Keywords
Cardiac anesthesia; Cardiac surgery; BIS; Fast-track extubation; Hospital length of stay
Introduction
The unintended awareness historically has higher incidence rate among cardiac surgeries anesthesia, when compared with other anesthetic subspecialties. But in the modern practice the incidence rate is less certain, but still there is no clear incidence rate among the cardiothoracic anesthesia, due to lack of adequate number of studies which address this issue.
The unintended awareness in cardiac surgery has wide range of incidence, ranges from less than 1% to 23%, and that depending on the size of the study, method of detection and definition of awareness. So at this high incidence rate of unintended awareness during cardiac anesthesia, The national institute of Health and Care Excellence (NICE) has suggested the use of monitoring device, to maintain adequate depth of anesthesia, specially the Bispectral index (BIS).
Bispectral index is defined as first quantitative electroencephalograph (EEG) index used in clinical practice as monitor to assess the depth of anesthesia and hypnosis of anesthesia component, physically it consist of sensor, a digital signal converter, and monitor.
The Bispectral index (BIS) is a measure of the effects of anesthesia and sedation on the brain, a new vital sign that allows clinicians to deliver anesthesia with more precision and to assess and respond more appropriately to patients changing condition during surgery. As such, it is an important advanced in the field of anesthesiology driven by the desire to improve patient care and recovery from surgery and anesthesia [1-5].
Bispectral index (BIS) index has been proven to be accurate and reliable in nearly all patients and clinical setting, and is robust in the presence of the most commonly used anesthetic and sedative agents. It could have direct or indirect effects on recovery. Initial efficacy studies have demonstrated that BIS monitoring can reduce anesthetic drugs use and the time of extubation in non cardiac surgery patients. Which means, consciousness recovers faster by using less anesthetic drugs? However BIS could have indirect effects on patient’s recovery across different surgical population. Such effects could be mediated through cognitive phenotypes which might play an important role in determining extubation in the ICU setting. If the intraoperative use of BIS monitor affects intermediate cognitive phenotypes such as post operative delirium, it could alter the time of extubation in the post operative period in the ICU [5-7].
The anesthesia advancement made a revolution in cardiac surgery and improved utilization of cardiopulmonary bypass, and improved post operative management. As this surgery continue to improve, ways to improve patient outcomes and length of stay remain high priorities, however in the past decade, while the number of cardiac surgery case has increased, there has been little reduction in the patients days of stay (https://www.sts.org/ sites/default/files/documents/pdf/ndb2010/3rdHarvestExecutiv eSummary2010.pdf, 2011).
In a Cochrane review (Hawkes, Dhileepan, and Foxcroft 2003) it investigated if early extubation in cardiac surgery patients could reduce not only the length of stay, but also patient’s mortality rate. It was found that there were no positive or negative effects on mortality rate with early extubation. But there was a reduction in intensive care unit and hospital length of stay, the study suggested farther investigation to establish the safety and efficacy of early extubation in these patients.
A sub group of the society of thoracic surgeon was formed to improve surgical outcomes in patients undergoing chest surgery. https://www.sts.org/sites/default/files/documents/pdf/ guidelines/BloodConservationUpdate0311.pdf
The Virginia Cardiac surgery quality identified fast - track anesthesia and early extubation as one possible way to improve outcomes in its edition [8-15].
Fast – track cardiac anesthesia, although variably defined, generally aims at tracheal extubation within 8 hours postoperatively. As fast-track tracheal extubation after cardiac surgery has become a common practice, methods believed to facilitate this must be validated. This includes the use of intraoperative monitoring modalities, such as candidate depth of anesthesia monitors (BIS).
Purpose of the Study
There are many cardiac anesthesia technique modalities nowadays, but many clinicians in Palestinian hospitals still in dilemma about the most efficient method to use, the BIS monitor is not available in most of cardiac surgery units in Palestine, except in An-najah National University Hospital. So I found it’s helpful and useful to investigate the role of using BIS monitoring among cardiac anesthesia patients, and its effect on postoperative extubation time, and patients discharge time, and to make evidence base practice for the correct role of BIS monitoring among cardiac anesthesia patient in our hospital [16-20].
one of the measurements to improve the quality of health care in the hospitals is by decreasing the time of extubation and avoiding the unintended awareness, there is a reliable method to use, which is BIS monitoring intra-operatively, to minimize the unintended awareness and to make optimal hemodynamic status to promote the ideal emergence, and extubation condition and to examine its effect on patients length of stay in the hospital.
