Keywords:
Cardiac resynchronization therapy; Ejection fraction; Electrocardiogram; QRS complex.
Introduction
Cardiac Resynchronization Therapy (CRT) has emerged as an effective option in treating patients with symptomatic heart failure resulting from systolic dysfunction. CRT is only one aspect of the treatment of patients with heart failure [1].
Progression of left ventricular dysfunction to heart failure with low ejection fraction (EF) is frequently accompanied by impaired electro mechanical coupling, which may further diminish effective ventricular systolic function [1,2].
Cardiac resynchronization therapy is the term applied to reestablishing synchrony between left ventricular free wall and ventricular septal contraction in an attempt to improve left ventricular efficiency and subsequently improve functional class in patients with heart failure [3].
Cardiac resynchronization therapy has been proposed as a treatment of patients with idiopathic as well as ischemic left ventricular dysfunction with drug refractory heart failure and intra or inter ventricular conduction delay [1,4,5].
The proven benefit of CRT includes improvement in heart failure symptoms, exercise capacity (6 minutes’ walk distance), quality of life, reduces heart failure re-hospitalization, induce LV reverse remodeling and improves systolic function [1,2].
The mechanical and hemodynamic effect of CRT occurs rapidly essentially within a beat after implantation as a consequence of improvement of excitation contraction coupling which is usually impaired in heart failure patients [6,7].
The chronic effect of CRT occurs through reduction in endsystolic and end-diastolic volumes, improvement in LVEF % and improvement in heart failure symptoms and quality of life within six months of implantation as observed by most studies of CRT patients [6,8].
Cardiac resynchronization therapy (CRT) has been shown to reduce the risk of death due to heart failure (HF), improves functional status of left ventricle (LV) in patients with advanced HF and improves LV dysfunction in patients with a wide QRS complex [9].
Several studies have been conducted to study the effect of CRT on clinical outcome and to determine the unique inclusion criteria for selection of patients [6-8].
Materials and Methods
Aim of the work
The aim of the present work is to detect the long term effect of CRT on clinical outcome in patients with HF.
Patients and methods
A total of 192 patients were successfully implanted with CRT in Critical Care Medicine Department, Cairo University. Only 180 patients (146 males and 34 females) completed their follow-up visits (at least 6 months after implantation), 11 patients died and one patient was lost during follow-up.
The indication of CRT implantation was New York Heart Association (NYHA)class II, III and ambulatory IV heart failure, Left Bundle Branch Block(LBBB) and QRS duration ≥ 120 ms or non LBBB with QRS duration ≥ 150 with ejection fraction (EF) ≤ 35%. Patients with recent myocardial infarction, sever valvular heart lesions and sever pulmonary hypertension are not subjected to this procedure.
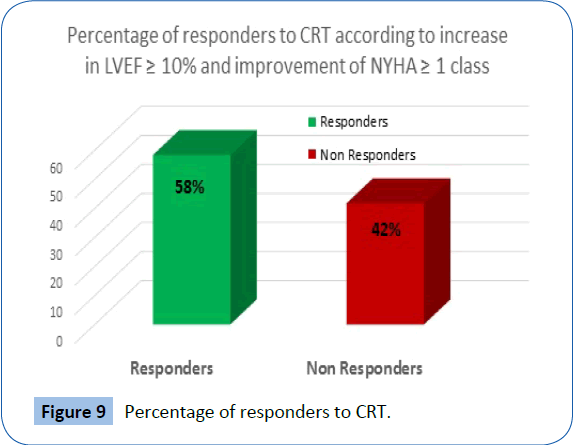
In our study the Candidates were considered responders to CRT if there was an increase in LVEF ≥ 10% and increase in NYHA class ≥ 1 after 6 months from CRT implantation.
The following data were obtained from the follow-up files of the patients at the pacemaker follow-up clinic, the main archiving system of the critical care department, Cairo University, electronic records of the critical care department, Cairo University and direct personal contact as well and include:
• Personal history (name, age, sex).
• History analysis and clinical examination.
• Assessment of the NYHA class.
• Indications for CRT implantation.
• CRT implantation data including (route of implantation, site of coronary sinus lead)
• 12 lead ECG to assess QRS morphology, width and axis and adequacy of capturing and sensing.
• Plain X-ray chest to detect leads positions and any complications e.g pneumothorax.
• Echocardiography to detect contractility of the heart, LV dimensions, degree of MR, and post implantation complications like hemopericardium in addition to vegetation or masses involving CRT leads.
• Pacemaker malfunction and complications and how they were managed.
Statistical methods
Data were statistically described in terms of mean ± standard deviation (± SD), frequencies (number of cases) and percentages when appropriate.
Comparison of numerical variables between the study groups was done using Student t test for independent samples. For comparing categorical data, Chi square (χ2) test was performed. Exact test was used instead when the expected frequency is less than 5. Accuracy was represented using the terms sensitivity and specificity.
p values less than 0.05 was considered statistically significant. All statistical calculations were done using computer programs SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) version 15 for Microsoft Windows.
Results
Our study included 180 patients (146 males and 34 females) with a mean age 56.7 ± 8.7 years who were successfully implanted with CRT in Critical Care Medicine Department, Cairo University.
