Research Article - (2023) Volume 15, Issue 5
“Improving efficiency in healthcare: Effects of deploying electronic claims management system on the implementation of a sub-national health insurance schemes in Anambra state, Nigeria”
Uchenna Ezenwaka1,2 and
Simeon Onyemaechi3*
1Department of Health Administration and Management, Faculty of Health Science and Technology, University of Nigeria Enugu Campus, Enugu, Nigeria
2Health Policy Research Group, College of Medicine, University of Nigeria Enugu Campus, Nigeria
3Anambra State Health Insurance Agency, Awka, Anambra State, Nigeria
*Correspondence:
Simeon Onyemaechi, Anambra State Health Insurance Agency, Awka, Anambra State,
Nigeria,
Tel: +234 8036740872,
Email:
Received: 22-Jul-2023, Manuscript No. ipaom-23-13961;
Editor assigned: 24-Jul-2023, Pre QC No. P-13961;
Reviewed: 05-Sep-2023, QC No. Q-13961;
Revised: 11-Sep-2023, Manuscript No. R-13961;
Published:
19-Sep-2023
Abstract
Objective: As healthcare becomes increasingly important to the
economic and social development of any nation, the problems
healthcare providers face in terms of efficiency and speed of
service delivery need to be addressed. By deploying an electronic
claims management system, these issues can be resolved, leading
to improved efficiency in healthcare. This study examines the
effects of deploying an electronic claims management system on
the implementation of a sub-national health insurance scheme in
Anambra State (ASHIS), Nigeria.
Methods: A qualitative study was conducted in Anambra state,
Nigeria. Data were collected from stakeholders- health insurance
managers and ASHIS-accredited healthcare providers- who play
critical roles in claims management. Twenty in-depth interviews
were conducted with the stakeholders to explore their experience
and effectiveness of electronic claims management system. Data
were analysed using a thematic approach.
Results: Manual claims management was stated to be cumbersome,
time-consuming and error prone. The analysis revealed that
implementation of the electronic claims management system
increased the efficiency of the ASHIS in terms of speed, accuracy,
transparency, convenience and cost savings. Furthermore, the
system also resulted in greater customer satisfaction among the
health service users. However, few respondents claimed that poor
internet connectivity often challenges the process.
Conclusion: The study highlights the importance of deploying
electronic claims management systems in providing efficient
healthcare services, hence, the need to ensure its sustainability.
Keywords
Anambra state health insurance scheme; Claims; E-claims
management system; Reimbursement
Introduction
In recent times, increasing global commitment to
Universal Health Coverage (UHC) has triggered health
financing policies and investments to improve access to
health services and financial risk protection, particularly
in many Low- and Middle- Income Countries (LMICs)
[1]. Globally, social health insurance has been recognized
as a strong and important financing mechanism capable
of enhancing access to care and improving financial
protection by mitigating the detrimental effects of user
fees towards the attainment of UHC [2]. Consequently,
many developing countries have introduced social health
insurance schemes [3,4].
However, the performance of the health financing
mechanisms adopted largely depends on the provider
payment and service delivery methods. Globally, the
predominant Provider Payment Mechanisms (PPM) used
include Fee-For-Service (FFS), capitation, Diagnostic-
Related Group (DRG) and mixed payment methods [5].
Although these PPM assisted in shaping health financing,
health outcomes and access to quality healthcare are
somewhat attributed to the way health providers’ claims
for services delivered are reimbursed [6]. This implies that
the claims management system – submission, processing
and reimbursement of claims is critical to the success of
any health insurance system. For instance, delayed and
unpredictable reimbursement of claims to health providers
is proven to challenge the efficient delivery of healthcare
to clients [7-9] and threatens the sustainability of health
insurance schemes [10].
Manual system of claims management has been proven
to result in unpaid claims due to errors and fraudulent
claims [11]. Evidence shows that given the complex nature
of claims management, the huge cost of a manual (paperbased)
claims management system poses major threat to the
performance and sustainability of health insurance schemes
[12]. Consequently, insurance agencies seek efficient and
innovative methods such as full digitalization of operations
using electronic claims (e-claims) management system
which significantly improve operational efficiency in
healthcare financing, which is considered critical for a wellfunctioning
healthcare system [13].