Aims and Objectives
The main aim of the study is to make clinical methods, and clinical guidelines to improve the quality of care which is provided for cardiac surgery patients, who undergo general anesthesia and to improve the post operative health care, and to increase satisfaction of these patients in An-najah National University Hospital.
Methods
After obtaining IRB approval and informed written consent, we studied a total number of 100 patient’s schedules for cardiopulmonary bypass in An-najah National University Hospital (ANUH)/ Nablus /Palestine. ANUH was selected due to high flow of cardiac surgery patients, and due to availability of high quality technologies like BIS monitoring device which is not available in any other hospital in the country and because An-najah National University Hospital is a central high advanced hospital that covers all the regions of Palestine, so the number of patients is higher than any other hospitals in Palestine.
100 patients between the age of 30 and 75 years undergoing elective cardiopulmonary bypass surgery and patients undergoing elective valve replacement or repair from 01/10/2015 to 01/04/2016 were assigned for this study [21-28].
Pre-operatively all patients received pre-operative sedation with midazolam 5 mg, induction of anesthesia was performed with the use of propofol (2 mg/kg), Rocuronium (1 mg/kg), fentanyl (20 mcg/kg) for both groups.
Anesthesia maintenance was balanced by the use of isoflurane Mac (0.6 to 1.5) and fentanyl 20 mcg/kg, and propofol infusion (50 to100 mcg/kg/min). In the conventional group the maintenance (propofol) was titrated to keep the MBP (60-65 mmHg), While the BIS group the propofol was titrated to maintain BIS reading between 40 to 50.
Exclusion criteria
1) Patients with ejection fraction less than 40%.
2) Patients with LV aneurysm.
3) Patients requiring pre-operative intra-aortic balloon pump.
4) Patients with hepatic or renal impairment.
5) Patients with cerebrovascular accident.
6) Patients with excessive alcohol intake.
7) Patients with COPD.
The study was approved by the institutional Ethics committee and written informed consent was obtained from each patient.
Patients were allocated to two groups. Randomization was done by using block randomization technique.
Group B: BIS guided anesthesia group.
Group C: Conventional anesthesia group.
Eligible patients for the surgery who admitted to the cardiac care unit in the An-najah National University Hospital were approached for the study participation immediately after the routine preanesthetic evaluation. Patients who agreed participation in the study singed a written informed consent [29-32].
at the time of surgery, patients was randomized to one of two groups, using block randomization technique, each block contains four participants, moreover the group will be stratified into age group less than 40 years, 40-59 years, 60-69 years, and over 70 years. This stratification will eliminate the age and sex bias.
Each stratum will have similar distribution between treatment group and control group.
The BIS guided group will be monitored by BIS monitoring by applying the BIS electrodes on the patient forehead as manufacturing procedure instruction after preparing the skin of the patient by cleaning the forehead with alcohol wipe to provide good electrical contact, while the other group will receive cardiac anesthesia as usual practice without BIS monitor. The BIS monitor and depth of anesthesia will be monitored continuously and, reading will be recorded as scheduled every 10 minutes, and to record any reading above 60 or less than 40, to investigate for unintended awareness, as a BIS value between 40 and 60 indicates an appropriate level for general anesthesia.
Study protocol
In the BIS group we recommended that volatile anesthetic agents be titrated to maintain a BIS value of 40 to 60, where in the conventional group, we recommended that volatile anesthetic be titrated within 0.7 to 1.3 ages -adjusted minimum alveolar concentration (MAC). Age adjusted MAC was calculated using published age corrected MAC chart. Participants were free to titrate outside of the range according to clinical discretion.
The fast-track approach used in this study involves usual dose narcotics, and age adjusted MAC volatile anesthetic technique. Propofol was given for induction of anesthesia unless contraindicated. Anesthesia was maintained using Fentanyl and isoflurane. Midozolam was given at the discretion of the attending anesthesiologist, and rocuronium was used for muscle relaxation (Table 1) following up the patients after surgery for both groups was started from the time of completion of surgery till the discharge of the patients, once the surgery finished and adhesive dressing applied on surgical site, the time for extubation was determined from that moment till the endotracheal tube was extubated. The time was measured by hours, minutes, and seconds. The follow up was continued if the extubation was performed in the cardiac care unit.
| An-najah National University Hospital Tracheal Extubation Criteria |
| Respiratory |
Ph 7.3-7.5
Carbon dioxide partial pressure (pco2) 30-50 mmHg.
