Keywords
Alveolar macrophages; Cytokines; Microfold cell; Mycobacterium tuberculosis; Phagosome
Abbreviations
Micro fold cells (M-Cells); Tuberculosis (TB); Human Immunodeficiency Virus (HIV); Mycobacterium tuberculosis (M. tuberculosis H37Rv); Phenolic Glycolipids (PGL); World Health Organization (WHO); Fatty Acid Synthase (FAS); Twin-Arginine Translocation (TAT); Receptor activator of nuclear factor- κB ligand (RANKL); Receptor Activator of Nuclear Factor Kappa-B (RANK); Nuclear Factor- Kappa B (NF-Κb); Multiple Drug Resistance-Tuberculosis (MDR-TB); Extensively drug-resistant tuberculosis (XDR-TB); Follicle- Associated Epithelia (FAE); Peyer’s Patches (PP); Mucosa- Associated Lymphoid Tissue (MALT); Nasal Associated Lymphoid Tissue (NALT); Bronchial Associated Lymphoid Tissue (BALT); Fatty Acid Synthase (FAS); Phospholipids (PL); Phenolic Glycolipids (PGL); Tumor Necrosis Factor Receptor Superfamily 11a (TNFRSF11a); Receptor Activator of Nuclear Factor-κB Ligand (RANKL); Receptor Activator of Nuclear Factor-κB (RANK); Type 1 fimbrin Dmannose specific adhesin (FimH).
Introduction
Tuberculosis is the global threat which is widely distributed and communicative [1]. It is caused by Mycobacterium tuberculosis H37Rv (M. tuberculosis H37Rv) strain which is one of the pathogenic strains among Mycobacterium species. Primarily tuberculosis is a respiratory disease, but it also infects other parts of the body including bone, brain, urinary tracts etc. which is known as extra-pulmonary tuberculosis [2]. Besides through respiration, M. tuberculosis H37Rv can also enter in host circulation by Micro fold cells (M-cells). These cells originate within the gut-associated lymphoid tissue (GALT) in Peyer’s patches of the small intestine, and in the mucosa-associated lymphoid tissue (MALT) of additional division of the human gastrointestinal tract [3]. M-cells are famous for instigating mucosal immunity response on the apical membrane of these cells then allocate for conveying of microorganisms and particles throughout the epithelial cell layer through the gut lumen to the lamina propria where communications with immune cells occurs [4]. M-cells are very specialized cells for phagocytosis of intestinal macromolecules, particulate antigens and microorganisms across epithelium. These cells can directly mediate leading infection by M. tuberculosis H37Rv bacterium and ease distribution beyond mucosa [5]. These cells are found in the follicle-associated epithelia (FAE) of Peyer’s patches (PP), isolated lymphoid follicles, NALT (nasal associated lymphoid tissue), BALT (bronchial associated lymphoid tissue), appendix and in MALT outside the gastrointestinal tract. These cells might be deficient in cilia and enzymatic movement, so they are not engaged with processing or ingestion but rather their essential capacity is to translocate particles from gut lumen to host immune cells [6]. Various earlier studies proved that M-cells receptor work very cleverly with host immune cells and inhibit the entry of the pathogen therefore play crucial role in vaccine development or drug delivery [7-9]. In our study, we focused on various characteristics that M-cells shows and its essentiality in manufacturing vaccine against TB.
Literature Review
Tuberculosis epidemics
According to WHO report of 2016, 61 lacs novel cases of tuberculosis were reported by national power system and informed to WHO. The respective data is an increment from the observed data of 2013-2015. 2016-year data shows 6 lac new TB cases which shows resistance to rifampicin (RRTB), which is the major efficient first-line anti tuberculosis medicine, of these 49 lac rifampicin resistance people had been generated multidrug-resistance TB (MDR-TB) and along with this, roughly partially (almost 47%) of these cases were only present in India, China and the Russian countries [10]. According to WHO report of 2017, TB mortality rate has fallen about 3% per year. Occurrence of TB has dropped 2% per year and death due to TB reduced up to 16%; but still there is an immense gap in TB recognition and cure. In 2017 WHO has mentioned TB- Sustainable Development Goals (SDG) monitoring framework of 14 indicators that are associated with TB incidence. In the end TB strategy specific goals are set that include 90% reduction in TB death and 80% reduction in new TB cases per year by 2030, compared with 2015 [11]. TB is a challenge to fitness and analytical tests such as polymerase chain reaction (PCR) and smearing test [12] as these are costly and time-consuming, so we still need a key to control TB. There are some assays that are cheap like TB biomarker assay which is accurate and easily available for TB identification of patient [13]. Now days, Human Immunodeficiency Virus (HIV) and TB drug resistance is a global risk [14,15]. M. tuberculosis H37Rv and Human Immune deficiency Virus (HIV) together weaken the immune system by decreasing CD4+ T lymphocytes and decrease the host survival [16]. People with this co-infection have unfavourable treatment outcome due to executive complexity of these pathogens [17]. Antiretroviral Therapy (ART) is recommended for HIV-TB co-infected patient in early stage of infection because it shows increased HIV-TB co-infected host survival [18]. TB has complicated and longlasting effects on human body that are not common but may be danger to life. In 1.5% to 3.5% cases, Deep Vein Thrombosis (DVT) is associated with TB and critical to isolate TB patients who are at high risk. Anti -Tubercular Treatment (AAT) and anticoagulant therapy can prevent the fatal complication of this disease [19].