Several studies have underlined the benefits derived
from digitalizing claims management over a paper-based
claims system, including allowing for cost-reallocation;
facilitating automated pre-payment control; reducing
error and fraudulent claims; providing transparent and
reliable processes; cost-savings by freeing staff from tedious
schedules [14] and reduction of denied claims costs [12].
Hence, digitalizing every step of claims management, from
submission of claims to reimbursement, has the potential
to boost operational efficiency and overall performance of
a health financing mechanism.
As part of renewed efforts at pursuing sustainable
healthcare financing mechanisms that promote UHC,
in 2016, the Anambra state government launched a subnational
social health insurance scheme – Anambra State
Health Insurance Scheme (ASHIS). The goal of the scheme
is to provide access to quality, affordable and efficient health
services for every resident of the State [15,16]. The scheme
which commenced in 2018 is managed by the Anambra
State Health Insurance Agency (ASHIA). The principal
objective of the agency is to promote, regulate, supervise,
implement, and ensure the effective administration of the
scheme [15].
The membership of ASHIS comprises all residents
of Anambra State including employees of the public and
Organized Private Sector (OPS), employees in the informal
sector, and vulnerable persons [15]. The scheme is financed
through premiums (basically payroll taxes and private
contributions), state government subsidies (general and
earmarked taxes), and other sources such as donations,
donor funds, etc. [15]. Actuarists determine the premium
rate be contributed. The ASHIA operational guideline
specifies the contributions as follows: i) Earnings for the
public and OPS employees where an employer pays 10 per
cent of the basic salary while the employee contributes 5 per
cent of the basic salary to cover a principal with the spouse
and four biological children below 21 years. For employees
of the OPS, the employer may decide to pay the entire
contribution for the employees. ii) Equity fund established
for the vulnerable persons. iii) Fixed contributions for
the informal sector. In addition, an enrolee makes a copayment
of only 10 per cent of the cost of medications
prescribed by the Health Care Providers (HCPs) at the
point of care whether as outpatient or inpatient [15,16].
The scheme operates a single pool as stipulated by the law
which established it. The ASHIS covers a basic package
of services including promotion, prevention, curative and
rehabilitative health care services provided at the primary,
secondary and tertiary levels of care at both private and
public health facilities [15,16]. The provider payment
mechanism is through capitation for primary care and
Fee-For-Service (FFS) for secondary and tertiary care.
Capitation is paid in advance for a defined population
for an agreed amount monthly to the HCPs while FFS is
paid by the agency when claims have been submitted and
processed [15,16].
Claims management was done manually at the
commencement of the scheme in 2018. However, ASHIA
introduced an e-claims management system in early 2022
as a more efficient method of claims management following
anecdotal evidence that manual claim management which
it had employed posed several financial, administrative,
and service delivery challenges such as erroneous claims,
inflation of bills, delays in submission, processing, and
reimbursement of claims to HCPs. These challenges
affected the efficiency and overall performance of the
scheme and therefore posed existential threat to her.
There is a dearth of empirical evidence on the
effectiveness of e-claims management for improving
efficiency in healthcare within ASHIS. In addition, study
designs targeted to evaluate the effect of the e-claims
management system could be informed by operational
research to understand whether the e-claims management
system is achieving its desired objectives of improving
health system performance. Such evidence would inform
policymakers, health insurance managers, health insurance
advocates and HCPs not only in Nigeria but other low-andmiddle-
income countries. The study assessed stakeholders’
experiences on the effects of deploying an electronic system
of claims submission, processing, and reimbursement in
the implementation of ASHIS in southeast, Nigeria.
Methods
Study design and area
This was a cross-sectional qualitative method where an
In-Depth Interview (IDI) was used to collect information
on stakeholders’ experiences of switching from a paperbased
system of claims preparation, submission, processing,
and reimbursement to an electronic method and the effects
of e-claims system on the implementation of ASHIS.