Fraction of inspired oxygen ( Fio2) = 0.5
Minute ventilation < 10 L/min
Few respiratory secretions |
| Hemodynamic |
Heart rate 50-110 bpm ( may be paced)
Mean arterial blood pressure 60-110 mmHg ( may be on stable dose of inotropes/ vasopressor).
Chest tube losses < 100 ml/h
Hemoglobin > 70 g/L |
| General |
Temp > 35.5°C.
Pain control adequate.
Able to left head off pillow for 5s
Conscious and responding to commands |
| Special concerns |
Was the patient difficult to intubate? (yes/no)
Patient currently has significant facial or oropharyngeal edema? (Yes or no).
Patient has no leak with the cuff deflated? (Yes or no). A physician must be present for the tracheal extubation with a yes answer in this column. |
Table 1: Extubation criteria.
The patients discharge time was also measured by days and hours.
Data analysis.
Anesthesia maintenance phase, defined as 10 minutes after anesthesia induction until 20 minutes before the end of surgery, was isolated to allow calculation of median age-adjusted MAC values during this maintenance phase. Data reduction was performed using Matlab engineering software, and data analysis was done by using SPSS statistical software version 21.
To ensure adequacy of the convenience sample size, an a priori power analysis was performed for a univariate Mann-Whitney U test to compare the time of extubation in the BIS group and conventional group.
30 minutes difference in time of extubation was considered to be the smallest clinically significant intergroup difference. Assuming a difference of 30 minutes between the mean times to tracheal extubation (Cohen d = 0.75), an α of 0.05, and β of 0.05 (power = 0.95), 50 patients per group would be needed to show a significant difference between the BIS and conventional groups.
The data analysis plan will be summarized using descriptive summary measures: expressed as mean (SD) for continuous variables and percentage for categorical variables. The significance level will be considered in this study is less than 0.05 by using T-test and chi square for any predicted correlation between dispended and independent variable. The primary predicted correlation will be measured by:
• T- Test will be used to compare the mean extubation time between two groups.
• T-Test will be used to compare the mean of patient hospital length of stay between the two groups.
Variables Definition
Dependent variable
• The time of extubation post CABG or value replacement as continuous variable.
• The time of length of stay in hospital among CABG or valve replacement as continuous variable.
Independent variable
• The use of BIS monitoring among CABG or valve replacement categorical variable
• Age
• Gender
• Time of surgery
Ethical issues
• Permission from institutional review board.
• Consent from was signed by the patients prior to participation.
• Confidentiality and voluntarily participation to all participants was ensured.
• Detailed explanation for all patients about aim and objectives of the study.
Data analysis plan
The Statistical Package of Social Sciences (SPSS) version 21 will be used for data entry and in statistical analysis, The data analysis plan will be summarized using descriptive summary measures: expressed as mean (SD) for continuous variables and percentage for categorical variables.
The significance level will be considered in this study is less than 0.05 by using t-Test and chi square for any predicted correlation between dependent and independent variable.
The primary predicted correlation will be measured by:
• T-test will be used to compare the mean extubation time between two groups.
• T-test will be used to compare the mean of patients length of hospital stay of between two groups.
Results
Data was collected from a total of 100 patients, between the age of 30 and 75 years were recruited in this study, with 50 patients randomly allocated in each group. All of them were male, underwent (CABG), and received coronary artery bypass during the surgery. The two groups were well matched with response to age, sex, body mass index, smoking history, and other comorbidities such as cardiac, pulmonary and renal diseases. The patients were randomized in two groups with the BIS group received titrated infusion of propofol to maintain BIS values between 40-50 in the operating room and 60-70 in the CCU, while the conventional group received anesthetic drugs without the use of BIS monitor during the surgery, and the sedation drugs was titrated to SAS sedation scale of zero in the intensive care. The majority of patients were ASA the majority of patients were ASA 3 and 4 with an ejection fraction above 40, the average number of vessels bypassed was three in both groups.