Baseline data Underlying heart disease and NYHA Class
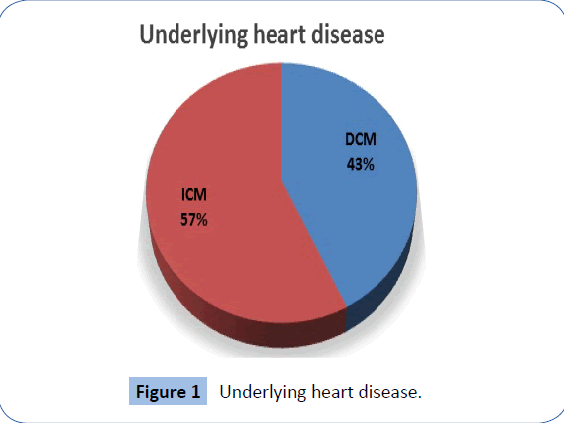
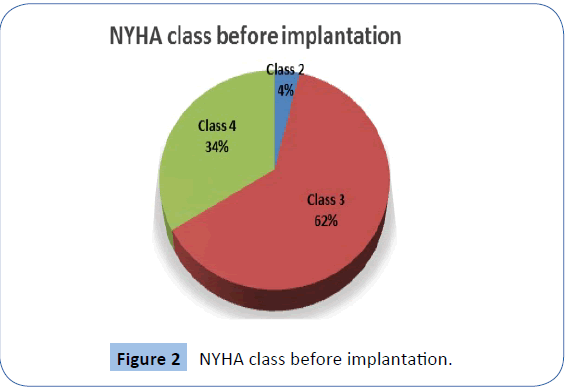
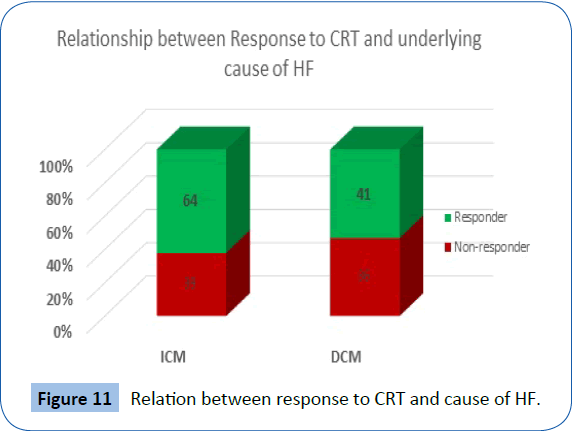
There were 103 patients (57.2%) with Ischemic Cardiomyopathy (ICM) and 77 patients (42.8) with Dilated Cardiomyopathy (DCM). Most of the patients presented with NYHA class III as shown in Figures 1 and 2.
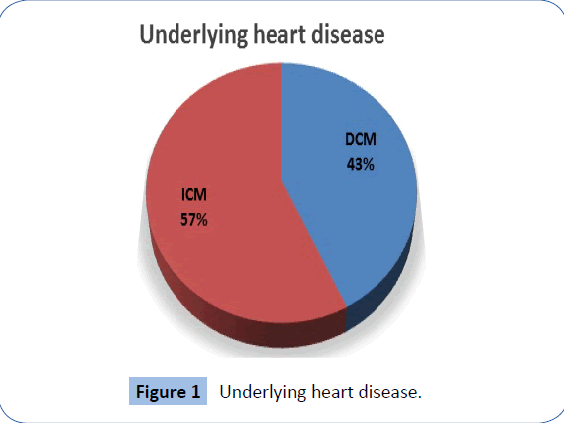
Figure 1: Underlying heart disease.
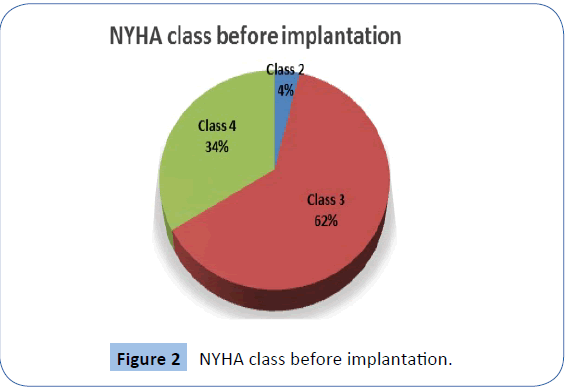
Figure 2: NYHA class before implantation.
ECG Data before implantation
ECG rhythm was sinus in 162 (90%) patients and atrial fibrillation in 18 (10%) patients. The mean QRS complex duration was 135.6 ± 15.1 msec. and the QRS morphology was LBBB in most of the patients as shown in Table 1.
| QRS |
Frequency |
| LBBB |
169 (93.8%) |
| RBBB |
5 (2.7%) |
| IVCD |
6 (3.3%) |
| Paced |
2 (1.1%) |
Table 1: QRS morphology before implantation.
Echocardiographic data before CRT implantation
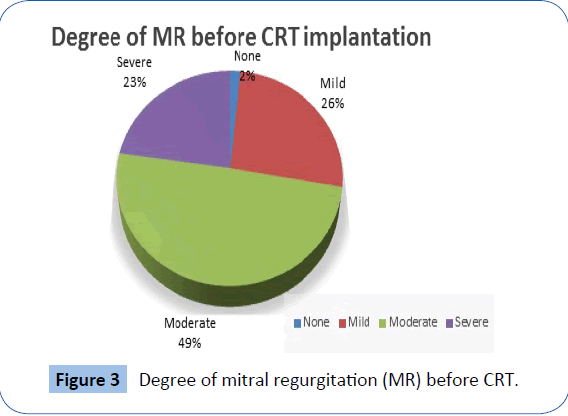
The mean LVEF % before implantation was 30.7 + 4.3%. Other echocardiographic data is shown in Table 2 and Figure 3.
| QRS |
Frequency |
| LBBB |
169 (93.8%) |
| RBBB |
5 (2.7%) |
| IVCD |
6 (3.3%) |
| Paced |
2 (1.1%) |
Table 2: LVEF and LV dimensions before CRT implantation.