The study was conducted in Anambra state, Nigeria.
The projected population of the state in 2022 is six million
persons with an estimated annual growth rate of 2.8 per
cent [17]. Politically, Anambra state is divided into three
senatorial zones: Northern, Central, and Southern. The
State has twenty-one Local Government Areas (LGAs)
for administrative purposes. The State Ministry of Health
(SMOH) coordinates the health system which is organized
into three tiers: primary, secondary, and tertiary levels of
healthcare. Anambra State Health Insurance Agency has
the sole mandate of managing the ASHIS. The provision
of healthcare services under ASHIS is done at both private
and public hospitals across rural and urban areas of the
state [17].
Study population and sampling technique
The study involved two categories of stakeholders
- policymaker’s/health insurance managers and ASHIAaccredited
HCPs who are directly involved in claims
management. Junior officers of the ASHIS who are not
involved in claims management and HCPs whose health
facilities are not accredited to provide services for the
scheme were excluded from this study.
Policymakers and health insurance managers were purposively selected to include those who are directly
involved in claims management and approval. These
respondents include the Chief Executive Officer of
ASHIA; the Technical Assistant to the Governor on Health
Insurance; Heads of the various departments of ASHIA
(Marketing and Business Development, Planning Research
and Statistics (PRS), Administration and Human Resource,
Finance, Internal Audit and Accounts, Information,
Communication and Technology (ICT) and Health
Services Standards and Quality Control) and ASHIA
LGA Desk officers. For the health facilities, a multistage
sampling of ASHIA-accredited HCPs was adopted. First,
the state was stratified into three senatorial zones. Second,
Simple Random Sampling (SRS) method was used to
select two senatorial zones. Third, the SRS method was
used to select a total of four LGAs (two per senatorial zone
comprising one urban and one rural LGA in each of the
two selected senatorial zones) to ensure representation of
geographical locations. In the fourth stage, we purposively
selected ten (10) facilities from an updated list of ASHIAaccredited
health facilities for the selected four LGAs on
the basis of number of enrolees managed (above 500),
facility geographical location (five urban and five rural)
and facility ownership (five public and five private) to
explore diverse experience from the respondents. In the
last stage, the respondents, Health Facility Heads (Medical
Directors or Hospital Administrators), from the selected
health facilities were purposively selected based on their
roles. Tab. 1. summarizes the background information of
the respondents interviewed.
| Category |
Location (n) |
Sex (n) |
Ownership of Facility (n) |
| Policymaker |
Urban (2) |
Male (1)
Female (1) |
- |
| Health Insurance Officer/Manager |
Urban (6) |
Male (7)
Female (4) |
- |
| Rural (2) |
- |
| Health Care Provider |
Urban (5) |
Male (7)
Female (3) |
Public (5) |
| Rural (5) |
Private (5) |
| Total |
20 |
20 |
10 |
|
|
|
|
Tab. 1. Background information of the study respondents.
Data collection
A total of twenty (20) In-Depth Interviews (IDIs)
were conducted with the respondents between May and
June 2022 using a pre-tested, semi-structured IDI guide
developed by the researchers. The IDI guide explored
information on how claims are submitted, processed,
and reimbursed as well as its influence on the effective
implementation of ASHIS. The guide was validated by
two health systems expert researchers to ensure internal
consistency and transferability. Data were collected by ten
experienced researchers who were trained for 3 days. The
researchers worked in pairs (an interviewer and a note-taker).
Interviews were conducted in English and were held in
offices or health facilities as convenient for the respondents.
Each interview lasted an average of 40 minutes and was
audio recorded and transcribed. Notes taken during the
interviews were incorporated into the transcripts to ensure
the completeness and accuracy of information. Prior to the
interviews, both written and verbal informed consents were
obtained from all respondents. Permission to audio-record
interviews and discussions was also obtained from each
respondent.
