brown J, Kilpatrick M (1999) Marital stability after breast cancer. J Natl Cancer Inst 91: 54-59.
- Yarney J, Donkor A, OpokuSY (2013) Characteristics of users and implications for the use of complementary and alternative medicine in Ghanaian cancer patients undergoing radiotherapy and chemotherapy: a cross-sectional study. BMC Complementary and Alternative Medicine13: 16-25.
- Truant TL, Porcino AJ, Ross BC, Wong ME, Hilario CT2 (2013) Complementary and alternative medicine (CAM) use in advanced cancer: a systematic review. J Support Oncol 11: 105-113.
- Donkor A, OpokuSY (2013) Complementary medicine use among cancer patients undergoing palliative radiation therapy. Journal of Palliative Care and MedicineS3: 5-9.
- Molassiotis A,Fernadez-Ortega P, Pud D, Ozden G, Scott JA, et al. (2005) Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol 16: 655-663.
- Stephens NM, Fryberg SA, Markus HR (2012) Social class disparities in health and education: reducing inequality by applying a sociocultural self-model of behaviour. Psychological Review 119: 723-744.
- Angel R,Thoits P (1987) The impact of culture on the cognitive structure of illness. Cult Med Psychiatry 11: 465-494.
- Opoku SY,Benwell M, Yarney J (2012) Knowledge, attitudes, beliefs, behaviour and breast cancer screening practices in Ghana, West Africa. Pan Afr Med J 11: 28.
- Kishore J, Ahmad I, Kaur R, MohantaPK (207) Beliefs and perceptions about cancer among patients attending radiotherapy OPD in Delhi, India. Asian Pacific Journal of Cancer Prevention9: 155-158.
- Wong-Kim E, Sun A, DeMattos MC (2003) Assessing cancer beliefs in a Chinese immigrant community. Cancer Control 10: 22-28.
- Johnson JL,Bottorff JL, Balneaves LG, Grewal S, Bhagat R, et al. (1999) South Asian womens' views on the causes of breast cancer: images and explanations. Patient EducCouns 37: 243-254.
- Teel CS, Meek P, McNamara AM, Watson L (1997) Perspectives unifying symptom interpretation. Image J NursSch 29: 175-181.
- Burgess C, Hunter MS, Ramirez A (2001) A qualitative study of delay among women reporting symptoms of breast cancer. British Journal of General Practice51: 967-971.
- Heaney CA, Israel BA (2008) Social networks and social support. In: Glanz K, RimerBK, Viswanath K, eds. Health behaviour and health education: theory, research and practice,(4th edn) John Wiley and Sons,San Francisco.
- Glanz K, Rimer BK, Viswanath K (2008) Health behaviour and health education: theory, research and practice (4th edn), John Wiley and Sons, San Francisco.
- Sharma M, Romas JA (2012) Theoretical foundations of health education and health promotion.
- Kawar LN (2013) Barriers to breast cancer screening participation among Jordanian and Palestinian America women. European Journal of Oncology Nursing17: 88-94.
- Moorman C, Deshpande R, Zaltman G (1993) Factors affecting trust in market research relationships. Journal of Marketing 57: 81-101.
- Abosag I, Tynan C, Lewis C (2006)The commitment-trust theory: The British and Saudi Arabian cross-national perspectives.
- Morgan RM, Hunt SD (1994)The commitment-trust theory of relationship marketing. Journal of Marketing 58: 20-38.
- Armstrong Schellenberg JR,Mrisho M, Manzi F, Shirima K, Mbuya C, et al. (2008) Health and survival of young children in southern Tanzania. BMC Public Health 8: 194.
- Magnani RJ, Rice JC, Mock NB, Abdoh AA, Mercer DM, et al. (1996) The impact of primary health care services on under-five mortality in rural Niger. Int J Epidemiol 25: 568-577.
- Arcury TA,GeslerWM, PreisserJS, Sherman J, Spencer J, et al. (2005) The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res 40: 135-155.
- Yau TK, Choi CW, Ng E, Yeung R, Soong IS, et al. (2010) Delayed presentation of symptomatic breast cancers in Hong Kong: experience in a public cancer centre. Hong Kong Med J 16: 373-377.
- Lam WW, Fielding R, Chan M, Or A (2009) Factors influencing delayed presentation with symptomatic breast cancer in Hong Kong Chinese women. Hong Kong Medical Journal 15: 4-7.
- Tanser F, Gijsbertsen B, Herbst K (2006) Modelling and understanding primary health care accessibility and utilization in rural South Africa: an exploration using a geographical information system. Social Science and Medicine 63: 691-705.