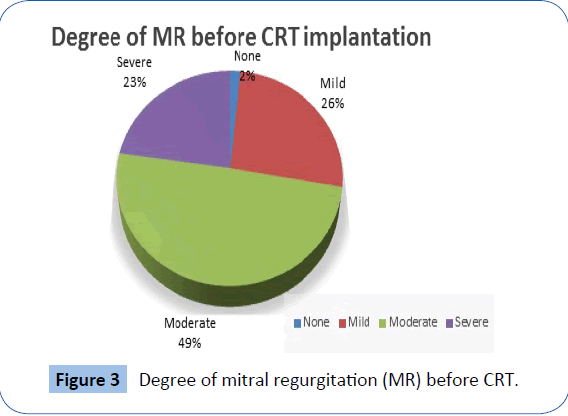
Figure 3: Degree of mitral regurgitation (MR) before CRT.
Cardiac resynchronization therapy implantation and complication
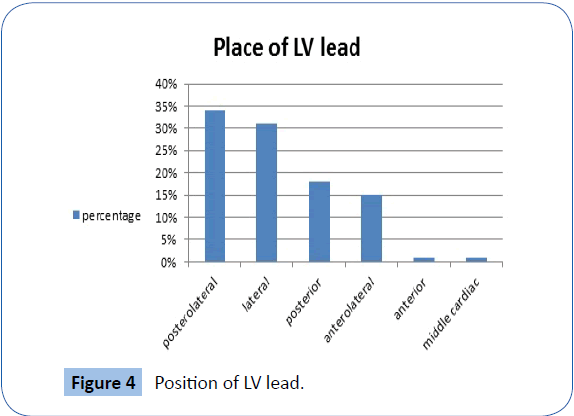
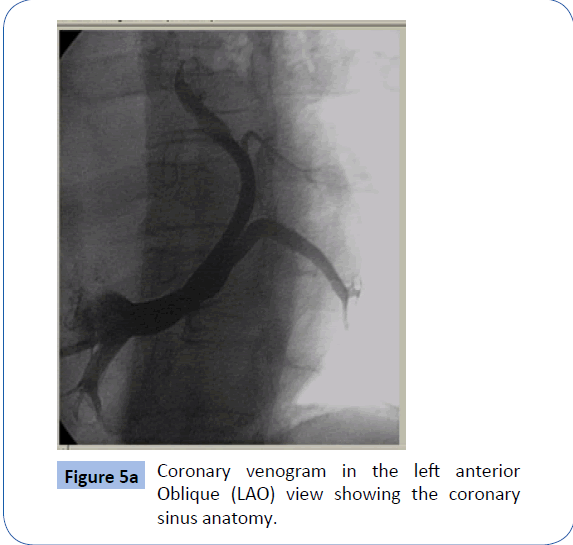
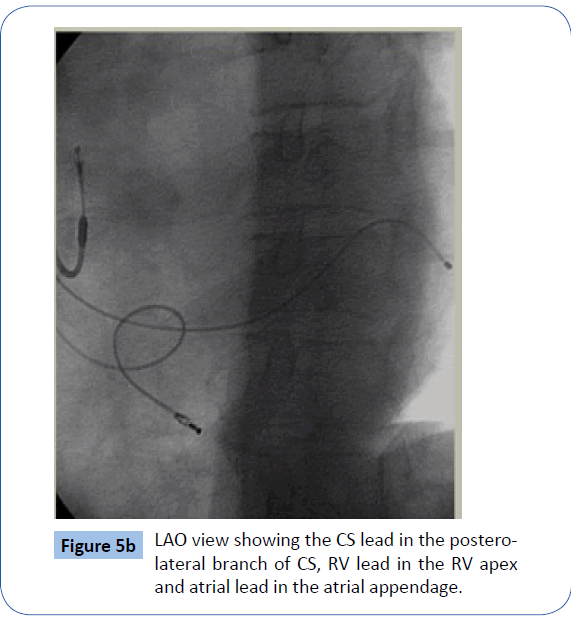
All the patients had the CRT device(143 CRT-Pacemaker and 49 CRT-Defibrillator) implanted, where 3 leads were implanted; one in the right ventricle (RV), one in the right atrium and the left ventricular (LV) lead was implanted via coronary sinus(CS) directed mainly to pace the lateral wall of the left ventricle as shown in Figures 4, 5a and 5b.
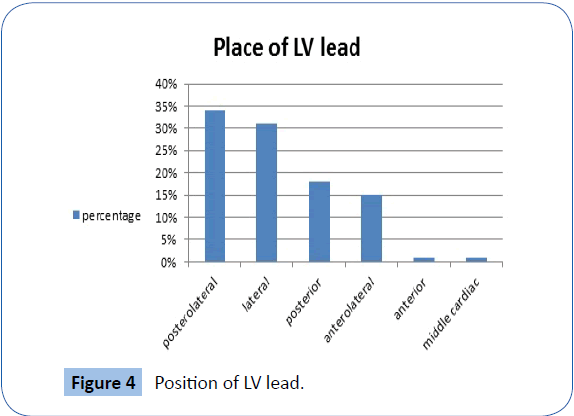
Figure 4: Position of LV lead.
