Lilia Rizo-Topete1, Giovanna Arteaga1, Jose G Martínez1,2, Concepcion Sanchez1, Elisa Guerrero1, Jesus Cruz1, Miguel Escobedo2,3, Homero Zapata2,3, Edelmiro Perez2,3, Marco Hernandez2,3, Gabriela Alarcon2,4, Homero Nanez2,5, Ana Silvera2 and Linda Munoz-Espinosa2,5*
1Nephrology Service, University Hospital “Dr. Jose E Gonzalez”, Universidad Autonoma de Nuevo Leon, Monterrey, Nuevo Leon, Mexico
2Transplantation Unit, University Hospital “Dr. Jose E Gonzalez”, Universidad Autonoma de Nuevo Leon, Monterrey, Nuevo Leon, Mexico
3Surgery Department, University Hospital “Dr. Jose E Gonzalez”, Universidad Autonoma de Nuevo Leon, Monterrey, Nuevo Leon, Mexico
4Pathology Department, University Hospital “Dr. Jose E Gonzalez”, Universidad Autonoma de Nuevo Leon, Monterrey, Nuevo Leon, Mexico
5Liver Unit, University Hospital “Dr. Jose E Gonzalez”, Universidad Autonoma de Nuevo Leon, Monterrey, Nuevo Leon, Mexico
Corresponding Author:
Linda Munoz-Espinosa
Transplantation Unit, University Hospital “Dr. Jose E Gonzalez”
Universidad Autonoma de Nuevo Leon, Monterrey, Nuevo Leon, Mexico
Tel: 018180297718
E-mail: marili18@hotmail.com
Received date: April 08, 2016; Accepted date: May 16, 2016; Published date: May 23, 2016
Citation: Rizo-Topete L, Arteaga G, Martinez JG, et al. Hepato-Renal Syndrome Post Liver Transplantation, Bridge Therapy with Continuous Renal Replacement Therapy in Type 1A Emergency. Successful Re-Transplant: A Case Report Arch Med. 2016, 8:3
Copyright: © 2016 Rizo-Topete L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Liver trasplantation; Hepatorenal syndrome; Continuous Renal Replacement Therapy (CRRT)
Introduction
Renal dysfunction after liver transplantation is common, with an incidence of 20 to 40%, with adverse effects on life quality and patient survival [1]. Nephrotoxicity is a common cause; however, the presentation of sudden anuria and persistent liver dysfunction forces us to suspect different pathologies.
Case Report
We present a case of a 61 years old women, diagnosed with liver cirrhosis NASH Child-Pugh C 10 and MELD 14 in May 2014 and type 2 diabetes mellitus of 10 years of evolution. She started with skin pigmentation in 2009, thrombocytopenia in 2011 and peripheral edema in 2014, she presented an episode of grade III hepatic encephalopathy on April 2014, and bleeding esophageal varices in July 2014, treated with band ligation. Chronic HBV and HCV viral markers were negative. In pre-transplant protocol echocardiography with LVEF 60%, negative for ischemia; preserved renal function with creatinine (Cr) of 0.6 mg / dL, BUN 9 mg/dL, Na 132 mEq/L, K 4.1 mEq /L, Albumin 3.3 mg/dL with GFR by MDRD 105 ml/min. She developed ascites with a good response to diuretics.
She underwent liver transplantation (LT) of deceased donor on March 2, 2015. Wedge biopsy of the donor liver was reported with 10% macrovesicular steatosis, with no evidence of inflammation, necrosis or fibrosis. Liver graft placement was performed successfully with piggybag technique, closing right hepatic vein, with no apparent complications, however it was not possible to close a hepato-renal shunt; for splanchnic edema, skin and subcutaneous tissue were closed. During peri-operative time, multiple blood transfusions were required: 9 blood packs, 6 plasmas, 6 platelet concentrates, 4 litres of 0.9% saline solution and 3 liters of Hartman solution. She passed to intensive care unit (ICU) with norepinephrine infussion, hemodinamicaly stable.