M. tuberculosis pathogenesis resistance inside the phagosome
This bacterium is gram positive, aerobic and classified as intracellular parasite of alveolar macrophages of humans. Although this bacterium is classified as gram positive, but it is difficult to stain the bacterium by gram staining procedure due to its complex cell wall nature. Strains of M. tuberculosis H37Rv enters in host through inhalation as these pathogens released by sneezing or coughing of M. tuberculosis H37Rv infected person and ultimately spread to the lungs and utilizes macrophages for its replication, causing primary infection and secondary infection in lymphoid organs. In the alveolar macrophages, this bacterium persists for longer period; enhance its progenies by replication that results in formation of granuloma which is characterized by M. tuberculosis H37Rv cells surrounded by various immune cells like B cells, T cells, NK cells and dendritic cells etc. When M. tuberculosis H37Rv outbreaks in host, it uses its Phenolic Glycolipids (PGL) surface lipid to recruit macrophages through recipient chemokine (C-C motif) ligand 2 (CCL2), which benefit M. tuberculosis H37Rv in inflowing deep in host tissue [20]. M. tuberculosis H37Rv synthesizes Lipomannans (LM) and Lipoarabinomannans (LAM), the two essential cell wall components and necessary for its virulence. M. tuberculosis H37Rv survives by regulating membrane lipid composition in favour to diverse environmental conditions. Many components of lipid rich cell wall are important for causing infection [21,22]. For lipid adjustment Fatty Acid Synthase 1 (FAS 1) and FAS 1 products depending metabolic pathways with membrane Phospholipid (PL) and cargo space compound Triacyl Glycerol (TAG) are essential [23]. In M. tuberculosis H37Rv, biogenesis of FAs is started by the enzyme FAS 1 which is a multifunctional enzyme catalyses de novo pathway and synthesizes long chain acyl CoAs from acetyl CoA via malonyl CoA as extender unit. These acyl-CoAs are consequently used for the production of membrane phospholipids (PL) or they are shambled into the FAS II organization for the production of mycolic acids. In M. tuberculosis H37Rv, the type II FAS organization is dependable for the strengthening of these acyl-CoAs during repetitive compression effect with malonyl-ACP, leading to the formation of long-chain meromycolyl-ACPs [24-26]. M. tuberculosis H37Rv cell wall core is made of peptidoglycan and linear galactofuran which are connected by a link unit L-Rha–D-GlcNAc-P. Peptidoglycan also attached to highly branched arabinofuran and mycolic acid. Mycolic acid is arranged perpendicular to the membrane and responsible for virulent character of M. tuberculosis H37Rv [27]. M. tuberculosis H37Rv hard cell wall could work as permeability barrier which provide resistance against antibiotics and help in diffusion of hydrophilic molecules through liposome [28]. M. tuberculosis H37Rv cell wall alone is unable to show resistance against drug so it requires enzymatic activity, when cell wall is treated with lysozyme, oligomers of weight 20,000 and amino acids, muramic acid, glucosamine are separated [29,30]. M. tuberculosis H37Rv obstructs the biogenesis of the phagolysosome [31]. The inclination of M. tuberculosis H37Rv to enter the host macrophages, where it is securely stowed in a pathogen-accommodating phagosome which does not develop into the phagolysosome [32] is essential to tuberculosis infection, inertness, spread, and concealment of immunological identification by the host.
M. tuberculosis H37Rv dependence on M-cell for infection
Different systems have been proposed to clarify enteral take-up of microorganisms, including interruptions of the epithelial obstruction, transcytosis transversely over enterocytes, infection of dendritic cells or potentially lymphocytes, and via M-cells situated inside the follicle-related epithelium (FAE) which covers Peyer's patches [33], and speckled along the villus-autonomous of Peyer's patches [34]. As mentioned in the introduction part of this manuscript that these cells also help in instigating immune response, also convey a noteworthy position for the testing of gut luminal antigens, as well as are vital for take-up of different commensally residence bacterial and viral pathogens together with Salmonella enteric (S. enteric), Vibrio cholerae (V. cholerae), HIV, Reovirus, Poliovirus etc. [35-38]. M-cells are developed by Receptor activator of nuclear factor-κB ligand and receptor activator of nuclear factor kappa-B (RANKLRANK) pathways [39,40]. If RANKL is absent, then M-cell number has been drastically reduced. The stromal cells below epithelial layer may be source of RANKL [41].
RANKL binds to its receptor, RANK (Tumor Necrosis Factor Receptor Superfamily 11a TNFRSF11a) that activate noncanonical transcription factor RelB and NF-κB related signaling pathway and induces expression of SpiB, an electron transport chain transcription factor which is important for M-Cells providence, determination and maturation [42-44]. M-Cells morphology is different in different animal species. These cells express many different carbohydrate markers on their surface which helps in cells to pathogen or antigen interaction [45]. Mcells allocate substances from gut across epithelium to immune cells and known to transport latex beads, carbon particles, liposome and macromolecules including ferritin, horseradish peroxidase, cholera toxin-binding subunit, lectins and antivirus antibodies [46]. One of the studies shows that these cells are also known for transporting microorganisms from outside the body like V. cholerae and S. typhimurium [47,48]. Distribution through M-cell occurs via transmembrane endocytosis that might be inhibited at 25°C or below and is a fast process in comparison to complete endocytosis and exocytosis that takes at least ten minutes to complete [49,50].
M-cells do not have compactly packed elongated microvilli which are normal characteristics for enterocytes, rather than they have disrupted squat microvilli alongside their apical fringe. Furthermore, these cells contain profound basolateral invaginations that are frequently establish to port different immune cells. This morphology takes into consideration for productive antigen and microbial interaction along fast transcytosis [51-53]. Current revisions in mice model had been confirmed the phenomenon of generation of M-Cells which showed that the origin of these cells is Lgr5+ intestinal stem cells (ISCs) [54]. The separated epithelial lineages of the intestinal system incorporate Paneth cells, cup cells, tuft cells, enterocytes, enteroendocrine cells, and M-cells which specific parts have been requisite for appropriate nourishment inside the setting of a composite advantageous luminal microbiota.