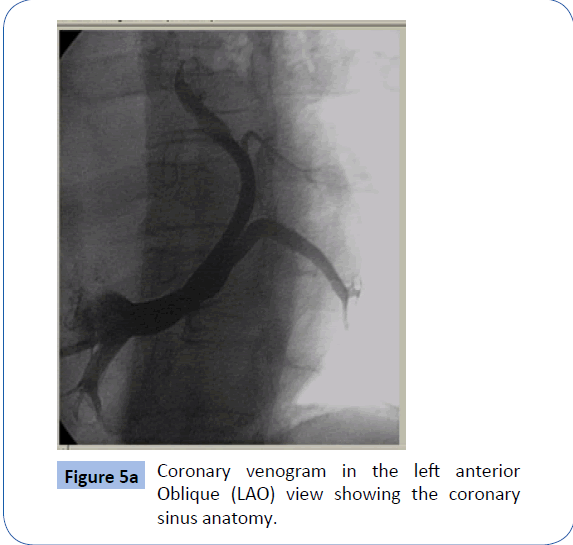
Figure 5a: Coronary venogram in the left anterior Oblique (LAO) view showing the coronary sinus anatomy.
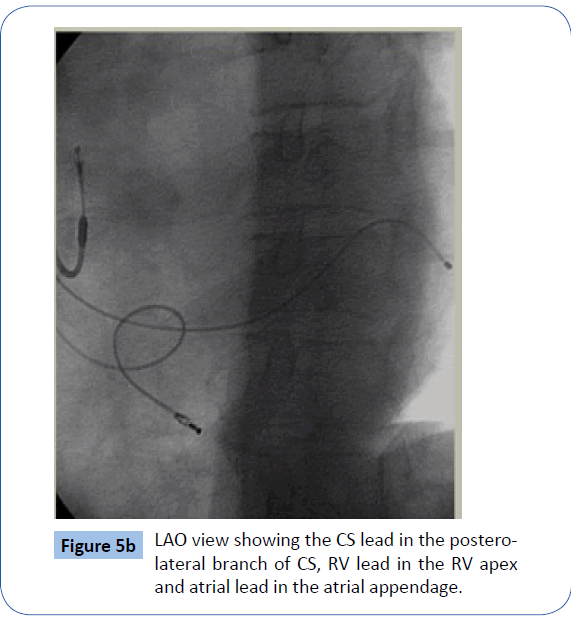
Figure 5b: LAO view showing the CS lead in the posterolateral branch of CS, RV lead in the RV apex and atrial lead in the atrial appendage.
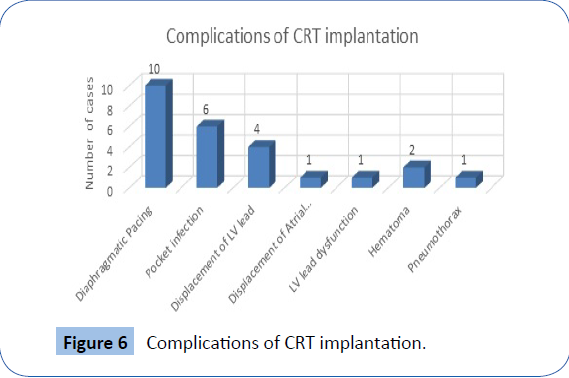
In our study complications occurred only in 25 patients (13.8%), diaphragmatic pacing was the most common complication occurred as shown Figure 6.
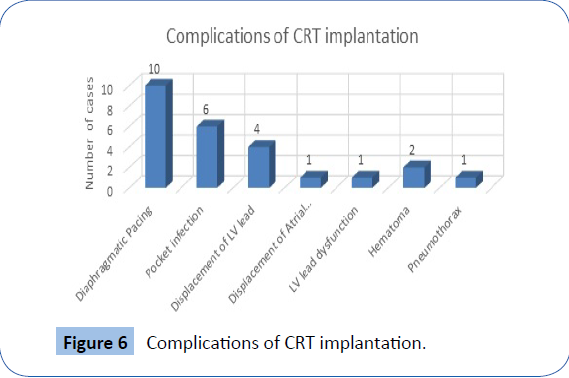
Figure 6: Complications of CRT implantation.
Post implantation data and comparing it with baseline data
NYHA class
There was a significant improvement of NYHA class after CRT implantation (P value<0.001), 72.2% of patients improved with at least 1 NYHA class, 61.6% improved in one NYHA class, 10.55% showed an improvement of two NYHA classes and 27.8% did not improve in NYHA class after CRT implantation (Table 3).
| NYHA |
Pre CRT |
Post CRT |
P-Value |
| Class 2 |
7 (3.8%) |
80 (44.4%) |
|
| Class 3 |
112 (62.2%) |
97 (53.8%) |
| Class 4 |
61 (33.8%) |
3 (1.6%) |
| Mean NYHA |
3.3 +/- 0.5 |
2.6 ±0.5 |
<0.001 |
Table 3: NYHA class before and after pacing.