The immediate postoperative creatinine was 0.8 mg/dL and BUN 11 mg/dL. Native liver weighed 715 gr showed advanced stage cirrhosis, with 5% steatosis and Mallory Weiss bodies cell.
In the first 24 postoperative hours (PO) she had cardiogenic shock with LVEF 15%, dobutamine infusion was initiated, 48 hrs later she recovered cardiac function with LVEF 40%. However, elevation in liver function test (LFTs) was observed; AST 12,007 U/L (42), ALT 6,901 U/L (42), BT 5.6 mg/dl with lactic acidosis and LDH 21,114 U/L (180). Impaired in renal function presented with Cr 1.2 mg/dL, BUN 20 mg/dL, with a GFR by MDRD of 48.6 ml/min, 11.8 HCO3, 5.4 K mEq/L, pH 7.09, lactate 8.8, diuresis was less than 30 cc/hr. Acute kidney injury AKIN 3 was established hepato-renal síndrome. She was started on CRRT with Prisma. The SOFA and APACHE score were 13 and 22 respectively.
There was no improvement in LFTs in 24 hrs so, she was reoperated with suspected outflow obstruction. Was found a congestive liver, with color changes that improved with changes of position in color and turgidity, dig-dig graft politetrafluoroetilino (GORE-TEX®) 5 mm was placed, a biopsy was taken on suspicion of necrosis, splenorenal shunt was closed. She presented multiorganic failure (MOF) 48 hrs Pos LT, transoperative graft biopsy reported submassive necrosis 85%. Architecturally preserved; however, hepatic trabeculae were composed of eosinophilic cells with appearance of ghost, typical of necrosis, such changes predominated in Zones 2 and 3. So state 1A emergency near reported. After 48 hrs of CRRT there was improvement renal function up to 1.6 mg/dl creatinine creatinine (peak 2 mg/dL), BUN 26 mg/dL, K 3.5 mEq/L, TB 2 mg/dL and remained anuric. She presented an increase of 11kg after the 1st transplant, which achieves balance it was neutralized supported by CRRT (Table 1). Hepatic encephalopathy was documented with an ammonium elevation of 136.9 (86.9) mg/dL.
| Filter |
M 100 |
| Solution |
Priamasate |
| Blood Flow |
8O a 120 ml/min |
| Reinjecction Flux |
1000 ml/h |
| Dialysis solution |
8OO ml/h |
| Extraction |
100 ml/h |
| Dialysis dose |
37 ml/kg/h |
| Total Hours |
72 h |
| Total IT |
7800 ml |
Table 1: CRRT Indications.
Successful liver retransplantation was performed on March 5, 2015. Cavoplasty it was made, the anastomosis of hepatic thrombus showed the presence of approximately 10% of the vessel diameter. CRRT was suspended because she presented spontaneous diuresis in the immediate post-OP 300 cc/hr diuresis and creatinine was corrected 48 hours later.
At 48 hrs post-retrasplantation she presented systemic candidemia, management began with anadalofungine was began and she stabilized.
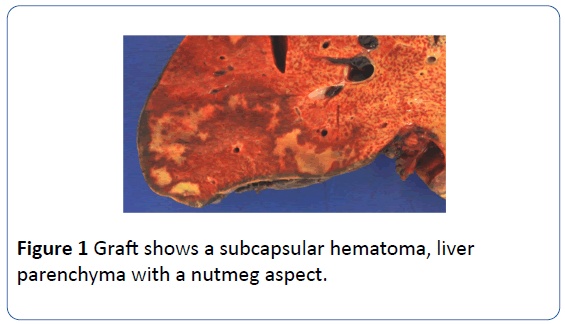
The liver explant weighed 1610 g; the capsule was grayish brown alternating with violet areas and subcapsular hematoma (Figure 1).