By means of temperament, these ISCs are especially delicate toward damage underneath unpleasant situation such as in infection. In case of such unpleasant environment, stagnant cell populaces of secretory ancestor cells (+4 cells) can dedifferentiate into authentic LGR5+ quickly multiplying ISCs [55]. In both cases homeostatic as well as in adverse conditions, the capacity of stem cells is accepted as affected through different cells inside the position containing subepithelial myofibroblasts, lymphocytes, macrophages, and dendritic cells. Several precise interactive molecules of these cells had been identified such as GP2, Marcks l1, M-Sec, Sgne-1, annexin V and CCL9, of which GP2 mediates bacterial uptake that express Type 1 fimbrin D-mannose specific adhesin (FimH), which is a constituent of type I Pilli on the outer membrane of bacteria and commence consequent definite immune response against bacteria [56-61].
Treatment with Anti - RANKL antibody leads to depletion of M-Cells [62] which efficiently blocks uptake of antigens and prevent development of disease [63]. M-cell specific monoclonal antibodies are established for M-cell targeted mucosal vaccine [64]. It had been demonstrated in many studies that lectin compounds which possess specificities for different carbohydrate molecules can boost uptake of drug in intestine [65-71]. The explicitly of M-Cell for lectins had further recognized through position of horseradish peroxidase (HRP)- conjugated lectins in the transmission electron microscope (TEM). In the glycocalyx of M-cells, carbohydrates are first demonstrated which are not expressed elsewhere on the FAE surface [72]. The phenomenon of targeting the antigen specific M-Cells at immune stimulation site grant a prospective influential approach for civilizing the efficacy of mucosal immunization whereas decreasing