Case Report - (2025) Volume 13, Issue 1
Giant Epidermoid Cyst of the Spleen: A Case Report
I. Boucebaine1*,
S. Irtan1,
L. Karima2,
L. Derradj3,
Y. Benaissa3,
L. Ammari3 and
Taibi3
1Department of Pediatrics, Creteil Intercommunal Hospital, Creteil, France
2Department of Pediatrics, Oran University Hospital, Algeria, France
3Department of Pediatrics, Bordj Bou Arreridj EPH, Algeria, France
*Correspondence:
I. Boucebaine, Department of Pediatrics, Creteil Intercommunal Hospital, Creteil,
France,
Email:
Received: 26-Sep-2024, Manuscript No. IPJUS-25-15455;
Editor assigned: 30-Sep-2024, Pre QC No. IPJUS-25-15455 (PQ);
Reviewed: 14-Oct-2024, QC No. IPJUS-25-15455;
Revised: 01-Mar-2025, Manuscript No. IPJUS-25-15455 (R);
Published:
28-Mar-2025
Abstract
Splenic cysts are a rare entity. They are divided into two groups: Parasitic and non-parasitic splenic cysts. Epidermoid cysts of the spleen belong to the primary non-parasitic group. They usually occur in children. They are most often asymptomatic, but they can present with abdominal discomfort.
Case presentation: We report the case of a 12-year-old child with a large splenic cyst. Additional examinations suggested an epidermoid cyst. A total splenectomy was performed via laparotomy. The pathological examination confirmed the diagnosis.
Conclusion: Recently, conservative surgical treatment in children has become the gold standard; in certain cases, a total splenectomy is mandatory if the cyst is large or if its anatomical position do not allow conservative treatment.
Keywords
Splenic cysts; Epidermoid cyst; Splenectomy
Introduction
Epidermoid cysts of the spleen are very rare. They are
primarily Primary Non-Parasitic Splenic Cysts (PNSCs),
representing approximately 2.5% of splenic cysts. They most
commonly occur in children and young women and have a good
prognosis overall. Splenic cysts are asymptomatic in
approximately 30% of cases and are usually discovered
incidentally. In exceptional cases, they present with certain
complications, such as infection, rupture and bleeding. Currently,
the diagnosis of epidermoid cysts has become easier given the
advances in diagnostic techniques; however, only a few cases
have been published in the literature to date. Traditionally,
surgical treatment is recommended for symptomatic cysts larger
than 5 cm. We report in this work a case of a giant epidermoid
cyst of the spleen [1].
Case Presentation
A 12-year-old child, with no past medical history, presented to
the pediatric surgery emergency department with a left
hypochondrium mass (Figure 1). Upon questioning the patient, it
was noted that he had few symptoms apart from an early gastric
fullness sensation during meals associated with left
hypochondrium pain and a palpable mass extending from the
left hypochondrium to the pelvis. The abdominal ultrasound,
performed as a first-line examination, indeed revealed a large
mass in the left hypochondrium. We supplemented this with an
abdominal CT scan [2].
Diagnostic
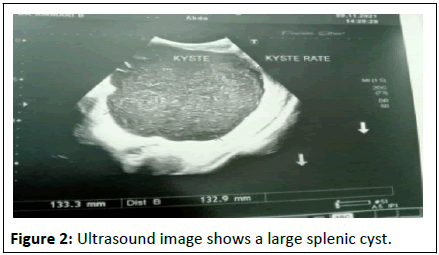
Abdominal ultrasound reveals a large, well-circumscribed
cystic formation measuring 133 × 134 mm with a finely
thickened fluid content with fine echogenic spots located in the
left hypochondrium. The structure appears to be dependent of
the spleen located in its lower pole [3].

Figure 1: A curvature of the left hypochondrium.
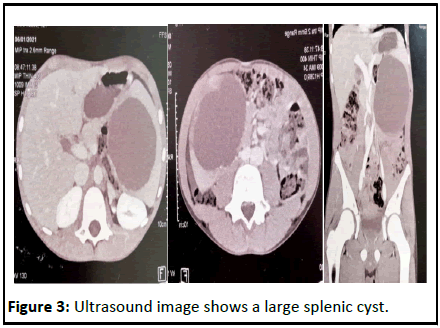
The CT scan confirmed a large well-defined cystic formation
(95 × 107 × 117 mm) with regular contours and heterogeneous
density.
• Medially, it comes into contact with the splenic vein, which is
laminated.
