Dr. Ajay Kumar Pandey*
Department of Pediatric Cardiac Surgery, Sir Gangaram Hospital, New Delhi, India
- *Corresponding Author:
- Dr. Ajay Kumar Pandey
Department of Pediatric Cardiac Surgery
Sir Gangaram Hospital
GC 510, Aditya Mega city, Vaibhav Khand Indirapuram
Ghaziabad, New Delhi, India
Tel: +91 9559500485
E-mail: drajaykumarpandey@gmail.com
Received Date: May 14, 2021; Accepted Date: May 25, 2021; Published Date: May 31, 2021
Citation: Pandey AK (2021) Gastric Outlet Obstruction Due to Primary Duodenal Tuberculosis - A Case Report on Rare Presentation of an Uncommon Condition. Arch Med Vol. 13 No. 5:24.
Keywords
Gastro duodenal tuberculosis; Gastrojejunostomy; Duodenal tuberculosis
Introduction
Tuberculosis is a major health problem worldwide and is endemic in India, especially in people of low socio-economic group. Pulmonary Tuberculosis is the most common manifestation and gastrointestinal tract is 6th most frequent site after lymphatic, genitourinary, bone, miliary and meningeal tuberculosis; with ileo-caecal region as the most common site involved in gastrointestinal tuberculosis [1]. Gastroduodenal Tuberculosis is a rare clinical entity and usually a result of secondary spread from pulmonary tuberculosis [2]. Primary duodenal tuberculosis presenting as gastric outlet obstruction is extremely rare. There is no management guideline present for primary duodenal tuberculosis presenting with gastric outlet obstruction in literature. Hence here we present the case report of two such rare cases and the treatment given.
Case Series
Case 1
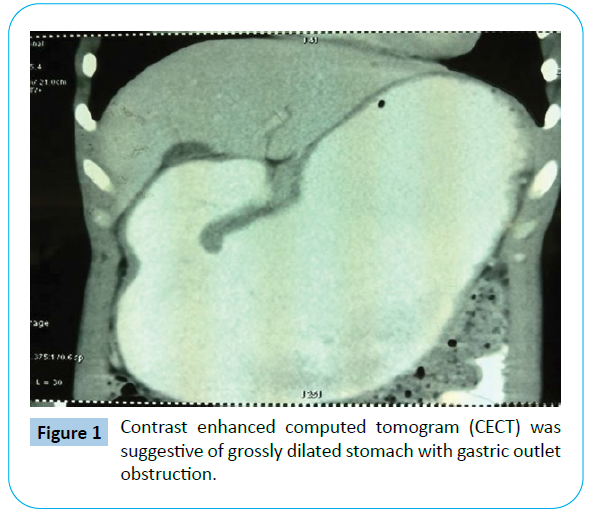
A 17-year-old male was admitted with history of vomiting associated with fullness of abdomen immediately after food since one year, and anorexia with weight loss in last 6 months. Biochemical parameter was normal except for raised erythrocyte sedimentation rate (ESR) (53 mm/hr). Contrast Enhanced Computed Tomogram (CECT) was suggestive of grossly dilated stomach with outlet obstruction (Figure 1). Upper gastrointestinal endoscopy revealed erythematous antrum with no visible duodenal opening and old food particles.
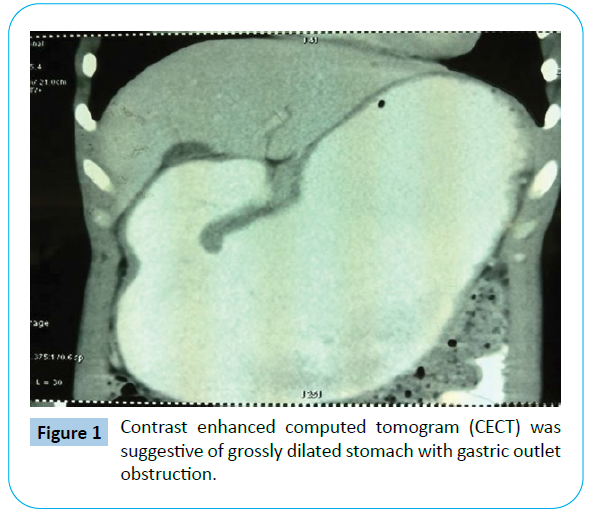
Figure 1: Contrast enhanced computed tomogram (CECT) was suggestive of grossly dilated stomach with gastric outlet obstruction.
Patient underwent exploratory laparotomy. Intraoperatively, grossly dilated stomach was seen with duodenal thickening in 1st and 2nd part with few enlarged and calcified lymph nodes. Gastrojejunostomy was done and biopsy taken from duodenum and lymph nodes. Post-operative recovery was uneventful. On histopathological examination, a chronic granulomatous inflammation with Langhans-type giant cell was seen. The patient was diagnosed as primary duodenal tuberculosis, and discharged on post-operative day 8 on WHO antitubercular 4 drug regime. Patient has been under regular follow up since 1 year, has gained weight and is asymptomatic at present.
