N Tsekova Traykovich*, D Nikolova, A Argirov
Department of Dermatovenereology, Medical University, Sofia, Bulgaria
- Corresponding Author:
- N Tsekova Traykovich
Department of Dermatovenereology
Medical University, Sofia, Bulgaria
Tel: 359 886307415
E-mail: natasa_cekova@yahoo.com
Received Date: May 26, 2021; Accepted Date: July 02, 2021; Published Date: July 09, 2021
Citation: Traykovich NT, Nikolova D, Argirov A (2021) Gaint Condylomata Acuminate of Buschke-Lowenstein in Woman with HPV Infection: Clinical Presentation and Treatment. Ann Clin Lab Res. Vol.9 No.7:360. doi: 10.36648/2386-5180.9.7.360
Copyright: © 2021 Traykovich NT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Buschke-Lowenstein tumor; HPV; SCC
Introduction
Buschke-Lowenstein Tumor (BLT) is a very rare sexuallytransmitted disease associated with human papillomavirus. It is a neoplasm of the anogenital region which has appearance on histopathology as relatively low-grade malignancy, but is locally destructive and with aggressive behaviour [1]. We have discussed an overview of etiopathogenesis, clinical presentation, diagnosis and management of this uncommonly disease [2].
Case Presentation
A 59-year-old female multiparous, immune competent patient with two normal deliveries and in menopause for 15 years presented to our clinic with a large, exophytic, cauliflower-like tumor involving the vulva, perineum and perianal regions.
The first lesions had been appeared on labia majora as pin-size papules before 30 years ago during pregnancy period [3]. They gradually increased in size and coalesced to form large tufts and covered perineum and perianal area.
It was not painful, but caused some discomfort mainly during sitting, urination and defecation. The lesions were treated with different locally destructive modalities without significant results. Her husband was examined and found to be free of any lesions in genital area [4].
The patient denied any history of extramarital sexual contact or assault. Physical examination reveled a 30 cm exophytic cauliflower like tumor affecting vulva, perineum and perianal regions and low vagina [5].
In some points erosions and yellowish secretion with odor are observed. Upper vagina and cervix appeared normal. No locoregional lymph nodes were present upon palpation. A Papanicolaou cervical smear was performed and smear from portio vaginals cervix uteri and cervix coli was classified as IIA group [6]
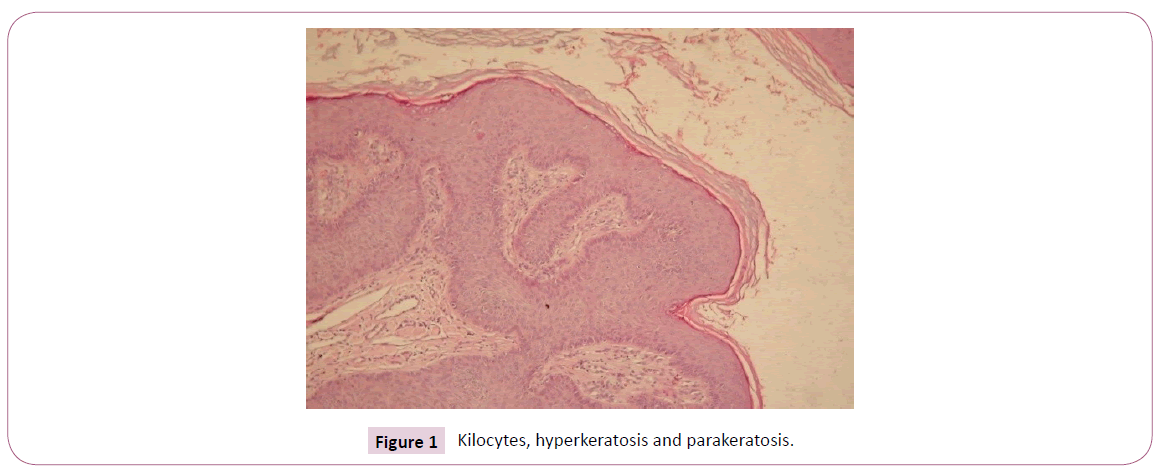
Her HIV, HbsAgan, VDRL status were nonreactive. Contrast enhanced computer tomography of chest, abdomen and pelvis was done that did not reveal any regional lymph node involvement or evidence of distant metastasis. Colonoscopy data for tumor mass which reached linea dentate mass without invasion in anal sphincter (Figure 1).