Data analysis
A thematic framework approach involving coding,
charting, and organising the data under themes was used
to analyse the data. Transcripts were manually coded using
a codebook developed by the researchers. The main themes
were deduced from the study objectives. The themes were
generated by reading the transcripts and reflecting on how
claims are managed and their effect on the implementation
of ASHIS. Inter-coder differences were resolved by
consensus. The main themes explored included: i)
experience with use of the manual and electronic claims
processing systems of claims management and ii) effect or
outcome of the e-claims management system on the health
insurance scheme implementation.
Results
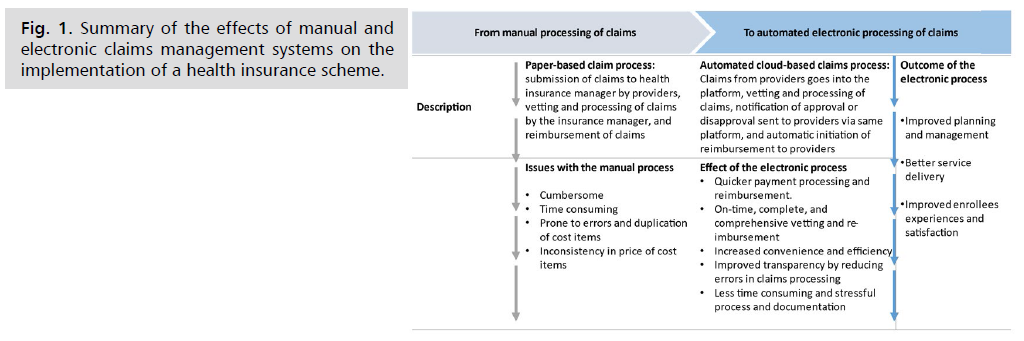
The findings of the study are presented under two headings as described in the data analysis subsection. The summary of the findings is outlined in Fig. 1.
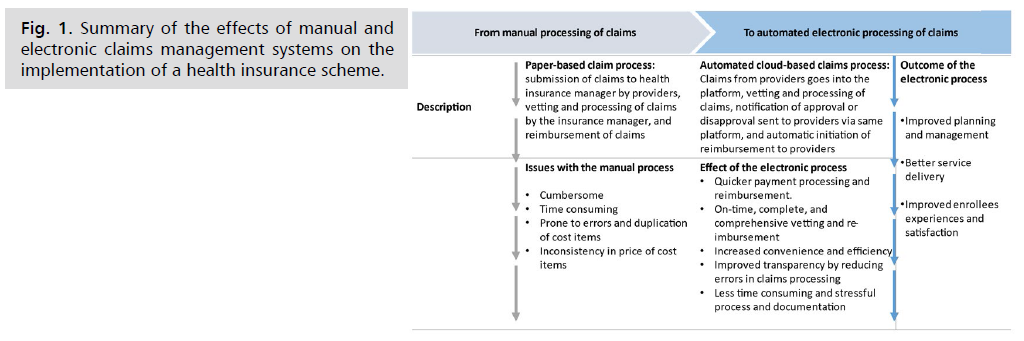
Fig. 1: Summary of the effects of manual and electronic claims management systems on the implementation of a health insurance scheme.
Experience with manual and electronic systems of claim management
Manual system: At the commencement of the scheme, claims were reported to be manually (paper-based) processed and sent directly to ASHIA for reimbursement. The manual processing of claims was stated by the actors (health insurance managers and ASHIA-accredited HCPs) to be cumbersome, time-consuming, and prone to several errors and duplications on claims reports. According to an ASHIA respondent “when we started we were doing fully paper-based, people will go to the hospital they call us to request for pre-authorization codes, we send we approve the services they should render and deny the ones we don't think are appropriate, and at the end of the month, they will send us their claims, the claims management unit will then work on the claims from the HCPs or hospitals, match the claims with the pre-authorization codes that we had sent, and then after vetting the bills, we (ASHIA) pay directly into the accounts of the facilities” (Health Insurance Manager, 01). From the viewpoint of the health provider, manual processing and submission of claims is a burdensome and stressful task. In the words of a provider “we are always to go to Awka (the capital of Anambra state where ASHIA head office is situated) to submit claims, so every time my desk officer collects transport money from me…. it takes time to do so. By the time one travels to Awka and time for working on the claim report, even, the back-and-forth movement during the vetting of our claims. After everything, ASHIA will now call and tell you that the report has errors and they wouldn’t pay this and that” (Health Care Provider, 18).