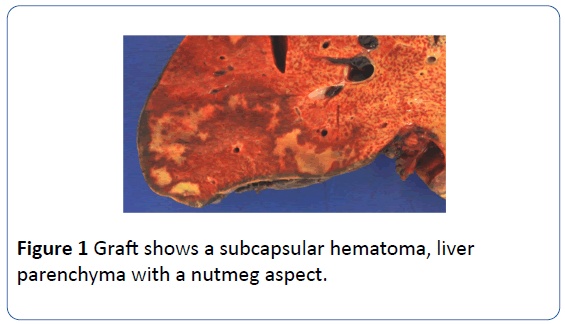
Figure 1: Graft shows a subcapsular hematoma, liver parenchyma with a nutmeg aspect.
A section of parenchyma had a nutmeg aspect. Extensive necrosis (85%) keeping only few islands of residual hepatocytes around the portal triad.
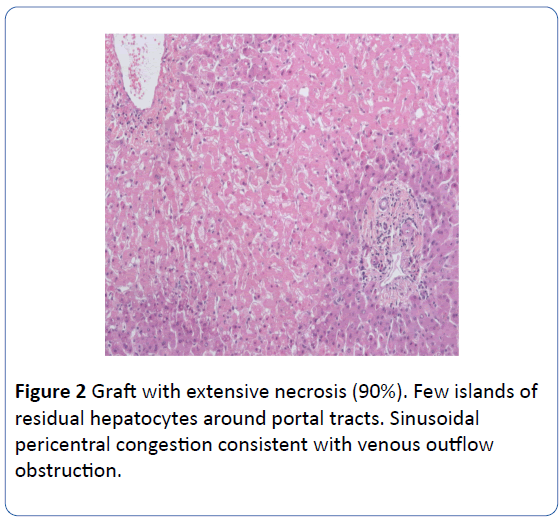
Sinusoidal congestion pericentral consistent with venous outflow obstruction (Figure 2). Portal triads without histological alterations. During her stay, she had multiple electrolyte disorders: hypernatremia, hyponatremia, hypokalemia, hypomagnesemia, hypocalcemia they were associated with the use of anadalofungina and tacrolimus.
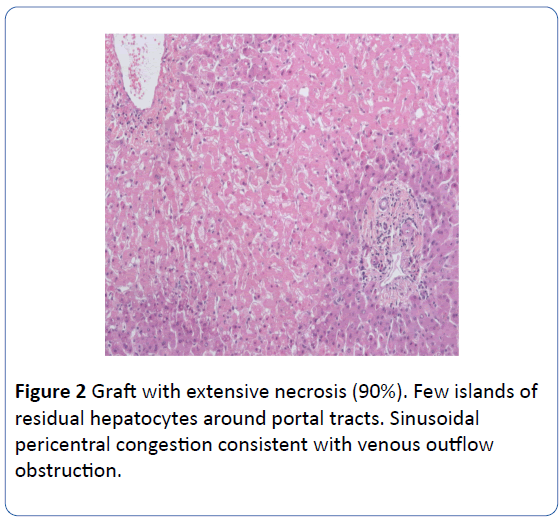
Figure 2: Graft with extensive necrosis (90%). Few islands of residual hepatocytes around portal tracts. Sinusoidal pericentral congestion consistent with venous outflow obstruction.
She was discharged on day 23 pos LT with normal liver and kidney function: Hb 11.3 mg/dl, Platelets 384 000, TTP 27.1, INR 1.06, AST 26 U/L (42), ALT 45 U/L (42), ALB 2.9 mg/dl, BT 1.3 mg/dl , Cr 0.6 mg/dl , BUN 11 mg/dl. She lost 12 kg during her hospital stay, with satisfactory evolution. After 7 months of her LT she is asymptomatic with normal liver and kidney function.