QRS width
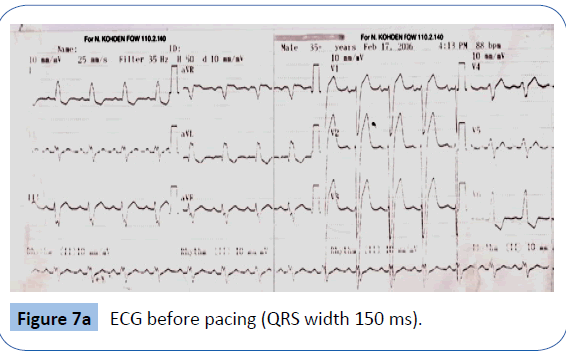
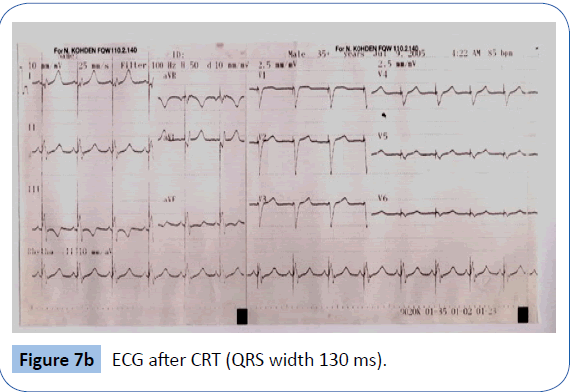
There was a significant decrease in QRS width after CRT implantation (P value<0.001). As shown in Table 4 and Figures 7a and 7b.
| |
Pre-CRT |
Post-CRT |
P-value |
| Mean |
SD |
Mean |
SD |
| QRS duration |
135.6 |
15.1 |
105.9 |
13.7 |
<0.001 |
Table 4: Duration of QRS complexbefore and afterpacing.
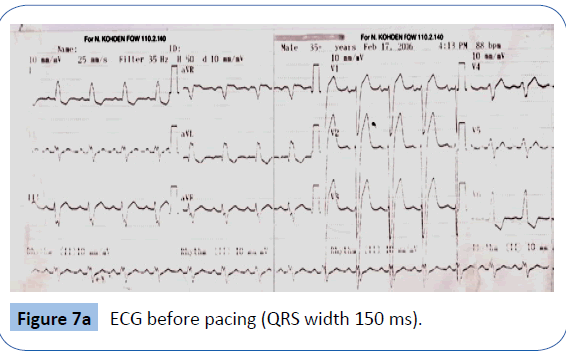
Figure 7a: ECG before pacing (QRS width 150 ms).
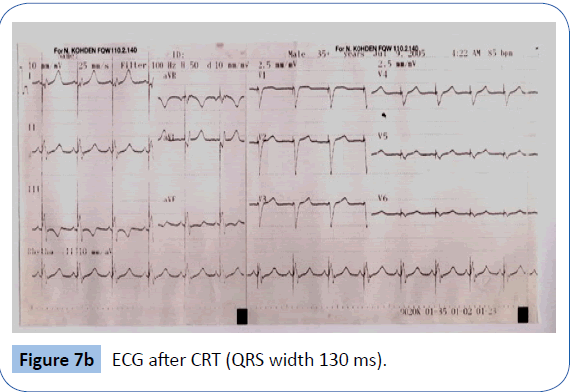
Figure 7b: ECG after CRT (QRS width 130 ms).
Echocardiographic data
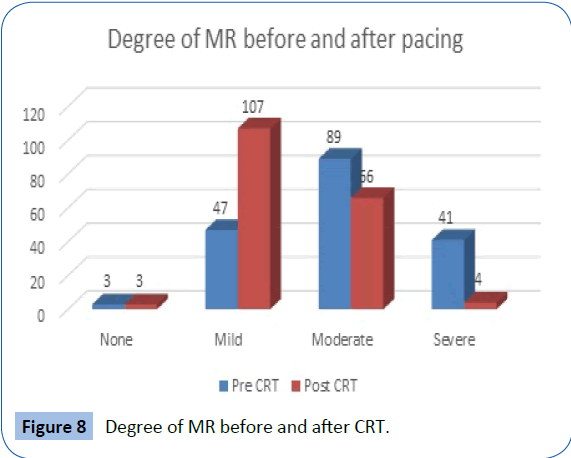
There was a significant improvement of LVEF%, LVEDd and LVESd (P value<0.001) after CRT implantation. Also there was an improvement in the degree of MR after CRT implantation Table 5 and Figure 8.
| |
Pre-CRT |
Post-CRT |
P-value |
| Mean |
SD |
Mean |
SD |
| LVEF% |
30.70% |
4.3 |
36.60% |
4.1 |
<0.001 |
| LVEDd |
71 mm |
7 |
65 mm |
7 |
| LVESd |
60 mm |
7 |
55 mm |
7 |
cTable 5: EF and LV dimensions pre and postpacing.
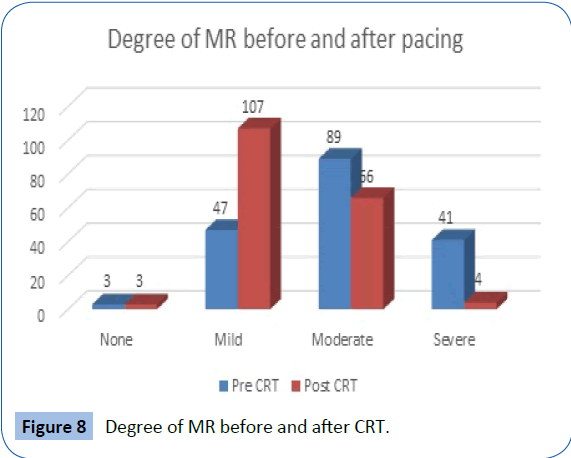
Figure 8: Degree of MR before and after CRT.