Regarding anesthetic time, the average anesthesia time was (290 min), and surgical time was (251 min), while the CPB time was (105 minutes) and the cross-clap time (85 min), the time was similar in both study and conventional groups.
Mean arterial blood pressure and heart rate which was recorded in the operating room and in the intensive care shows no significant difference.
The average use of midazolam is (8 mg in BIS group and 9 mg in control group) and fentanyl (1600 in BIS group and 1650 in control group).
The propofol infusion was started at the time of CPB and sevoflurane was discontinued, the infusion of propofol was continued during patients transfer to the CCU, and was stopped when weaning criteria was established. Body temperature during CPB was adapted to 28 degree Celsius, in both groups, during which propofol infusion was enough to keep BIS value less than 45.
Total amount of propofol which was used in both groups during surgery was (1050 mg BIS and 1145 mg in conventional group), while in the CCU (390 mg BIS, and 470 mg in conventional group).
In the CCU morphine was the drug used for analgesia which was given intermittently 1-1.5 mg hourly taking in consideration the hemodynamic stability of the patient, while at the time of extubation 2 mg of morphine was given to all patients in both groups. The total amount of morphine given to both groups was almost the same.
During weaning 22.1% of patients regained their consciousness in the first hour, and 57% of the patients regained their consciousness within 2 hours after surgery, and about 85% of the patients have an emergence time from anesthesia of less than 3 hours.
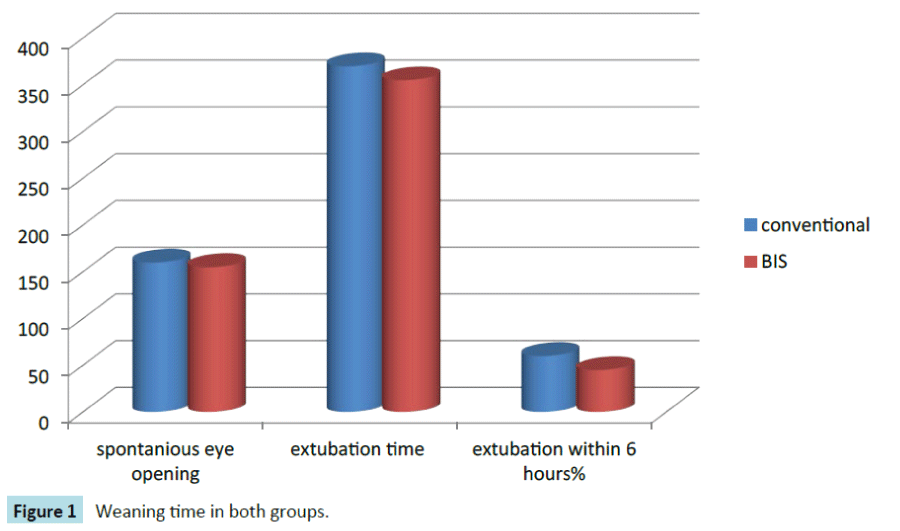
The time of extubation, was 320 minutes in BIS group and 365 minutes in conventional group, which showed that there was no significant difference in between both groups. Extubation within 6 hours after surgery which is used as a criteria to differentiate early versus late extubation did not show any significant difference as 70% of BIS group and 55% of conventional group were extubated before 6 hours.
The MAP values in BIS and conventional group at baseline was (92, 118 mmHg), were at intubation (75, 83 mmHg), at incision (80, 85 mmHg), at the beginning and end of CPB (60, 64 mmHg), and at the end of sterna wiring (72, 75 mmHg). On CCU the MAP for both BIS and conventional groups was almost similar in the first 6 hours, The BIS value was more than 70 at the time of eye opening and extubation.
No any intra operative complications necessitating the use of intra aortic balloon pump during weaning from CPB, such as severe hypotension, or hypoxia. We interviewed all the patients in the study post operatively at 12 hours after extubation by an investigator; each patient was asked the following questions:
1) What was the last thing you remember before surgery?
2) What was the very next thing you remember?
3) Can you remember anything in between these two periods?
4) Did you have any dreams during the surgery?