probably detrimental sideeffects. Advancement has been made during emergence of such targeting approaches by means of exclusive cell surface assets and the carbohydrate specificity of lectins and these approaches as well confirm valuable effect in treatment of tuberculosis [73].
Microspheres efficiently used for controlled drug delivery and as carrier. Drug delivery through microspheres has several advantages over conventional method. Biodegradable microspheres provide sustain release and eliminate the need of several doses with controlled drug delivery they provide prolonged therapeutic effects; these are reliable and reduce dosing frequency [74,75]. Nanoparticle based drug delivery is advance system and correspond as a marketable, convenient moreover main capable alternate meant for probable TB treatment. Cells intake nanoparticles more efficiently than bigger molecules delivery of drug and are adapted to enable controlled, slow and persistent discharge of drug through the matrix. Nanoparticles comprises of mainly polymers which are biocompatible and biodegradable material, they may be either natural (e.g., gelatin and albumin), synthetic (e.g., polylactides and polyalkylcyanoacrylates), or solid lipids [76].
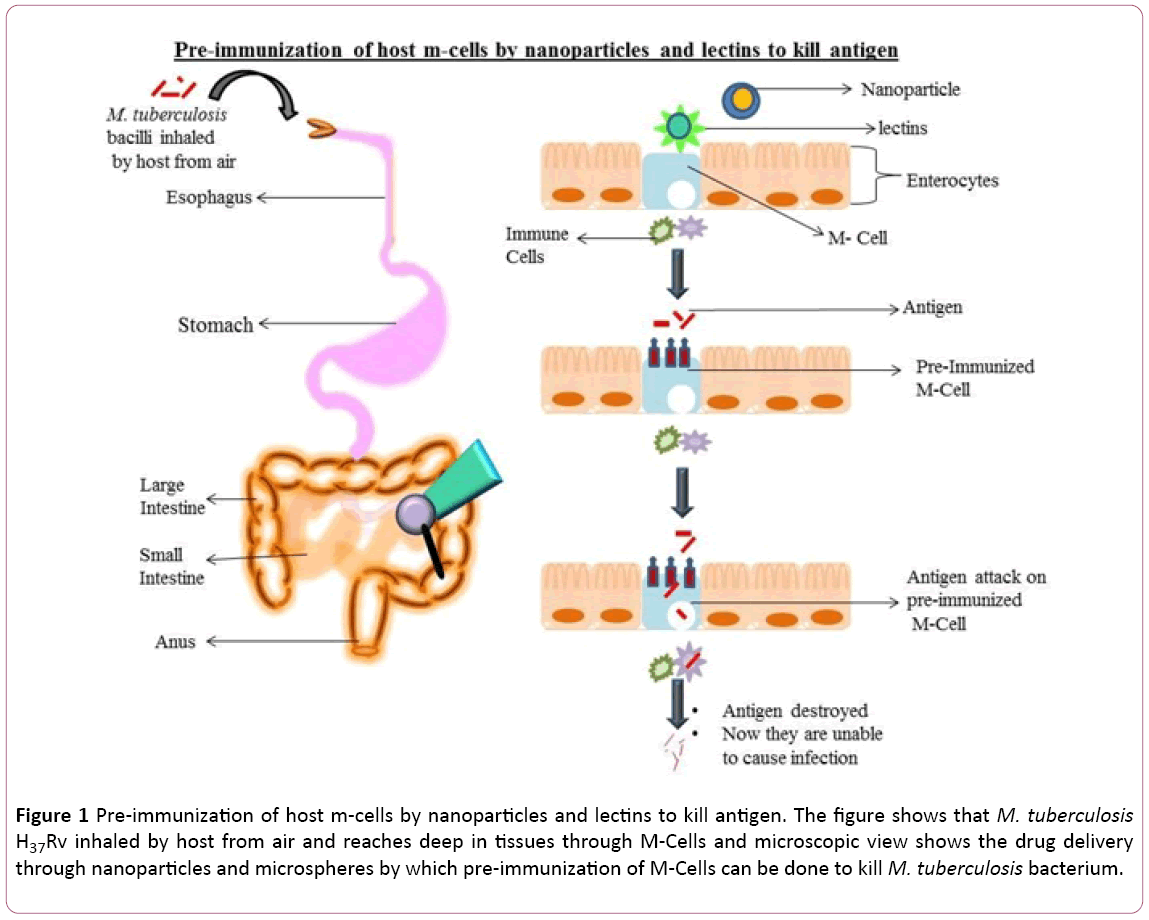
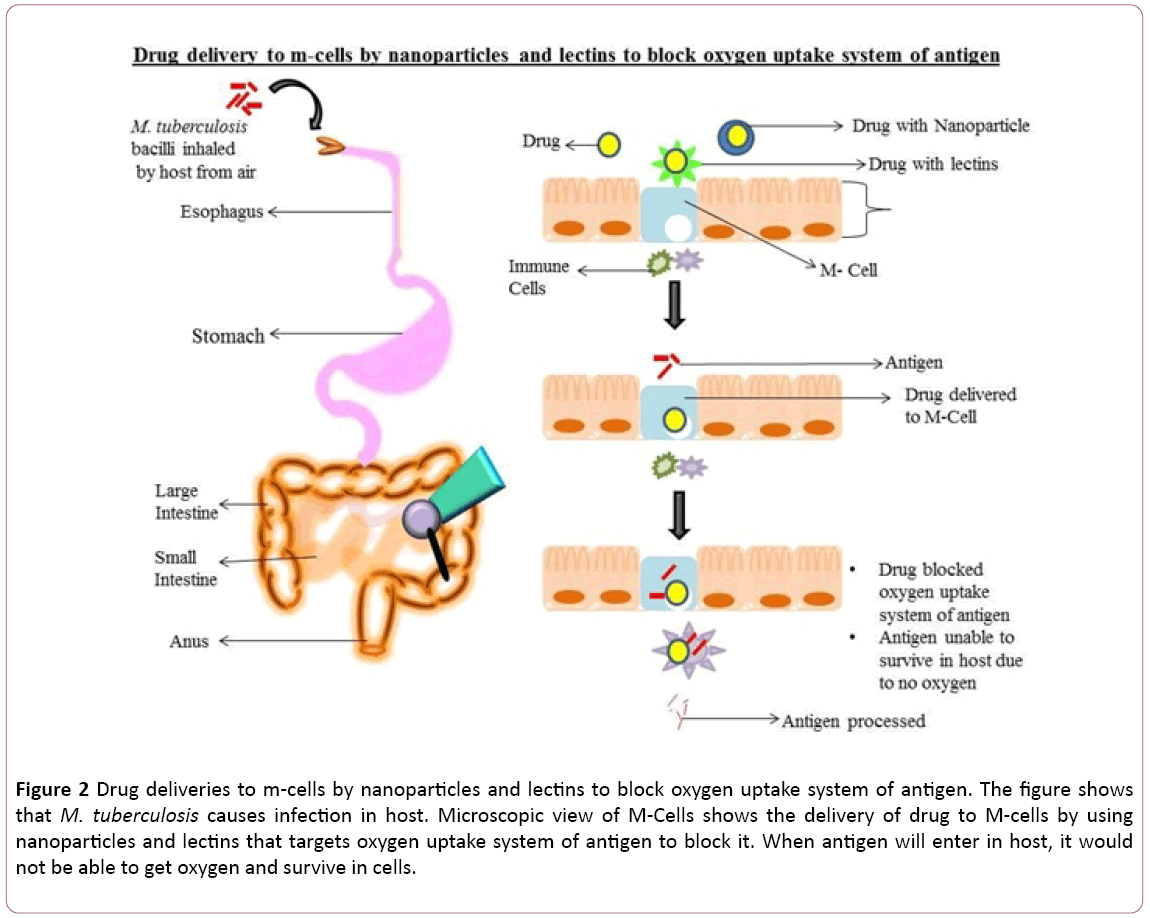
As we know from above lines that microspheres and nanoparticles are successfully used for drug or vaccine delivery so that we can pre-immunize our system by delivering effective antibody or drug in microfold cells which can work against M. tuberculosis H37Rv pathogen (Figure 1). We can also deliver drugs through microfold cell by using lectins or microspheres which can target M. tuberculosis H37Rv system to exterminate it (Figure 2) such as artemisinin which target M. tuberculosis H37Rv system and hinder in oxygen uptake [77].