Cardiac Resynchronization Therapy responders
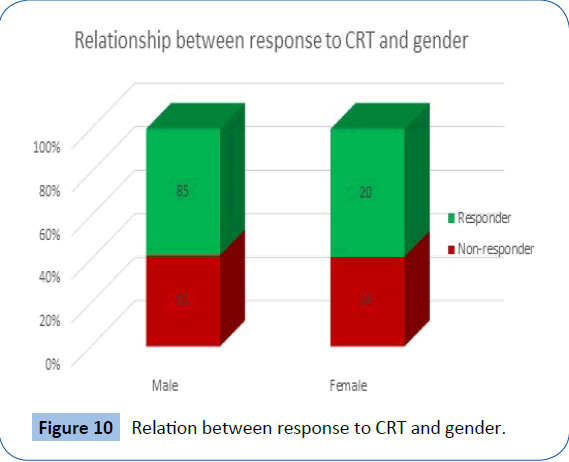
The Candidates were considered responders to CRT if there was an increase in LVEF ≥ 10% and improvement in NYHA class ≥ 1 class after CRT implantation, we found that 105 patients (58.33%) were considered responders and 75 patients (41.66%) were not responders. We did not found significant differences between responders and non-responders either in gender or the underlying heart disease (Figures 9-11).
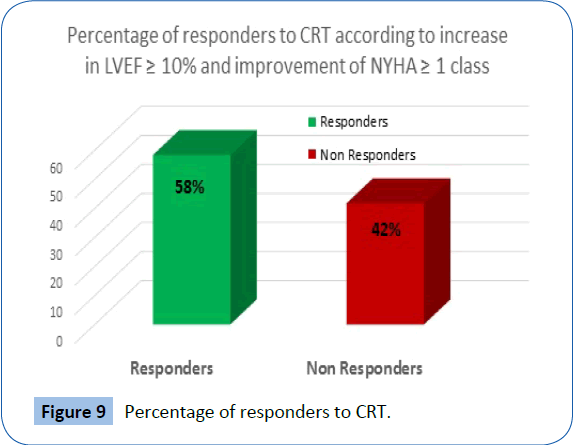
Figure 9: Percentage of responders to CRT.
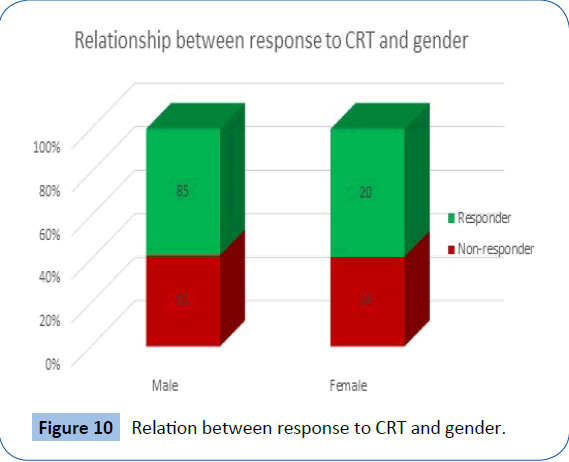
Figure 10: Relation between response to CRT and gender.
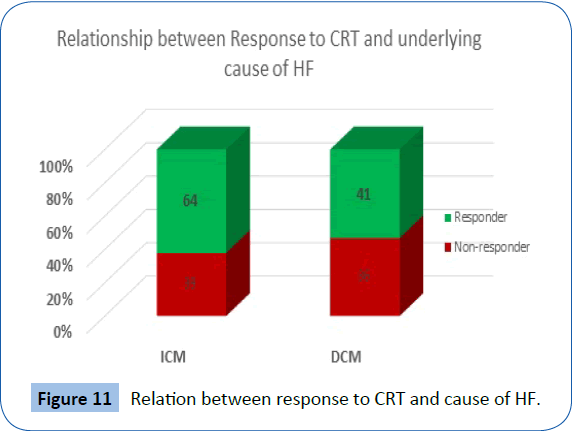
Figure 11: Relation between response to CRT and cause of HF..
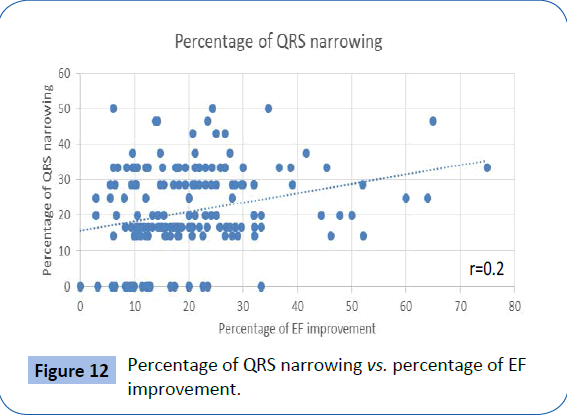
Correlation between QRS width and improvement in LVEF% after CRT implantation
In our study, as the percentage of decrease in QRS width after CRT implantation increased, there was a significant improvement in LVEF % after CRT implantation, (P-value<0.01). This is shown in Figure 12.