Case 2
A 23-year-old female patient reported to our outpatient department with complain of pain in epigastrium and vomiting since one month, low-grade fever since three month, weight loss and anorexia since six months. Body mass index was low 16.44. Patient had raised ESR (89 mm/hr). CECT whole abdomen was suggestive of enlarged lymph nodes at porta and in peripancreatic region. Upper gastrointestinal endoscopy revealed closed pylorus with multiple ulcers (Figure 2). Exploratory laparotomy was done. Intraoperatively, circumferential thickening at pylorus and D1 segment of duodenum was seen along with matted, calcified lymph nodes in lesser sac. Gastrojejunostomy was done, and lymph node biopsy taken. Post-operative recovery was uneventful. Histopathology was suggestive of caseating tuberculous lymphadenitis. Patient was started on WHO antitubercular 4 drug regimen, and regular follow-up done. She has gained more than 10 kg weight in last 4 months, and is asymptomatic.

Figure 2: Upper gastrointestinal endoscopy image showing closed pylorus with multiple ulcers.
Discussion
Upper gastrointestinal tuberculosis is rarely seen even in endemic areas, with duodenal involvement an exceedingly rare entity reported only in a few cases [2,3]. In previously reported cases of, medical management has been sufficient treatment modality. However in cases presenting with obstruction, emergent surgery may be required.
The diagnosis of gastroduodenal tuberculosis is difficult preoperatively as there are no pathognomic clinical features. Vomiting (86.08%) and epigastric pain (56.5%) are most common presenting symptoms. Other symptoms noted are weight loss, upper GI bleeding and fever [2]. Patient in our case had presented with episodes of upper abdominal distension followed by vomiting, weight loss and anorexia.
Radiological diagnosis of gastroduodenal tuberculosis is also difficult. On barium studies duodenal tuberculosis presents nonspecifically as various combination of mucosal ulceration, luminal narrowing, extrinsic compression and proximal dilatation [4]. Endoscopy is not conclusive most of the time. Endoscopic biopsy shows non-specific inflammation [5]. Duodenal tuberculosis being a sub mucosal disease, endoscopic brush biopsy may fail [6]. For patients in our case, case 1 had presented with obstruction, barium study was deferred and endoscopic biopsy report would had taken time, case 2 endoscopic brush biopsy was inconclusive and s/o chronic gastritis.
Gastric outlet obstruction occurs commonly due to peptic ulcer or malignancy. Our patients were young (17 yrs & 23 yrs), so malignancy was taken as remote possibility. History and Upper gastrointestinal scopy ruled out peptic ulcer disease. As patients had presented with features of obstruction, emergent surgery was offered as first treatment and subsequently antitubercular treatment was given based on histopathology. Management of gastroduodenal tuberculosis if diagnosed before surgery is medical, with standard WHO quadruple drug regimen [7].
Conclusion
Duodenal tuberculosis is a rare clinical entity. Presentation of duodenal tuberculosis as gastric outlet obstruction is even rare. High index of suspicion should be kept in patient coming from endemic areas. Efforts are taken to diagnose the condition before need for surgery as medical management has shown promising results. Surgical procedure be offered in cases presenting with acute obstruction and be followed with anti-Koch’s treatment regimen.
37577
References
- Gorbach S (1989) Tuberculosis of the gastrointestinal tract. In: Sleisenger M (ed).Gastrointestinal diseases. (4th edn), Philadelphia: WB Saunders, USA. 2: 363-372.
- Rao YG, Pande GK, Sahni P, Chattopadhyay TK (2004) Gastroduodenal tuberculosis management guidelines, based on a large experience and a review of the literature. Can J Surg 47: 364-368.
- Padussis J, Loffredo B, McAneny D (2005) Minimally invasive management of obstructive gastroduodenal tuberculosis. Am Surg 71: 698-700.
- Chavhan GE, Ramakantan R (2003) Duodenal tuberculosis; radiological feature on barium studies and their clinical correlation in 28 cases. J Postgraduate Med 49: 214-217.
- Sharma BL, Prasad H, Bhasin DK, Singh K (2000) Gastroduodenal Tuberculosis presenting with massive hematemesis in a pregnant woman. J Clin Gastroenterol; 30: 336.
- Kuganeswaran E, Smith OJ, Quiason SG, Clarkston WK, Pandya PK, et al. (1998) Both massive upper and lower gastrointestinal haemorrhage secondary to tuberculosis. Am J Gastroenterol 94: 271-272.
- Agarwal S, Shetty SV, Bakshi G (1999) Primary hypertrophic tuberculosis of pyloroduodenal area: A report of 2 cases. J post grad med 45:10-12.