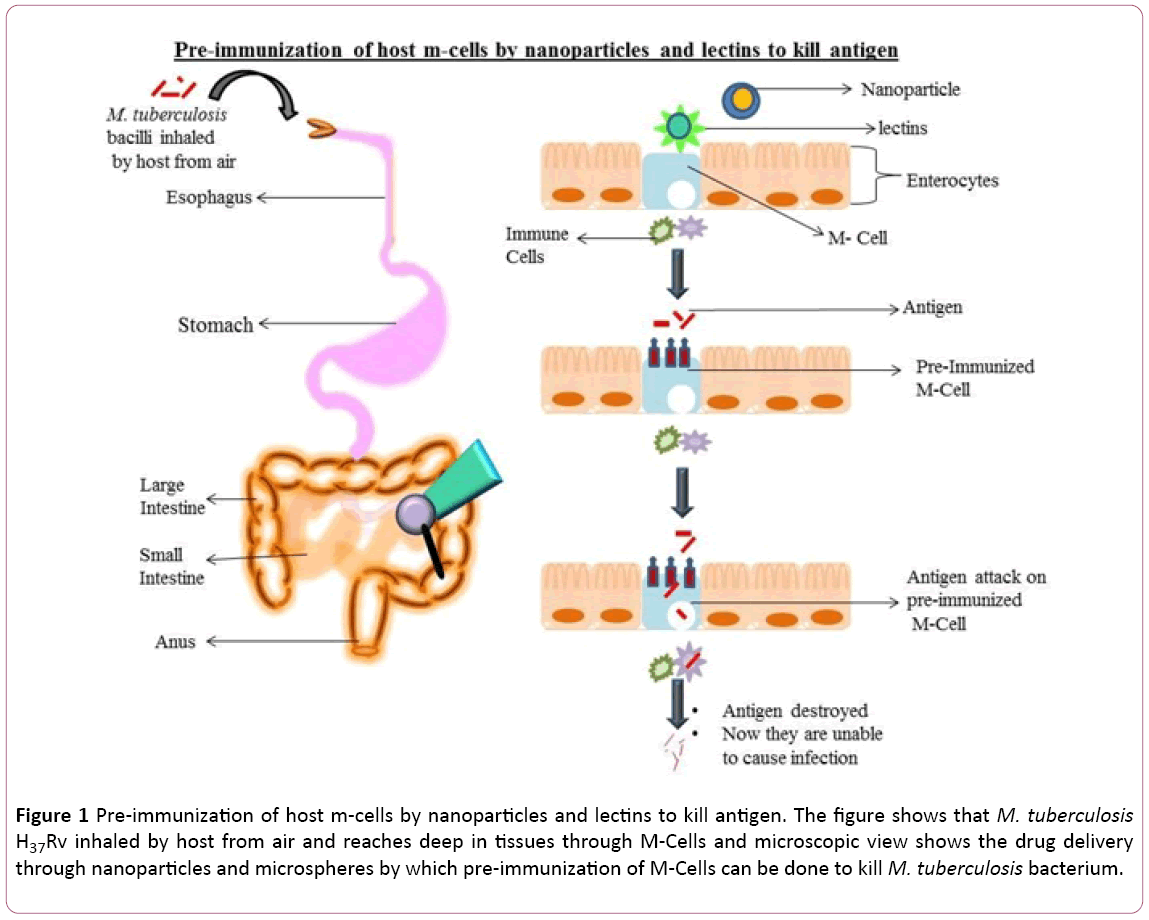
Figure 1: Pre-immunization of host m-cells by nanoparticles and lectins to kill antigen. The figure shows that M. tuberculosis H37Rv inhaled by host from air and reaches deep in tissues through M-Cells and microscopic view shows the drug delivery through nanoparticles and microspheres by which pre-immunization of M-Cells can be done to kill M. tuberculosis bacterium.
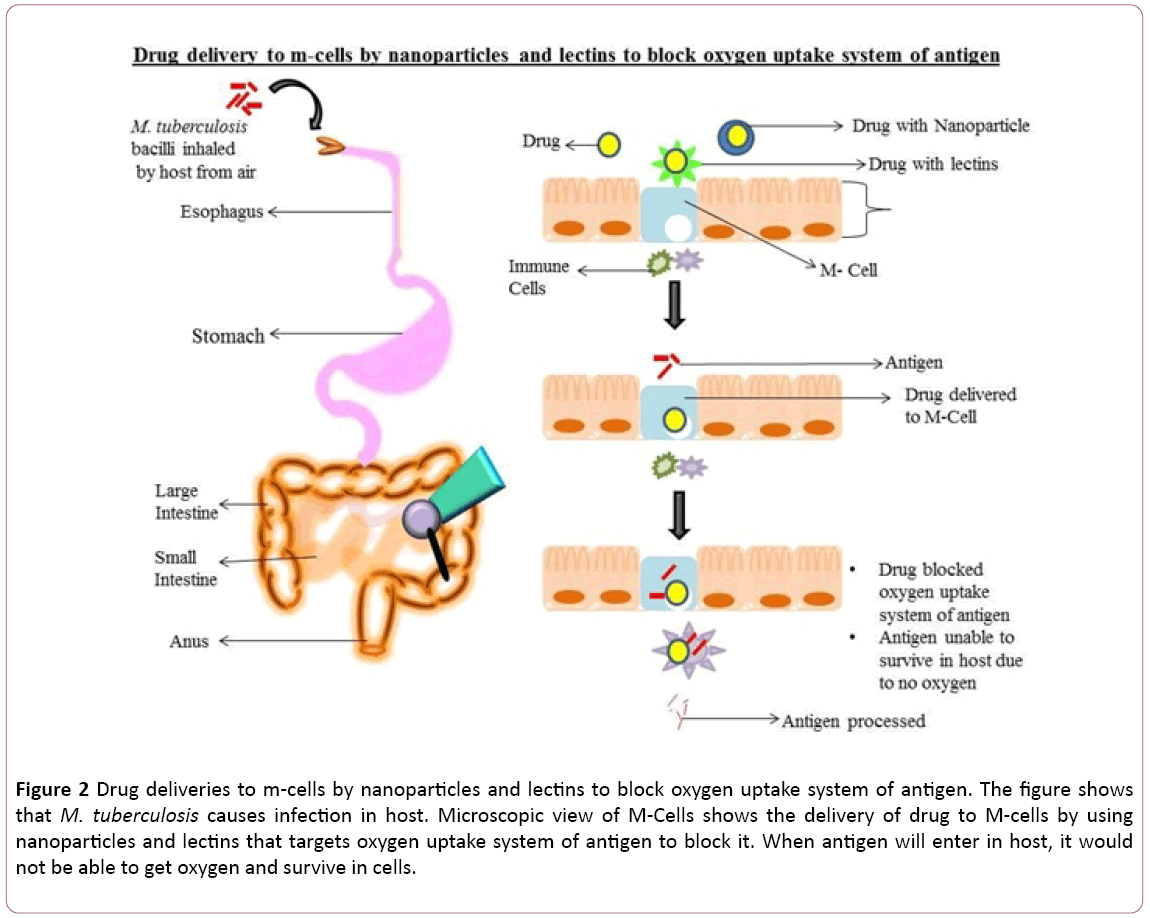
Figure 2: Drug deliveries to m-cells by nanoparticles and lectins to block oxygen uptake system of antigen. The figure shows that M. tuberculosis causes infection in host. Microscopic view of M-Cells shows the delivery of drug to M-cells by using nanoparticles and lectins that targets oxygen uptake system of antigen to block it. When antigen will enter in host, it would not be able to get oxygen and survive in cells.