• Inferiorly, it contacts the loops and a branch of the mesenteric
artery over a 30 mm length.
• It contacts the aorta over a 40 mm length and the renal
vascular pedicle.
• It pushes back the left kidney and pancreas.
• All criteria suggest a hydatid cyst.
We completed the assessment with hydatid serology and
tumor markers (CA19.9, AFP), which returned negative. The
absence of any evidence of splenic trauma and hematic
sediment rule out a post-traumatic cyst. The absence of a
daughter cyst and the absence of associated liver lesions in this
child argues against a hydatid cyst. Furthermore, the thin,
regular walls rule out cystic lymphangioma, whose edges are
classically scalloped. Finally, the content of fine echogenic spots
that may correspond to cholesterol crystals suggests the
diagnosis of an epidermoid cyst of the spleen [4].
Treatment
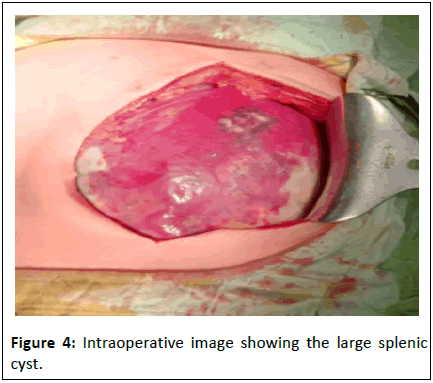
A total splenectomy was performed en-bloc via a midline
laparotomy given the large volume of the cyst and the tight
anatomical relations after vaccination prophylaxis.
The pathological examination confirmed the diagnosis of an
epidermoid cyst (Figures 2-4). The outcome was favorable [5].
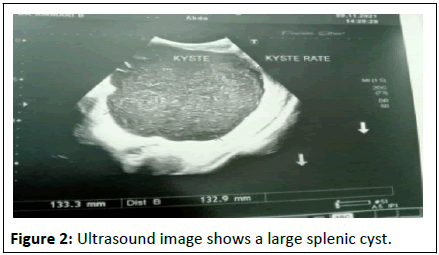
Figure 2: Ultrasound image shows a large splenic cyst.
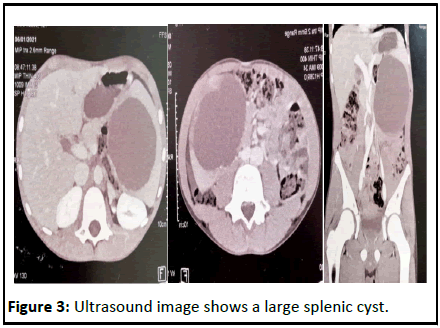
Figure 3: Ultrasound image shows a large splenic cyst.
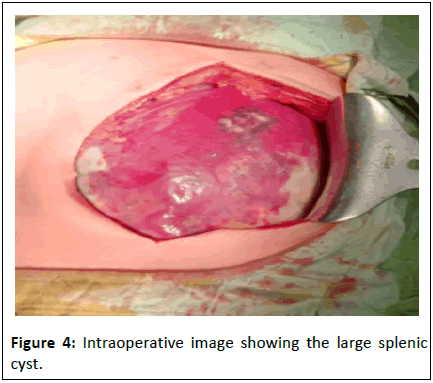
Figure 4: image showing the large splenic
cyst.
Results and Discussion
Splenic cysts, although rare (approximately 1000 cases
reported), have been the subject of multiple classifications which
distinguish (Table 1) [6].
| Clinical classification of splenic cysts (martin) |
| Primary-True |
| Parasitic |
| Non-parasitic |
| Congenital |
| Neoplastic |
| Secondary-False |
Table 1: Classification table of splenic cysts.
Epidermoid cysts of the spleen are rare benign tumors. They
represent 2.5% of all splenic cysts and 25% of non-parasitic
splenic cysts. Their cause is undetermined; their occurrence
possibly results from inclusions of mesothelial remnants in the
spleen. This is a congenital pathology that is found mainly in
children and young adults, with a female predominance. They
are generally small and asymptomatic, discovered incidentally.
They can gradually increase in size. Cysts larger than 5 cm may
present with splenomegaly, pain in the left hypochondrium,
shoulder or chest pain, dyspnea, persistent cough, nausea,
vomiting, constipation, dyspepsia, dysphagia or sometimes a
palpable mass with signs of compression of nearby organs.