Electronic system: Respondents reported that the claim management system had been fully digitalized. Claims submission, processing, and reimbursement were stated to be through an automated electronic end-to-end claims management system introduced by the scheme in early 2022. The e-claims management system was said to be designed to allow HCPs who receive a pre-authorization code (for secondary care for a patient) from ASHIA to complete an ‘Individual Claims Form’ (ICF) and then submit the form to the provider portal. At the end of every month, the system consolidates information from all the submitted ICFs and automatically populates the ‘HCP claims form’. The HCP may also upload supporting information for each individual claim such as operation notes, admission reports, laboratory investigation reports etc. These claims (per HCP) are reviewed via a multilevel process supported by an electronic system. After the vetting, claims queries, denial or approval are initiated.
Both health insurance managers and ASHIA-accredited HCPs had a good knowledge on the timing and the electronic process of submitting and reimbursing claims. In the words of a health insurance manager, “we have done away with the paper-based methods, at this point, every claim management in ASHIA is done fully electronically. The hospitals have a portal they log in, make their request, and we (ASHIA) give them approval and it shows on their dashboard there, they treat the patients and send in their bills, the system vets it, and automatically we (ASHIA) can reimburse the claims” (Health Insurance Manager, 05). Similarly, a HCP alluded that “for the past few months, a new portal where you submit your claims was established and we have been using it for a couple of months now and the structure is good. At the first week of every new month when the claims are being submitted electronically, the reimbursements come at the right time actually as agreed, kudos to ASHIA” (Health Care Provider, 11). Another said, “we have laptops we use to process these claims, the Desk officer does this and I will sign on it and vet it and then we send it to them new every month through email and when it is time for reimbursements, they send the money directly to the bank and we receive the bank credit alert. The new system is very good” (Health Care Provider, 14).
Effect of e-claims submission, processing and reimbursement
Study participants shared their experiences in preparing claims, submission, processing, and reimbursement of claims, their influence on health service delivery and implementation of ASHIS at large. All the respondents interviewed reported that transiting from the manual method of claims management to an electronic-based system has made the process easier and better, leading to better service delivery, improved customer experiences and satisfaction, with overall improved efficiency in the system. According to an ASHIA respondent, “the electronic process is working very well. It has helped us to work better and enrollees do not have to suffer for secondary care they want to receive” (Health Insurance Manager, 06). In the affirmative, a HCP alluded that, “when it comes to reimbursement ASHIA pays and they pay as at when due. ASHIA pay the fee-for-service unless you didn’t send your request. This has helped us with treating our enrolees well and they are happy. Yes, money is everything [laughs]” (Health Care Provider, 18).