Discussion and Conclusion
The above content is summarized as, we know that, as TB is a major threat and co-infection of TB with HIV is riskier, therefore we need to discover a novel way to treat this lethal disease. In the above content, we find that M-cells have higher rate of transferring various particles beyond mucosa that provide a different and efficient way of M. tuberculosis H37Rv entry in host and this entrance in most of the people is the primary cause of TB. As M-Cells provide favorable condition like acidic pH for M. tuberculosis H37Rv to survive therefore we can predict that this inhibiting way of transferring of this pathogen from M-Cells can inhibit further infection of M. tuberculosis. M-Cells can be targeted to produce immunity and by using receptors of these cells, pathogen entry can be inhibited either by generating immune response, vaccine or drug delivery. In this way we can predict that such nanoparticle should be synthesized that can recognize the selected M-Cells, carrying specific markers after infection by M. tuberculosis H37Rv. M-Cells represent different carbohydrate receptors that help antigen to get entry so by raising antibodies against these carbohydrate markers may successfully eliminate infected MCell. We can use lectines as they increase drug uptake, nanoparticles as they are efficiently accepted by cells and microspheres as they reduce dosing frequency, to convey drug and vaccine which can pre-immunize our system or can target M. tuberculosis H37Rv system to eliminate it.
Acknowledgments
The authors acknowledge financial support from the Department of Science and Technology-SERB, Council of Scientific and Industrial Research-Institute of Genomics and Integrative Biology under the research project GAP0145.
Conflict of Interest
There is no conflict of interest.
23369
References
- Buczacki SJ, Zecchini HI, Nicholson AM, Russell R, Vermeulen L, et al. (2013) Intestinal label-retaining cells are secretory precursors expressing Lgr5. Nat 495: 65-69.
- Meena LS, Rajni (2010) Survival mechanisms of pathogenic Mycobacterium tuberculosis H37Rv. FEBS J 277: 2416-2427.
- McDonough KA, Kress Y, Bloom BR (1993) Pathogenesis of tuberculosis: Interaction of Mycobacterium tuberculosis with macrophages. Infect Immun 61: 2763-2773.
- Gebert A, Pabst R (1999) M cells at locations outside the gut. Semin Immunol 11: 165-170.
- Nair VR, Franco LH, Zacharia VM, Khan HS, Stamm CE, et al. (2016) Microfold cells actively translocate Mycobacterium tuberculosis to initiate infection. Cell Rep 16: 1253-1258.
- Cor SC, Hill C (2007) M-cells: Origin, morphology and role in mucosal immunity and microbial pathogenesis. FEMS Immunol Med Microbiol 52: 2-12.
- Wang M, Gao Z, Zhang Z, Pan L, Zhang Y (2014) Roles of M cells in infection and mucosal vaccines. Hum Vaccin Immunother 10: 3544-3551.
- Frey A, Neutra MR (1997) Targeting of mucosal vaccines to Peyer's patch Mcells. Behring Inst Mitt 98: 376-389.
- Kim SH, Kim J, Lee KY, Jang YS (2010) The M cell-targeting ligand promotes antigen delivery and induces antigen-specific immune responses in mucosal vaccination. J Immunol 185: 5787-5795.
- Meena LS, Rajni (2016) Biochemical characterization of PE_PGRS61 family protein of Mycobacterium tuberculosis H37Rv reveals the binding ability to fibronectin. IJBMS pp: 1105-1113.
- Yerlikaya S, Broger T, MacLean E, Pai M, Denkinger CM (2017) A tuberculosis biomarker database : The key to novel TB diagnostics. Int J Infect Dis 56: 253-257.
- Duarte TA, Nery JS, Boechat, N, Pereira SM, Simonsen V, et al. (2017) A systematic review of east african-indian family of Mycobacterium tuberculosis in brazil. Braz J Infect Dis 21: 317-324.
- Alizadeh AM, Marjani M, Moniri A, Baghaei P, Jabbehdari S, et al. (2016) Tuberculosis in solid organ transplantation. Tanaffos 15: 124-127.
- Lawn SD (2004) AIDS in africa: The impact of coinfections on the pathogenesis of HIV-1 infection. J Infect 48: 1-12.
- Cunha R, Maruza M, Montarroyos UR, Coimbra I, Miranda-Filho D, et al. (2017) Survival of people living with HIV who defaulted from tuberculosis treatment in a cohort, Recife, Brazil. BMC Infect Dis 17: 137.
- Nagua TJ, Aboud S, Mwirud R, Matee IM, Rao M, et al. (2016) Tuberculosis associated mortality in a prospective cohort in Sub Saharan Africa: Association with HIV and antiretroviral therapy. Int J Infect Dis 56: 39-44.
- Rajni, Meena LS (2010) Guanosine triphosphatases as novel therapeutic targets in tuberculosis. Inter J Infect Dis 14: 682-687.
- Cambier CJ, Falkow S, Ramakrishnan L (2014) Host evasion and exploitation schemes of Mycobacterium tuberculosis. Cell 159: 1497-1509.
- Cashmore TJ, Klatt, S, Yamaryo-Botte Y, Brammananth R, Rainczuk AK, et al. (2017) Identification of a membrane protein required for lipomannan maturation and lipoarabinomannan synthesis in Corynebacterineae. J Biol Chem 292: 4976-4986.