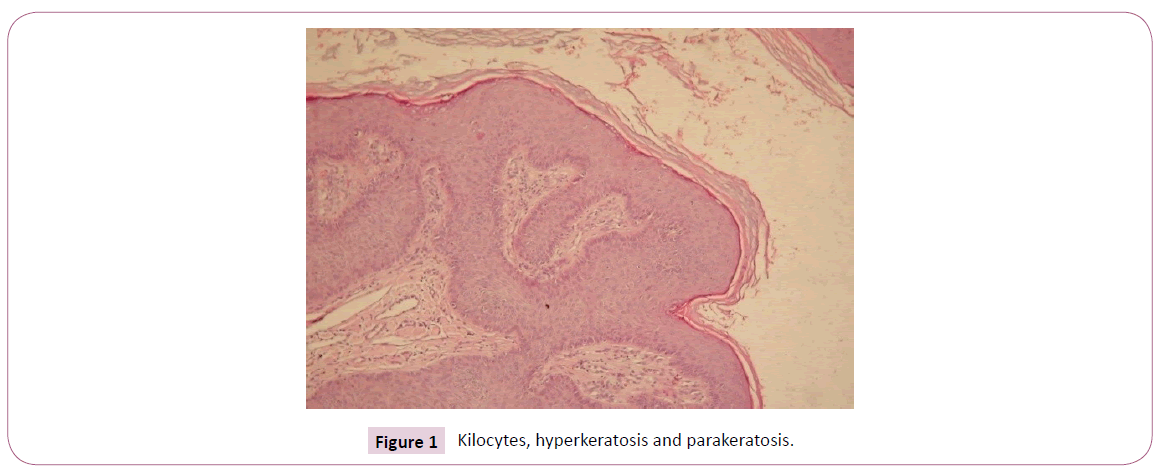
Figure 1: Kilocytes, hyperkeratosis and parakeratosis.
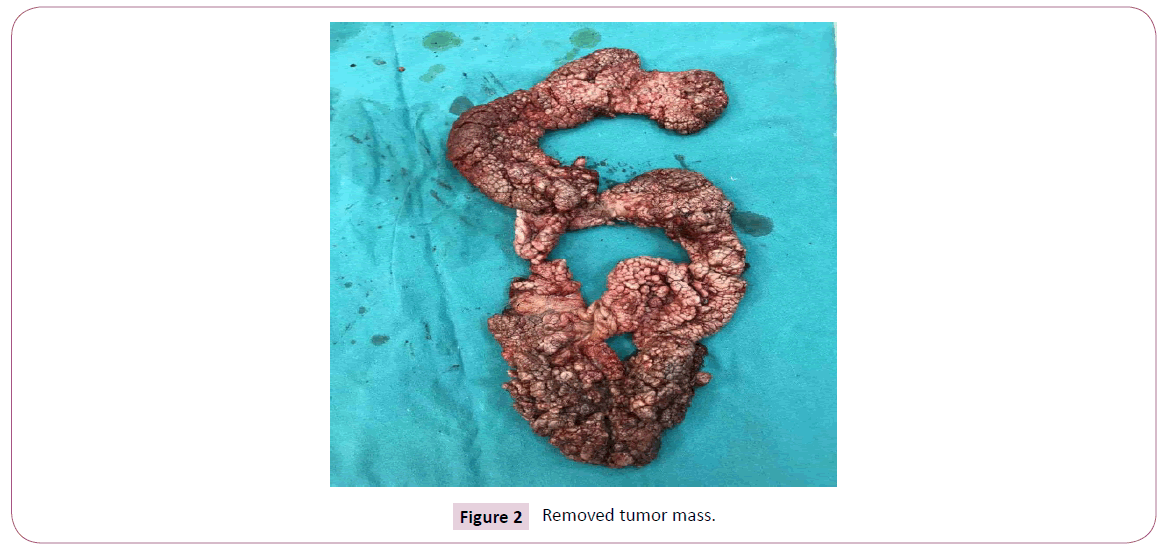
A biopsy, under local anesthesia, was performed. On histology we observed koilocytic changes, hyperkeratosis and parakeratosis. The epithelium extends into the dermis with blunt-shaped masses, forming sinuses and keratin-filled cysts. The distinction from conventional squamous cell carcinoma witch rests on 2 criteria: cytologic atypia and clearly infiltrative pattern of growth, are not seen in our case [7]. A PCR of the specimen revealed the presence of HPV- type 6,11. The patient was send to Gynecology department and radical vulvectomy was performed. Follow-up after 1 year did not reveal any new lesions (Figure 2).