This is the case of our patient who presented with a palpable
mass (cyst larger than 5 cm) that was painful and showed signs
of compression of neighboring organs. In very rare cases, when
the diameter exceeds 8 cm, other complications may occur, such
as intracystic hemorrhage or rupture, which induce peritoneal
signs such as hemoperitoneum or peritonitis. Superinfections
remain exceptional. In the literature, the symptoms and
complications of cysts are proportionally linked to their
diameter. The growth of the NPSC is slow and occurs over
several years, culminating at around the ages of 11 and 12 [7].
On abdominal ultrasound, the most characteristic signs were:
• The existence of a fluid-filled mass with posterior
enhancement and finely mobile echogenic content. This
content, highly suggestive of the diagnosis of epidermoid cyst,
is attributed to cholesterol crystals, keratin lamellae,
hemorrhage or intracystic superinfection.
• The existence of a single, well-defined mass with peripheral
trabeculae (“festoon sign”).
The CT appearance is less specific than the ultrasound
appearance. The epidermoid cyst is a benign cystic lesion whose
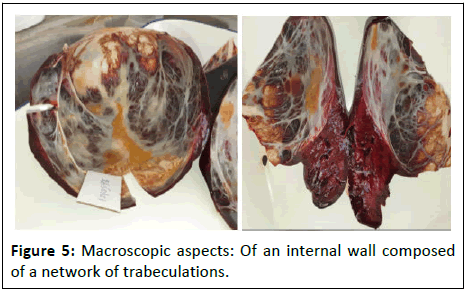
ultrasound appearance is practically pathognomonic. A
pathological study of the surgical specimen confirms the
diagnosis. On macroscopic examination: The internal wall of the
cyst is composed of a network of thick, fibrous trabeculations
and areas covered with squamous epithelium. The fluid content
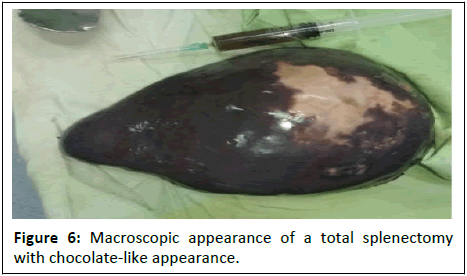
is chocolate-colored (Figures 5 and 6). The definitive diagnosis
can only be established based on the cytopathology studies with
the presence of a cuboidal, columnar or squamous epithelial
lining [8].
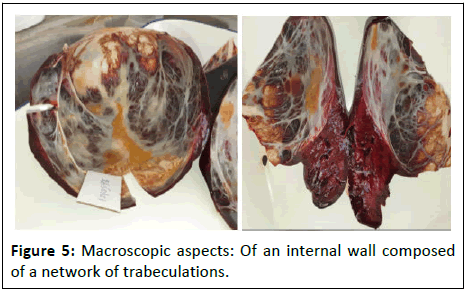
Figure 5: Macroscopic aspects: Of an internal wall composed
of a network of trabeculations.
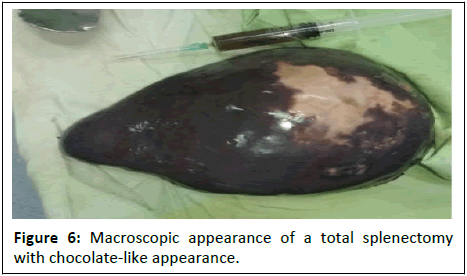
Figure 6: Macroscopic appearance of a total splenectomy
with chocolate-like appearance.
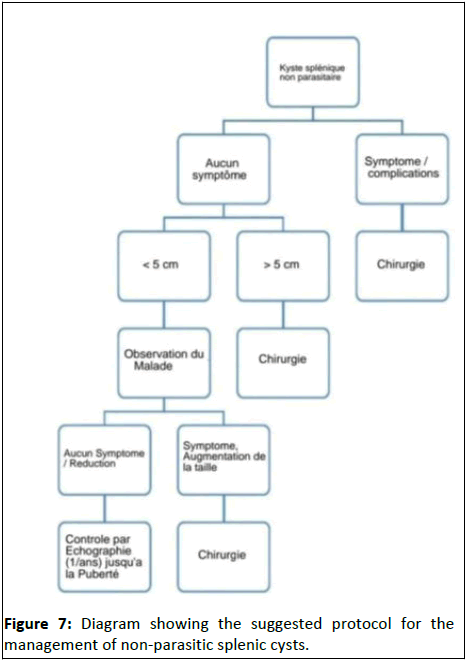
The spleen has an immunological function, so its preservation
should be a therapeutic concern, especially in children. The
management of Non-Parasitic Splenic Cysts (NPSCs) remains
controversial. Several conservative treatment strategies can be
proposed for cysts smaller than 5 cm, such as surveillance,
aspiration with or without sclerotherapy or cystectomy.