- Bacon J, Marsh PD (2007) Transcriptional responses of Mycobacterium tuberculosis exposed to adverse conditions in vitro. Curr Mol Med 7: 277-286.
- Cabruja M, Mondino S, Tsai YT, Lara J, Gramajo H, et al. (2017) A conditional mutant of the fatty acid synthase unveils unexpected cross talks in mycobacterial lipid metabolism. Open Biol 7: 160277.
- Schaeffer ML, Agnihotri G, Volker C, Kallender H, Brennan PJ, et al. (2001) Purification and biochemical characterization of the Mycobacterium tuberculosis beta-ketoacyl-acyl carrier protein synthases KasA and KasB. J Biol Chem 47: 29-47.
- Kremer L, Guérardel Y, Gurcha SS, Locht C, Besra GS (2002) Temperature-induced changes in the cell-wall components of Mycobacterium thermoresistibile. Microbiol 148: 3145-3154.
- Jackson M, McNeil MR, Brennan PJ (2013) Progress in targeting cell envelope biogenesis in Mycobacterium tuberculosis. Future Microbiol 8: 855–875.
- Brennan PJ (2003) Structure, function, and biogenesis of the cell wall of Mycobacterium tuberculosis. Tubercul 83: 91-97.
- Trias J, Jarlier V, Benz R (1992) Porins in the cell wall of mycobacteria. Science 258: 1479-1481.
- Jarher V, Nlkaldo H (1994) Mycobacterial cell wall: Structure and role in natural resistance to antibiotics. FEMS Microbiol Lett 123: 11-18.
- Adam A, Ciorbaru R, Petit JF, Lederer E (1972) Isolation and properties of a macromolecular, water-soluble, immuno-adjuvant fraction from the cell wall of Mycobacterium smegmatis. Proc Nat Acad Sci 69: 851-854.
- Russell P (2002) Characterization of mutations in NOT2 indicates that it plays an important role in maintaining the integrity of the CCR4-NOT complex. J Mol Biol 322: 27-39.
- Armstrong JA, Arcy Hart PD (1971) Response of cultured macrophages to Mycobacterium tuberculosis, with observations on fusion of lysosomes with phagosomes. J Exp Med 134: 713-740.
- Mabbott NA, Donaldson DS, Ohno H, Williams IR, Mahajan A (2013) Microfold (M) cells: Important immunosurveillance posts in the intestinal epithelium. Mucosal Immunol 6: 666–677.
- Clark AM, Hirst BH (2002) Expression of junction-associated proteins differentiates mouse intestinal M cells from enterocytes. Histochem Cell Biol 118: 137-147.
- Amerongen HM, Weltzin R, Farnet CM, Michetti P, Haseltine WA, et al. (1999) Transepithelial transport of HIV-1 by intestinal M cells: A mechanism for transmission of AIDS. J Acq Immu Def syn 4: 760-765.
- Neutra M, Frey A, Kraehenbuhl J (1996) Epithelial M cells: Gateways for mucosal infection and immunization. Cell 86: 345-348.
- Gonzalez-Hernandez MB, Liu T, Payne HC, Stencel-Baerenwald JE, Ikizler M, et al. (2014) Efficient norovirus and reovirus replication in the mouse intestine requires microfold (M) cells. J virology 88: 6934-6943.
- Amerongen HM, Weltzin R, Mack JA, Winner LS, Michetti P, et al. (1992) M cell-mediated antigen transport and monoclonal IgA antibodies for mucosal immune protection. Ann New York Acad Sci 664: 18-26.
- Knoop KA, Kumar N, Butler BR, Sakthivel SK, Taylor RT, et al. (2009) RANKL is necessary and suf?cient to initiate development of antigen-sampling M cells in the intestinal epithelium. J Immunol 183: 5738–47.
- Wood MB, Rios D, Williams IR (2016) TNF-αaugments RANKL-dependent intestinal M cell differentiation in entered cultures. Am J Physiol Cell Physiol 311: 498-507.
- Kurashima Y, Kiyono H (2016) Mucosal ecological network of epithelium and immune cells for gut homeostasis and tissue healing. Annu Rev Immunol 35: 119-147.
- Kanaya T, Hase K, Takahashi D, Fukud AS, Hoshino K, et al. (2012) The Ets transcription factor Spi B is essential for the differentiation of intestinal microfold cells. Nat Immunol 13: 729-736.
- Rouch JD, Scott A, Lei NY, Martín MG (2013) The functional maturation of M cells is dramatically reduced in the Peyer’s patches of aged mice. SMI 6: 1027-1037.
- Tahoun A, Mahajan S, Paxton E, Malterer G, Donaldson DS, et al. (2012) Salmonella transforms follicle-associated epithelial cells into M cells to promote intestinal invasion. Cell Host Microbe 12: 645-656.
- Miller H, Zhang J, Lee RK, Patel GB, Chen W (2007) Intestinal M cells: The fallible sentinels. World J Gastroenterol 13: 1477-1486.
- Gebert A, Rothkotter HJ, Pabst R (1996) M cells in Peyer’s patches of the intestine. Int Rev Cytol 167: 91-159.
- Kerneis S, Bogdonova A, Kraehenbuhl JP, Pringault E (1997) Conversion by Peyer’s patch lymphocytes of human enterocytes into M-cells that transport bacteria. Sci 277: 949-952.
- Jensen VB, Harty JT, Jones BD (1998) Interaction of the invasive pathogens Salmonella typhimurium, Listeria monocytogenes, and Shigella ?exneri with M-cells and murine Peyer’s patches. Infect Immun 66: 3758-3766.
- DesRieux A, Ragnarsson EG, Gulberg E, Preat V, Schneider YJ, et al. (2005) Transport of nanoparticles across an in vitro model of the human intestinal follicle associated epithelium. Eur J Pharm Sci 25: 455-465.