Specifically, the respondents mentioned the beneficial effects of the e-claim management system, including i) Quicker payment processing and reimbursement. “We (ASHIA) now operate an online system of receiving claims which makes ASHIA attend to them faster” (Health Insurance Manager, 04). Similarly, HCP held the same view that “there is no delay both in payments of claims, they (ASHIA) pay as at when due. In fact, even the capitation, everything is okay. For now, ASHIA is living above the standard” (Health Care Provider, 10). ii) On-time, complete, and comprehensive vetting, and reimbursement. The e-claim management system was reported to have reduced delays in the vetting and reimbursement of claims. From the experience of the health insurance managers, “during the paper-based system, we (ASHIA) were paying within two months and now we pay our fee for service first of every new month since it is fully electronic. All we do is click on the button (on the digital platform) and it'll calculate everything and we pay. So that’s where we are right now, our journey from paper-based to the fully electronic management system, and we have escaped the complaints on time for paying claims to hospitals arising from the manual system” (Health Insurance Manager, 01). iii) Increased convenience and efficiency. Yes, if I should judge between the paperwork and the computer work, I would say that the computer work is easier for us because then I will pack paper home and I will work, work and work and I will do a lot of photocopies and typing so this computer one is better, easier and saves time than that of paperwork and the submission of claims is smoother than the previous system (Health Care Provider, 18). iv) Improved transparency. Respondents stated that the electronic system removed errors and conflict in vetting claims. v) Less time consuming and stressful process and documentation. Ever since we converted the process to an electronic platform there are no conflicts in the system anymore. Unlike before when we have wrong calculations in the price of e.g., drugs and quantities used. Also, bills were not properly done and sent to us, sometimes the prices are inflated, but now with the help of the electronic system, it is way better this cut-off errors. So, there is no need to check if the hospital entered the wrong drug price, the system automatically does it” (Health Insurance Manager, 04)
Although all the respondents agreed that the electronic system of claims management is very efficient and effective. However, few reported that some HCPs still default in the timely submission of their claim to the ASHIA for reimbursement. Their reason for the late submission of their claims includes the unavailability of the responsible staff and poor internet network access. A health insurance respondent reported, “there are hospitals that are still having delays in sending us their claims, some will give you reasons that their desk officers were not on sit or some went on maternity leave, or some went for their annual leave” (Health Insurance Manager, 02). In agreement, a health provider stated, “there are delays but the reason is from the hospitals. Sometimes network disturbs you when you want to input some data into the system and that becomes a problem. Sometimes, our workers may be lazy to do the work you have to make them do it” (Health Care Provider, 13).
Discussion
This study explored stakeholders’ experiences on
switching from the manual to an e-claims management
system and its influence on service delivery and general
implementation of the ASHIS in Nigeria. The study
reveals that the manual system of claims management
was cumbersome and prone to errors resulting in delayed
reimbursement. This could be attributed to the painstaking
nature of processing paper-based claims which require
more labour strength to accomplish. Our findings agree
with previous studies that report manual submission,
processing, and reimbursement of claims to be associated
with delayed claims reimbursement, and discrepancies in
claims vetting which insignificantly impacted health service
delivery negatively [7-9,18]. Perhaps, continuing with the
manual system of preparing claims and submitting claims
with its lapses might eventually encourage HCPs to limit
or compromise the provision of secondary health services
thus affecting quality access to health care services and the
sustainability of ASHIS. It could also lead to HCPs' lack of
trust and confidence in the system. Our assertion is in line
with a study that reported delay in claims reimbursement as
threat to sustainability of a health insurance scheme [8,10].
The use of an e-claims management system benefits
HCPs by reducing delays in reimbursement, minimising
claims rejection and resultant improved service delivery
compared to a paper-based system. The e-claim system
was demonstrated to be efficient due to its ability to detect
or flag errors that cannot be identified by the paper-based
system due to its programming nature. Hence, preventing
human entry errors associated with claims preparation,
submission, and processing, unlike the paper-based
system. This implies that the HCPs and health insurance
managers benefit more from processing claims using the
electronic system than the manual one thereby achieving
more efficiency in healthcare. The implication is that
the “digitalization effects” are achieving their objective
of enhancing efficiency within ASHIS. Our finding is
similar to a study that outlined the benefits of digitalizing
claims management in a health insurance scheme [11,14].
In addition, our findings revealed adequate capacity in
terms of timing and step-wise processes for submitting
and reimbursement of claims using the newly introduce
e-claims system. This suggests that the providers had been
sufficiently educated on the guidelines or procedures for
preparations and submission of claims. Previous studies
have reported long delays in reimbursement of claims to be
due to unclear claims reporting procedures [19,20].
The outlined beneficial effects of implementing
an e-claims management system including faster
process, increased convenience and efficiency, improved
transparency, and reduction of errors/fraudulent claims were
found to lead to build trust and confidence in the system
which ultimately promoted better patient experience and
satisfaction, improved healthcare, and overall performance
of the scheme. This is consistent with a previous study
in reporting that lack of transparency in claims led to
delays in reimbursement of claims, inefficiency, and high
cost of healthcare services [21,22]. More so, large-scale
experimental studies on the digitalization of payments in
other sectors have demonstrated its benefits [23].