Conservative treatment for cysts larger than 5 cm increases
the risk of recurrence. Partial or total splenectomy is performed
conventionally or laparoscopically. Different surgical options
have been suggested depending on the patient's age, symptoms,
size, nature of the cyst and its anatomical relationships with
neighboring organs. Surgical treatment involves partial
splenectomy preferably, but this requires the metameric
arrangement of the vascularization and polar position of the
epidermoid cyst (Figure 7) [9].
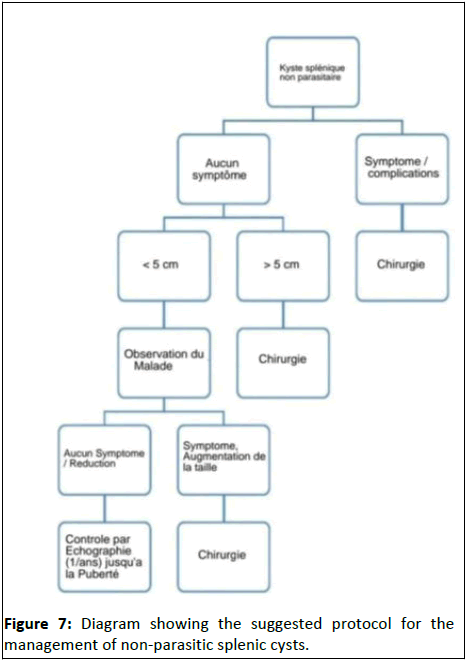
Figure 7: Diagram showing the suggested protocol for the
management of non-parasitic splenic cysts.
Partial splenectomy is technically more difficult to perform
and carries a risk of bleeding during division of the splenic
parenchyma. Our case presented a 10 cm cyst with intimate
connections to the vessels and adhesions to neighboring organs.
In this situation, we recommend a total splenectomy.
Conclusion
Splenic epidermoid cysts are rare benign tumors. They are
often discovered incidentally, despite their sometimes-large size,
as in our case. Ultrasound and CT scans can guide the diagnosis,
which is confirmed by pathological examination. The surgical
treatment of choice is conservative which might sometimes be
impossible. If the cyst is large or if its anatomical relationships
with the surrounding tissues prevent partial splenectomy, a total
splenectomy is recommended.
References
- Cianci P, Tartaglia N, Altamura A, Fersini A, Vovola F, et al. (2016) A recurrent epidermoid cyst of the spleen: Report of a case and literature review. World J Surg Oncol 14: 1-4.
[Crossref] [Google Scholar] [PubMed]
- Mahi M (2007) DIG-WP-19 Imaging of splenic masses. J Radiol 88: 1534.
- Robbins FG, Yellin AE, Lingua RW, Craig JR, Turrill FL, et al. (1978) Splenic epidermoid cysts. Ann Surg 187: 231.
[Crossref] [Google Scholar] [PubMed]
- Gervaise A (2007) Giant epidermoid cyst of the spleen. Feuillets de radiologie 47: 37-41.
- Dossouvi T (2018) Epidermoid splenic cyst: A report of two cases. Rech Sci Univ Lome 20: 461-465.
- Pastore V, Bartoli F (2014) A report of a giant epidermoid splenic cyst. Afr J Paediatri Surg 11: 67-70.
[Crossref] [Google Scholar] [PubMed]
- Delforge X, Chaussy Y, Borrego P, Abbo O, Sauvat F, et al. (2017) Management of nonparasitic splenic cysts in children: A French multicenter review of 100 cases. J Pediatr Surg 52: 1465-1470.
[Crossref] [Google Scholar] [PubMed]
- Mirilas P, Demetriades DM, Siatitsas YS (202) Epithelial (epidermoid) splenic cysts in childhood: Surgical management of eight cases. American Surg 68: 134-138.
[Crossref] [Google Scholar] [PubMed]
- Krichen I, Maazoun K, Kitar M, Kamal NM, Khan U (2021) Huge non-parasitic mesothelial splenic cyst in a child: A case report and literature review. Clin Med Insights Pediatr 15.
[Crossref] [Google Scholar] [PubMed]
Citation: Boucebaine I, et al. (2025) Giant Epidermoid Cyst of the Spleen: A Case Report. J Univ Surg Vol.13 No.1: 070.