After data assessment we could not detect any recall (Tables 2-15) (Figure 1).
| Age |
N (100) |
MEAN |
SD |
Probability |
| BIS |
50 |
61.41 |
10.39 |
|
| Conventional |
50 |
66.59 |
9.259 |
0.097 |
| Height in cm |
| BIS |
50 |
173.6 |
9.48 |
0.450 |
| conventional |
50 |
171.9 |
9.45 |
|
| Weight in kg |
| BIS |
50 |
86.2 |
12.75 |
0.642 |
| conventional |
50 |
85.4 |
19.42 |
|
| Ejection fraction |
| BIS |
50 |
54.1 |
9.61 |
0.175 |
| conventional |
50 |
56.8 |
9.48 |
|
Table 2 Patientsâ€Âââ€Å¾Â¢ Demographics.
| ASA class |
BIS |
conventional |
Probability |
| 11 |
5(100%) |
0(0%) |
0.271 |
| 111 |
30(45%) |
27(48%) |
|
| 1V |
15(35%) |
23(62%) |
|
| total |
50 |
50 |
|
Table 3: ASA class.
| Total propofol |
number |
Median |
SD |
Probability |
| BIS |
50 |
1440mg |
675.4 |
0.450.4 |
| Conventional |
50 |
1615 |
1125.8 |
|
Table 4 Propofol given during surgery and in the CCU.
| Total morphine |
Number |
Median |
SD |
Probability |
| BIS |
50 |
5 |
4.6 |
0.64 |
| Conventional |
50 |
5 |
5.6 |
|
Table 5: Total amount of morphine given in the OR and CCU.
| Total fentalnyl |
number |
Median |
SD |
probability |
| BIS |
50 |
1700 |
692.3 |
071 |
| Conventional |
50 |
1675 |
681.1 |
|
Table 6: Total amount of fentanyl use during OR.
| Total medazolam |
number |
median |
SD |
Probability |
| BIS |
50 |
8 |
4.58 |
0.641 |
| Conventional |
50 |
8.5 |
3.98 |
|
Table 7: Total amount of medazolam use in the OR.
| Surgical time |
Number |
Median |
SD |
Probability |
| BIS |
50 |
290 min |
53.1 |
0.77 |
| Conventional |
50 |
285 min |
48.82 |
|
Table 8: Surgical time.
| Anesthesia time |
Number |
Median |
SD |
Probability |
| BIS |
|
251 min |
52.81 |
0.73 |
| Conventional |
|
248 min |
48.75 |
|
Table 9: Anesthesia time.
| Body temperature |
number |
Median |
SD |
Probability |
| BIS |
50 |
28 |
1.51 |
0.581 |
| Conventional |
50 |
28.5 |
1.28 |
|
Table 10: Body temperature during surgery.
| BIS reading |
Mean |
SD |
| Baseline |
89 |
14.9 |
| At intubation |
40 |
15.21 |
| At incision |
42.9 |
10.221 |
| At start of CBP |
39.8 |
10.176 |
| At end of CBP |
41.3 |
8.1 |
| At last suture |
45.7 |
9.11 |
Table 11: Intra-operative BIS reading.
| BIS reading |
mean |
SD |
| Admission |
58.2 |
14.72 |
| 1st hour |
61.8 |
16.21 |
| 2nd hour |
66.9 |
15.3 |
| 3rd hour |
74.3 |
17.2 |
| 4th hour |
77.8 |
17.4 |
| 5th hour |
80.2 |
18.1 |
| 6th hour |
77.6 |
17.5 |
| Eye opening |
73.8 |
17.1 |
| Start of weaning |
80.3 |
17.9 |
| Extubation |
90.7 |
8.42 |
Table 12: Post operative BIS reading in the CCU.
| Baseline MAP |
Number |
Mean |
SD |
Probability |
| BIS |
50 |
95.3 |
11.04 |
0.28.6 |
| conventional |
50 |
121.9 |
121.1 |
|
| MAP at intubation |
number |
mean |
SD |
Probability |
| BIS |
50 |
82.1 |
18.41 |
0.659 |
| Conventional |
50 |
79.89 |
14.72 |
|
| MAP at incision |
number |
mean |
SD |
Probability |
| BIS |
50 |
77.51 |
10.14 |
0.65 |
| Conventional |
50 |
79.81 |
19.76 |
|
| MAP at start of CBP |
number |
mean |
SD |
Probability |
| BIS |
50 |
67.91 |
9.87 |
0.91 |
| Conventional |
50 |
68.21 |
10.11 |
|
| MAP at end f CBP |
number |
mean |
SD |
Probability |
| BIS |
50 |
68.12 |
6.35 |
0.08 |
| Conventional |
50 |
66.87 |
8.52 |
|
Table 13: Intra operative hemodynamic (MABP).