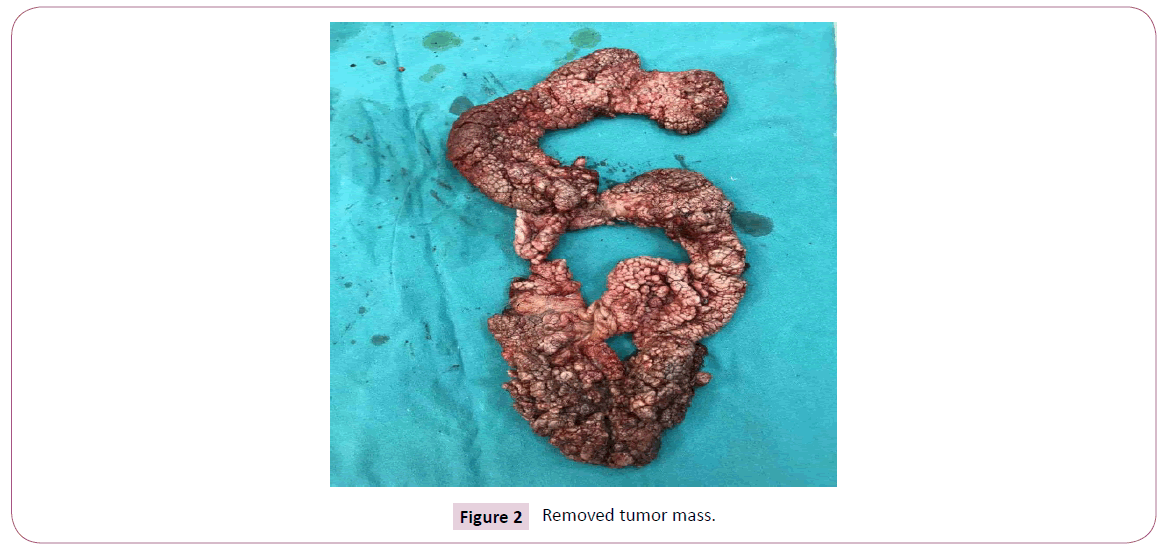
Figure 2: Removed tumor mass.
Discussion and Conclusion
BLT first described by Buschke and Lowenstein in 1925. They observed a penile lesion that clinically resembled both common condyloma acuminata and squamous cell carcinoma, but differing from both of them regarding the biological behavior and the histopathological appearance. Some authors support the hypothesis that BLT is an intermediary lesion between condyloma acuminata and SCC. However, others equate it to verrucous carcinoma of the anogenital region. It is a very rare sexually transmitted disease associated with HPV type 6 and 11, suggesting a pathogenic role. Rare cases of oncogenic HPV types- HPV 16, 18, 54 were also reported. There is no racial predilection and male-to-female ratio is 3.5:1. BLT is located in the genital, anorectal and perianal regions. It is well differentiated, benign lesion and its management is often challenging due to the size, rapidly growing, degree of local invasion, and recurrence rate. Perirectal GCBL include perianal mass (47%), fistula or abscess (32%), and bleeding (18%). BLT is associated with a high rate of recurrence (up to 70%) and a risk of malignant transformation to SCC (30-56%), especially in immune-compromised status and patients with oncogenic types of HPV.
The diagnosis is based mainly of clinical presentation, histological picture and PCR- HPV DNA. A proper biopsy must be wide and deep enough to accurately determine the extension of infiltration of the tumor and the possible presence of a squamous cell carcinoma. differentiated from ordinary condylomas by the characteristic pushing rather than “infiltrating” effect that tends to compress and displace the underlying tissue. Radical surgical excision is the gold standard in treatment. Other various treatment topical modalities include podophyllin, 5-FU, Interferon, ?leomycin (intralesional), ?idofovir gel 1.5%, Imiquimod in association with ??2 laser. Chemoradiation has been recommended when malignant transformation my occur. Radiation therapy alone has been discouraged because of protentional risk of transformation into anaplastic carcinoma. And last but not the least HPV vaccine could lead to a protentional prevention and reduction in the incidence of this disease. Because of frequent recurrence and malignant transformation multidisciplinary patient control collaboration is necessary and regular follow-up is mandatory.
38712
References
- Spinu D, Radulescu A, Bratu O, Checherita IA, Ranetti AE, et al. (2014) Giant condyloma acuminatum-Buschke- Lowenstein disease: A literature review. Chirurgia 109: 445-50.
- Mohs FE, Sahl WJ (1979) Chemosurgery for verrucous carcinoma. J Dermatol Surg Oncol 5: 302-6.
- Weils M, Robertson S, Lewis F, Dixon MF (1988) Squamous carcinoma arising in a giant condyloma associated with human papillomavirus type 6 and 11. Histopathology 12: 319–23.
- Dolanc R, Kocher T, Langer I, Marti WR, Pierer G, et al. (2002) Malignant transformation of perianal Buschke-Lowenstein tumor. Extensive abdominoperineal rectum excision and reconstruction with transpelvic myocutaneous rectus abdominis muscle flap. Chirurg 73: 370-4.
- Safi F, Bekdache O, Al-Salam S, Alashari M, Mazen T, et al. (2013) Management of peri-anal giant condyloma acuminatuma case report and literature review. Asian J Surg 36: 43–52.
- Battaglia L, Vannelli A, Belli F, Rampa M, Milione M, et al. (2011) Giant condyloma acuminatum of the anorectum: Successful radical surgery with anal reconstruction. Tumori 97: 805-7.
- Correia E, Santos A (2015) Buschke-Lowenstein tumour: Successful treatment with minimally invasive techniques. Case Rep Dermatol Med 2015: 651703.