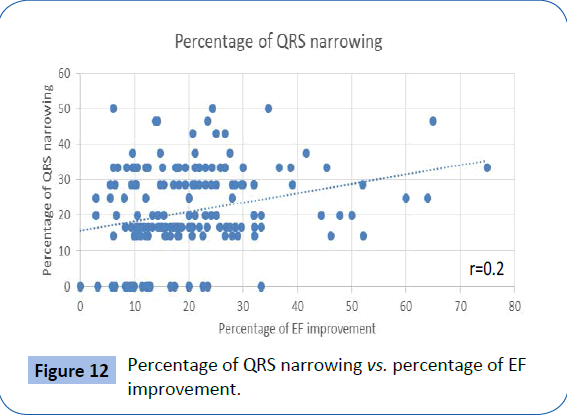
Figure 12: Percentage of QRS narrowing vs. percentage of EF improvement.
Mortality after CRT implantation
Eleven patients died (5 with refractory heart failure, 4 with sudden cardiac death, 1 with cerebrovascular accident and 1 with lymphoma).
The underlying cardiac pathology of the 11 mortality patients was ischemic in 7 patients and idiopathic in 4 patients and the functional class was NYHA IV in 8 patients and NYHA III in 3 patients. The underlying rhythm was sinus in 10 patients and AF in one patient.
Discussion
Cardiac Resynchronization Therapy (CRT) has emerged as an effective option in treating patients with symptomatic heart failure resulting from systolic dysfunction. CRT is only one aspect of the treatment of patients with heart failure [1].
Cardiac Resynchronization Therapy has been shown to improve heart failure, reduce the risk of death and improve the status of LV dysfunction. However, a number of patients remain unresponsive to the therapy. The cause of unresponsiveness has been an issue of research in many trials and has a concern in follow-up of CRT patients [3,10-12].
In our study there were 103 patients (57.2%) had ischemic cardiomyopathy (ICM) and 77 patients (42.8%) had dilated cardiomyopathy (DCM), The large number of patients with ICM in our study was attributed to the large number of ischemic patients in our community and with advance in their management in our department including primary intervention, the mortality rate reduced and some of them became myopathic.
Contrary to our expectations there was no significant difference (P-Value 0.3) in response to CRT between patients with ICM and patients with DCM.
In our study, the position of LV pacing lead was in posterolateral branch of coronary sinus in 62 patients (34.3%), lateral branch in 55 patients (30.6%), posterior branch in 32 patients (17.8%), anterolateral branch in 28 patients (15.6%), and 3 patients in non-optimal position (anterior and middle cardiac branches), and we tried to follow the data obtained from the sub-analysis of MADIT-CRT which showed that an apical LV lead position resulted in a significant increased risk for heart failure and death [13] by inserting the leads in basal or mid ventricular position rather than an apical position.
In our study the rate of complications was low reflecting the experience of our center in this field. Complications occurred only in 25 patients (13.8%), most of them (10 cases) were diaphragmatic pacing which were corrected by reprogramming the device except in one patient who was managed by replacing the battery with another one with more LV pacing configuration. Six cases with pocket infection 2 of them were managed by removing the old system and re-implantation in the other side, after complete recovery of infection and the other 4 cases, the infection was mild and superficial and they were managed by IV antibiotics and local dressing. Four cases with LV lead displacement and repositioning was done, one case with LV lead dysfunction and the lead was changed and 1 case with atrial lead displacement and repositioning was done. Two cases with hematoma with conservative measures, one case with pneumothorax and intercostal chest tube was inserted then removed after expansion of the lung occurred.
Our study focused on the pre and post implantation echocardiographic changes that occur in patients after CRT implantation and the effect of CRT on clinical outcome of patients within months after implantation.
In our study and in concordance to other major and small studies there was a significant decrease in LV diameters, increase in EF% (P-value<0.001) and reduction in MR degree 6 months after CRT implantation [14-16].
Mitral regurgitation is one of the echocardiographic changes that predict CRT reverses remodeling and clinical improvement.
This improvement in MR could be explained by the effect of resynchronization on the papillary muscles and the better cooptation of the leaflets as a result of this synchronization. The decrease in the contraction time possibly leads to a decrease in the MR. The reverse remodeling and reduction of the LV dimensions can explain further improvement at follow-up.
Further investigations are warranted to combine CRT with specific MR therapeutic approaches such as surgical annuloplasty or percutaneous therapies to maximize the effect of CRT in MR patients [17].
In our study, The Candidates considered responders to CRT if there was an increase in LVEF ≥ 10% after CRT and improvement in NYHA class ≥ 1 class 6 months after CRT implantation and according to this 105 patients (58.33%) were considered responders and 75 patients (41.66%) were not responders and this rate is in concordance with other studies [10-12,18,19].
In a trial to find any predictor to CRT response, gender and underlying heart disease failed to predict this response but ECG succeeded to predict CRT response where in our study when we correlated between the QRS width and improvement in LVEF% after CRT implantation, we found that there was a significant improvement in LVEF% as the percentage of decrease in QRS width increased (P-value <0.01).
Our results agreed with the study of Cazeau et al. [20], who studied 100 patients with successful CRT implantation, he found that 63 patients had a decrease in QRS complex post CRT implantation and as the percentage of decrease in QRS width after implantation increased; there was an improvement in LVEF % and clinical outcome post implantation [20].