However, while this study demonstrates that the
e-claims management system was beneficial to providers
and ASHIA compared with paper claims processing, the
economic implications- costs and benefits of processing
claims manually or electronically to the system is yet
unknown. Hence, further study is needed to evaluate the
Cost-Benefit Analysis (CBA) of e-claims compared with
the paper-claims management system and to establish
whether the marginal benefits of electronic processing of
claims cover its marginal cost (positive net benefits) or
not, thus providing evidence-based information on which
claims processing type provides Value-for-Money (V4forM)
to both providers and the overall health system.
The main strength of this research is the representation
and mix of stakeholders; HCPs of health facilities (public private and urban-rural health facilities) and ASHIS
managers. This allowed for diverse experiences and views
from stakeholders who are directly involved in claims
management and service delivery thereby contributing
to the richness and robustness of the findings. More so,
the study used a probability sampling technique to select
health facilities and participants to share their experiences
on the subject matter which may necessarily represent the
views of the larger population.
The main limitation was that the study used only a
qualitative method to assess the effect of the two claims
processing types among HCPs and ASHIS managers.
Hence, the design did not permit measuring the magnitude
of the effect of the e-claims management system on the
implementation of the scheme.
Conclusion
The study demonstrates the effectiveness of employing
an e-claims management system over a manual system.
The e-claims submission, processing and reimbursement
improved efficiency and led to better service delivery
and performance of ASHIS. It is recommended that the
health insurance agency should make effort to ensure the
sustainability of the electronic claims management system,
with plans for continuous improvement.
Ethics Approval and Consent to Participate
The study obtained an approval from the Health
Research and Ethics Committee of the State Ministry
of Health Awka, Anambra State, Nigeria (Ref. no. MH/
AWK/M/321/408).
Following ethical approval, permission to conduct
data collection was obtained from the management of all
the selected health facilities. This study was conducted
in accordance with the Declaration of Helsinki. All
participants provided both written and verbal informed
consent. Participants were informed of the purpose of the
research, rights of participants and measures that will be
taken to protect them and their data. Hence, participation
was voluntary, and confidentiality was assured. Written
and verbal permission to audio-record interviews was also
obtained from respondents.
Acknowledgment
We thanked the research assistants who assisted in the
data collection. We also appreciate the management of the
health facilities for granting approval for the study.
Consent for Publication
Written informed consent was obtained from
the participants to use quotes from the transcripts in
publication.
Availability of Data and Materials
The data generated and analyzed in this study are not
publicly available due to limitations of ethical approval
involving patient data and anonymity but are available
from the corresponding author on reasonable request.
Competing Interests
The authors declare that there is no competing interest.
Funding
The authors received no financial support for the
research and/or publication of this article.
Authors Contributions
UE and SO conceptualized, designed the study
protocol and data collection instruments. UE analyzed the
data. UE and SO wrote the first draft of the manuscript.
Both authors reviewed and approved the final version for
journal submission.
References
- World Health Organization. Primary health care on the road to universal health coverage: 2019.
- Spaan E, Mathijssen J, Tromp N, et al. The impact of health insurance in Africa and Asia: A systematic review. Bull World Health Organ. 2012;90:685-692.
Google Scholar, Crossref, Indexed at
- Savedoff WD, de Ferranti D, Smith AL, et al. Political and economic aspects of the transition to universal health coverage. Lancet. 2012;380(9845):924-932.
Google Scholar, Crossref, Indexed at
- Lagomarsino G, Garabrant A, Adyas A, et al. Moving towards universal health coverage: Health insurance reforms in nine developing countries in Africa and Asia. Lancet. 2012;380(9845):933-943.
Google Scholar, Crossref, Indexed at
- De Bruin SR, Baan CA, Struijs JN, et al. Pay-for-performance in disease management: A systematic review of the literature. BMC Health Serv Res. 2011;11(1):1-4.