Discussion
Primary graft non-function (PGNF) following LT is a lifethreatening clinical condition [1-3], which is manifested by severe liver cytolysis, increasing transaminasemia, hypoalbuminemia, hepatic coagulopathy, hyperlactatemia, hyperbilirubinemia, hemodynamic instability, hypoglycemia and acute renal failure [1]. Coagulative necrosis of the liver graft is evident in the biopsy [1-3]. PGNF affects 2-23% of patients undergoing LT [1-3]; and has been defined more specifically as the cause of liver failure, that led to retransplantation or death within the first week posttransplant, in which technical, vascular, and immunological causes have been ruled out [2]. Multiple factors are involved in graft function. Among these risk factors are extended cold ischemia time, female donor gender, increased donor age, donor intensive ICU, donations after cardiac death, protracted operating room time, liver graft steatosis, decreased graft size, and renal failure [2]. At the present PGNF is the most common indication for early retransplantation, since this surgical procedure still represents the only treatment option. The patient reported here fulfilled criteria for PGNF with hemodynamic instability, need for inothropics, hepatic encephalopathy persistently elevated liver enzymes, MOF, and massive graft necrosis. She had an advanced Child-Pugh classification preLT, as well as hyponatremia, hypoalbumineia and thrombocytpopenia as to risk factors for postop PGNF [4].
Acute kidney injury (AKI) is common in patients with decompensated cirrhosis. AKI is defined as significant reduction in glomerular filtration rate, a rise in serum creatinine level of at least 2 fold from baseline or an absolute increase a serum creatinine level more than .3 mg/dL or a diuresis less than 0.5 ml/kg/h in 6 hours [5]. Pre LT renal failure has been associated with postoperative AKI [6], our patient had a type 2 HRS pre LT and a type 1 HRS posLT. As regard to donor risk factors for AKI only one was identified as deceased donor [3]. AKI was associated with grade IV graft dysfunction [4]. Oliguria in the immediate postop period was the early indication for CRRT [4,6,7]. AKI posLT is due to ATN in 70% of cases [4].
In a multivariate analysis for risk factors for CRRT hepatic encephalopathy, deceased donor, advances MELD score, intraoperative blood loss, hepatocellular carcinoma (as the indication for LT). This has led to de development of mathematical models for an early identification of cases [8].
It has been suggested that 5% of secondary LRA LT require CRRT. It has been shown that weight gain of over 10% in ICU morbidity and mortality increases, why should be evaluated at an early stage the use of CRRT in anuric patients and intensive resuscitation.
Conclusion
The continuous elevated transaminases suggest significant hepatic necrosis. Etiological reasons of early graft dysfunction after transplantation must be ruled out such as ischemia, reperfusion injury, PGNF, technical complications, rejection and infection.
It has been suggested that 5% of secondary LRA LT require CRRT. It has been shown that weight gain of over 10% in ICU morbidity and mortality increases, so it should be evaluated at an early stage the use of CRRT in anuric patients.
9585
References
- Contreras AL (2014) Post Operative Care of the Liver Trasplantation Patients in Mount Sinai Expert Guides, Hepatology.
- Bonder A, Botero M, Cardenas A (2014) Current Therapies for Hepatorenal Syndrome, Current Hepatology.
- Kim JM, Jo YY, Na SW, Kim SI, Choi YS, et al. (2014) The predictors for continuous renal replacement therapy in liver transplant recipients. Transplant Proc 46: 184-191.
- Munoz LE, Cordero P, Cura I (2013) Hepatic Failure as an Early Complication Following Orthotopic Liver Trasplantation . Liver Failure Etiologies, Neurological Complications and Emerging Therapies, Nova Science Publishers, New York.
- Davis EG, Florman SS (2014) Primary Non Function in Mount Sinai Expert Guides, Hepatology.
- Cabezuelo JB, Ramírez P, Rios A, Acosta F, Torres D, et al. (2006) Risk factors of acute renal failure after liver transplantation. Kidney Int 69: 1073-1080.
- Weber ML, Ibrahim HN, Lake JR (2012) Renal dysfunction in liver transplant recipients: evaluation of the critical issues. Liver Transpl 18: 1290-1301.