- Kraehenbuhl JP, Neutra MR (1992) Molecular and cellular basis of immune protection of mucosal surfaces. Physiol Rev 72: 853-879.
- Fotopoulos G, Harari A, Michetti P, Trono D, Pantaleo G, et al. (2002) Transepithelial transport of HIV-1 by M cells is receptor-mediated. Proc Natl Acad Sci USA. 99: 9410-9414.
- Fantini J, Yahi N, Chermann JC (1991) Human immunodeficiency virus can infect the apical and basolateral surfaces of human colonic epithelial cells. Proc Natl Acad Sci USA 88: 9297-9301.
- Kerneis S (1997) Conversion by Peyer’s patch lymphocytes of human enterocytes into M cells that transport bacteria. Sci 277: 949-952.
- Rouch JD, Scott A, Lei NY, Vargas RSS, Wang J, et al. (2016) Development of functional microfold (M) cells from intestinal stem cells in primary human enteroids. Am J Physiol Cell Physiol 311: 498-507.
- Sato T, Vries RG, Snippert HJ, Van De, Wetering M (2009) Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nat 459: 262-265.
- Hase K, Kawano K, Ohno H (2009) Uptake through glycoprotein 2 of FimH+ bacteria by M cells initiates’ mucosal immune response. Nat 462: 226-230.
- Terahara K, Yoshida M, Igarashi O, Nochi T, Pontes GS, et al. (2008) Comprehensive gene expression profiling of Peyer’s patch M cells, villous M-like cells, and intestinal epithelial cells. J Immunol 180: 7840-7846.
- Hase K, Ohshima S, Kawano K, Hashimoto N, Ohno H (2005) Distinct gene expression profiles characterize cellular phenotypes of follicle-associated epithelium and M cells. DNA Res 12: 127-137.
- Verbrugghe P, Waelput W, Dieriks B, Waeytens A, Vandesompele J, et al. (2006) Murine M cells express annexin V specifically. J Pathol 209: 240-249.
- Hase K, Murakami T, Takatsu H, Ohno H (2006) The membrane-bound chemokine CXCL16 expressed on follicle associated epithelium and M cells mediate lympho-epithelial interaction in GALT. J Immunol 176: 43-51.
- Hase K, Kimura S, Takatsu H, Ohmae M, Kawano S et al. (2009) M-Sec promotes membrane nanotube formation by interacting with Ral and the exocyst complex. Nat Cell Biol 11: 1427-1432.
- Cunningham AL, Guentzel MN, Yu JJ, Arulanandam BP (2016) M-Cells Contribute to the entry of an oral vaccine but are not essential for the subsequent induction of protective immunity against Francisella tularensis. PLoS One 11: 153-402.
- Donaldson DS, Kobayashi A, Ohno H, Yagita H, Williams IR, et al. (2012) M cell-depletion blocks oral prion disease pathogenesis. Mucosal Immunol 5: 216-25.
- Nochi T, Yuki Y, Matsumura A, Mejima M, Terahara K, et al. (2007) A novel M cell–specific carbohydrate targeted mucosal vaccine effectively induces antigen-specifi c immune responses. J Exp Med 204: 2789-2796.
- Clark MA, Hirst BH, Jepson MA (2000) Lectin-mediated mucosal delivery of drugs and microparticles. Adv Drug Deliv Rev 43: 207-223.
- Ertl B, Heigl F, Wirth M, Gabor F (2000) Lectin-mediated bioadhesion: Preparation, stability and Caco-2 binding of wheat germ agglutinin-functionalized poly (DL-lactic-co-glycolic acid)-microspheres. J Drug Targeting 8: 173-184.
- Wirth M, Fuchs A, Wolf M, Ertl B, Gabor F (1998) Lectin mediated drug targeting: Preparation, binding characteristics, and antiproliferative activity of wheat germ agglutinin conjugated doxorubicin on Caco-2 cells. Pharm Res 15: 1031-1037.
- Russell-Jones GJ, Veitch H, Arthur L (1999) Lectin-mediated transport of nanoparticles across Caco-2 and OK cells. Int J Pharm 190: 165-174.
- Lehr CM, Bouwstr JA, Kok W, Noach AB, Boer AG, et al. (1992) Bioadhesion by means of specific binding of tomato lectin. Pharm Res 9: 547-553.
- Hussain N, Jani PU, Florence AT (1997) Enhanced oral uptake of tomato lectin-conjugated nanoparticles in the rat. Pharm Res 14: 613-618.
- Carreno-Gomez B, Woodley JF, Florence AT (1999) Studies on the uptake of tomato lectin nanoparticles in everted gut sacs. Int J Pharm 183: 7-11.
- Clark MA, Jepson MA, Simmons NL, Booth TA, Hirst BH (1993) Differential expression of lectin-binding sites defines mouse intestinal M-cells. J Histochem Cytochem 41: 1679-1687.
- Jepsona MA, Clarkb MA, Hirstb BH (2004) M cell targeting by lectins: a strategy for mucosal vaccination and drug delivery. Adv Drug Deliv Rev 56: 511-525.
- Meena LS, Ansari R (2016) Microvesicles: Transporter of proteins in Mycobacterium tuberculosis pathogenesis. J Mol Bio Biotech 1: 2.
- Kaur D, Saini S, Singh G, Rana AC (2012) Biodegradable Microspheres. IRJP 3: 12.
- Wissing SA, Kayser O, Muller RH (2004) Solid lipid nanoparticles for parenteral drug delivery. Adv Drug Deliv Rev 56: 1257-1272.
- Ntutela S, Smith P, Matika L, Mukinda J, Arendse H, et al. (2009) Efficacy of Artemisia afra phytotherapy in experimental tuberculosis. Tuberculosis 89: 33-40.