Google Scholar, Crossref, Indexed at
- Awoonor-Williams JK, Tindana P, Dalinjong PA, et al. Does the operations of the National Health Insurance Scheme (NHIS) in Ghana align with the goals of Primary Health Care? Perspectives of key stakeholders in northern Ghana. BMC Int Health Hum Rights. 2016;16(1):1-1.
Google Scholar, Crossref, Indexed at
- Laar AS, Asare M, Dalinjong PA, et al. What alternative and innovative domestic methods of healthcare financing can be explored to fix the current claims reimbursement challenges by the National Health Insurance Scheme of Ghana? Perspectives of health managers. Cost Eff Resour Alloc. 2021;19(1):1-6.
Google Scholar, Crossref, Indexed at
- Alhassan RK, Nketiah-Amponsah E, Arhinful DK, et al. A review of the National Health Insurance Scheme in Ghana: What are the sustainability threats and prospects?. PloS One. 2016;11(11):e0165151.
Google Scholar, Crossref, Indexed at
- Alawode GO and Adewole DA. Assessment of the design and implementation challenges of the National Health Insurance Scheme in Nigeria: A qualitative study among sub-national level actors, healthcare and insurance providers. BMC Public Health. 2021;21(1):1-2.
Google Scholar, Crossref, Indexed at
- Fusheini A, Marnoch G, Gray AM, et al. Implementation challenges of the National Health Insurance Scheme in selected districts in Ghana: Evidence from the field. Int J Public Adm. 2017 16;40(5):416-426.
Google Scholar, Crossref, Indexed at
- Carroll L. More than a third of US healthcare costs go to bureaucracy. Reuters. 2020;6.
- Adzakpah G, Dwomoh D. Impact of digital health technology on health insurance claims rejection rate in Ghana: A quasi-experimental study. BMC Digital Health. 2023;1(1):5.
Google Scholar, Crossref, Indexed at
- Gille F, Smith S, Mays N, et al. Why public trust in health care systems matters and deserves greater research attention. J Health Serv Res Policy. 2015;20(1):62-64.
Google Scholar, Crossref, Indexed at
- World Health Organization. The role of digital claims management for Estonia’s health insurance: A leverage for making healthcare purchasing more strategic. WHO. 2023;10.
- Anambra State Government. Anambra State Health Insurance scheme Law. 2016.
- https://ashia.an.gov.ng/
- Demographic N. Health Survey. National Population Commission (NPC) [Nigeria] and ICF International. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF International. 2013.
- Akweongo P, Chatio ST, Owusu R, et al. How does it affect service delivery under the National Health Insurance Scheme in Ghana? Health providers and insurance managers perspective on submission and reimbursement of claims. PloS One. 2021;16(3):e0247397.
Google Scholar, Crossref, Indexed at
- Wang H, Otoo N, Dsane-Selby L, et al. Ghana National Health Insurance Scheme: Improving financial sustainability based on expenditure review. World Bank Publications; 2017;14.
Google Scholar, Crossref, Indexed at
- Aryeetey GC, Nonvignon J, Amissah C, et al. The effect of the National Health Insurance Scheme (NHIS) on health service delivery in mission facilities in Ghana: A retrospective study. Glob Health. 2016;12:1-9.
Google Scholar, Crossref, Indexed at
- Fenenga CJ, Nketiah-Amponsah E, Ogink A, et al. Social capital and active membership in the Ghana National Health Insurance Scheme-a mixed method study. Int J Equity Health. 2015;14(1):1-2.
Google Scholar, Crossref, Indexed at
- Hu Q, Xu J, Chu Z, et al. Barriers to acceptance of provider-initiated testing and counseling among men who have sex with men in Shenyang, China: A cross-sectional study. Biomed Res Int. 2013;2013.
Google Scholar, Crossref, Indexed at
- Muralidharan K, Niehaus P, Sukhtankar S, et al. General equilibrium effects of (improving) public employment programs: Experimental evidence from India. Econometrica. 2023;91(4):1261-1295.
Google Scholar, Crossref, Indexed at