The results of Zhang et al. were in concordance with our study as he studied 132 patients with different QRS durations in 3 groups, a group of Cardiac Contractility Modulation therapy, CRT group with narrow QRS complex and a third group with CRT and a wide QRS complex. Cardiac Contractility Modulation (CCM) is a new device therapy for advanced heart failure due to systolic dysfunction. It works by applying a relatively high voltage electrical signal to the myocardium during the absolute refractory period of the contractile cycle [21].
The study found that there was a significant improvement in CCM group in NYHA class and life style of the patients but better results were observed in CRT group patients who had a wide QRS complex ≥ 150 ms [21].
Approximately 200 CRT devices were implanted in Critical Care Medicine Department, Cairo University. We tried to help the poor patients with severe heart failure refractory to medical treatment. The patients showed variable degrees of improvement and we achieved acceptable experience in this field.
Conclusion
Cardiac resynchronization therapy had great positive impact on clinical outcome in patients with congestive heart failure and according to our experience in this field CRT implantation is safe and with low rate of complications.
20136
References
- Stickberge A, Corti J, Dauod E (2010)Patient selection for cardiac resychronization therapy.Circulation111:2146-2150.
- Willerson JT, Kereiakes DJ (2004) Cardiac resynchronization therapy: Helpful now in selected patients with CHF. Circulation 109:308-309.
- DavidLH, Josephy GM (ed), Margaretal(ed) (2008) Cardiac resynchronization therapy mayo clinic cardiology.3rdedn., 34:467-447.
- Gimelli A, Frumento P, Valle G (2010)CRT in patients with heart failure time course of perfusion and wall motion changes. AM J Cardiol 2010: 1-5.
- Moss AJ, Hall JW,Cannom DS (2009) Cardiac resynchronization therapy for prevention of heart failure events. N Engl J Med 361: 1329-1338.
- William TA, Baliga RR (2010)Cardiac resynchronization therapy in heart failure.Lippincott Williams & Wilkins, USA, p:208.
- Ypenburg C, Van De Veire N, Westenberg J(2009)Non Invasive imaging in cardiac resynchronization therapy: Follow-up and optimizing setting. Pacing Clin Electrophysiol 31:1628-1639.
- Antman EM (2007)Cardiovascular therapeutics a companion to Braunwald’s Heart Disease. 3rd edn., Patricia Tannian, pp: 366-386.
- Pouluer AC, Knappe D, Shah AM (2011) Relationship between left ventricular dysshnchrony and contractile function and clinical outcome in cardiac resynchronization therapy: The MADIT-CRT trail. Eur Heart J 32: 1720-1729.
- Russo AM, Stainback RF, Bailey SR (2013)ACCF/HRS/AHA/ASE/HFSA/SCAI/SCCT/SCMR 2013 appropriate use criteria for implantable cardioverter-defibrillators and cardiac resynchronization therapy: A report of the American College of Cardiology Foundation appropriate use criteria task force, Heart Rhythm Society, American Heart Association, American Society of Echocardiography, Heart Failure Society of America, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol61: 1318-1368.
- Dupont M, Rickard J, Baranowski B (2012) Differential response to cardiac resynchronization therapy and clinical outcomes according to QRS morphology and QRS duration. J Am Coll Cardiol60: 592-598.
- Sipahi TP, Carrigan DY, Rowland (2011) Impact of QRS duration on clinical event reduction with cardiac resynchronization therapy: Meta-analysis of randomized controlled trials. Arch Intern Med171: 1454-1462.
- Singh JP, Klein HU, Huang DT, Reek S, Kuniss M, et al. (2011) Left ventricular lead position and clinical outcome in the multicenter automatic defibrillator implantation trial-cardiac resynchronization therapy (MADIT-CRT) trial. Circulation123:1159-1166.
- Van Bommel RJ (2010) Morbidity and mortality in heart failure patients treated with cardiac resynchronization therapy: influence of pre-implantation characteristics on long-term outcome. Eur Heart J 31: 2783-2790.
- Holzmeister J, Leclercq C (2011) Implantable cardioverter defibrillators and cardiac resynchronisation therapy. Lancet 378: 722-730.
- Goldenberg I, Moss AJ, Hall WJ, Foster E, Goldberger JJ, et al. (2011) Predictors of response to cardiac resynchronization therapy in the multicenter automatic defibrillator implantation trial with cardiac resynchronization therapy (MADIT-CRT). Circulation124: 1527-1536.
- Cabrera-buneno F, Jose Molina-Mora M, Alzueta J(2010)Persistence of secondary mitral regurgitation and response to cardiac resynchronization therapy. Eur J Echocardiogr 11: 131-137.
- Chatterjee NA, Kandala J, Parks KA, Lewis GD,Singh JP (2012)RV dilation and geometric remodeling impact mortality in cardiac resynchronization therapy. Circulation 126: A16919.
- Ypenburg C (2009)Long-term prognosis after cardiac resynchronization therapy is related to the extent of left ventricular reverse remodeling at midterm follow-up. J Am Coll Cardiol 53: 483-490.
- Cazeau S, Leclercq C, Lavergne T(2001)Effects of multisite biventricular pacing in patients with heart failure and intraventricular conduction delay. N Engl J Med344: 873-880.
- Zhang Q, Chan YS, Liang YJ (2012)Comparison of left ventricular reverse remodeling induced by cardiac contractility modulation and cardiac resynchronization therapy in heart failure patient with different QRS duration. Int J Cardiol 167: 889-893.