| Baseline HR |
number |
mean |
SD |
Probability |
| BIS |
50 |
76.11 |
16.31 |
0.631 |
| Conventional |
50 |
74.78 |
17.42 |
|
| HR at intubation |
number |
mean |
SD |
Probability |
| BIS |
50 |
69.82 |
14.91 |
0.964 |
| Conventional |
50 |
69.95 |
13.95 |
|
| HR at incision |
number |
mean |
SD |
Probability |
| BIS |
50 |
68.43 |
14.71 |
0.825 |
| Conventional |
50 |
66.02 |
15.21 |
|
| HR at start of CBP |
number |
mean |
SD |
Probability |
| BIS |
50 |
65.32 |
14.53 |
0.787 |
| Conventional |
50 |
66.34 |
15.22 |
|
| HR at end of CBP |
number |
mean |
SD |
Probability |
| BIS |
50 |
68.75 |
12.11 |
0.889 |
| conventional |
50 |
76.32 |
10.43 |
|
Table 14: Intra operative hemodynamic.
|    Level |
Description |
Explanation |
| 1 |
Unarousable |
Minimal to response to noxious stimuli |
| 2 |
Very sedated |
Arouses to physcical stimuli. Doesn’t communicate or follow commands. May move spontaneously |
| 3 |
Sedated |
Difficult to arouse. Awakens to Verbal Stimuli or gentle shaking, but drifts off again. Follows simlle Commands |
| 4 |
calm/cooperative |
Calm, awakens eaisly Follows command |
| 5 |
Agitated |
Anxious or Mildly Agitated. Attempts to sit up. Calms with verbal instructions |
| 6 |
very agitated |
Doesn’t calm despite frequent verbal reminding of limits .Requries physical restraits. Bites ET tube |
| 7 |
Dangerous Agitated |
Pulling at ET tube. Tries to remove Catheters, climb over bedrail, strike at staff, and/or trashing side-to-side. |
Table 15: Sedation scale.
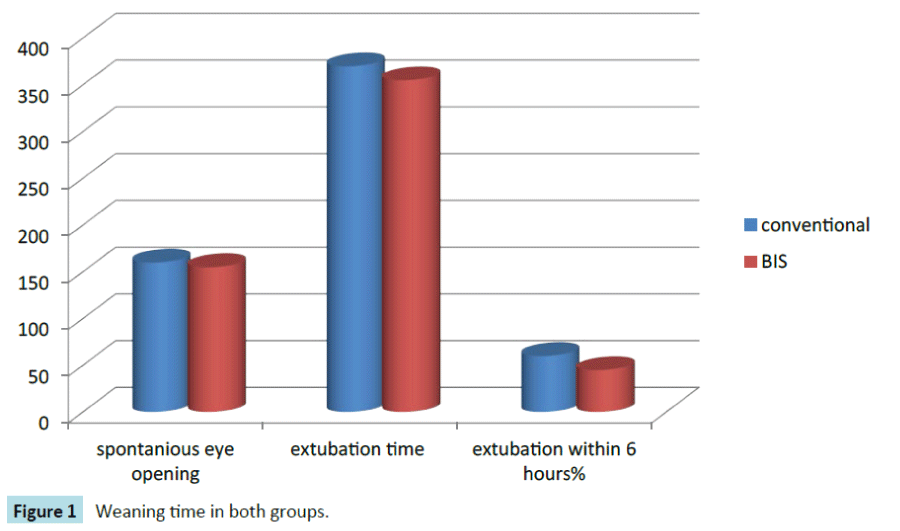
Figure 1: weaning time in both groups.
Discussion
Our study did not identify a significant difference in time to extubation after cardiac surgery between BIS group and conventional group, which were well matched in terms of co morbidities. There were also no significant differences in the CCU or total postoperative hospital length of stay.
BIS monitor has been introduced to the operating room to improve anesthetists the ability to administer anesthetic drugs, decrease emergence time and to improve patient’s outcome by early discharge from recovery room.
Subsequent analysis of large effectiveness studies did not show that BIS confers a benefit in overall time to recovery. Time to extubation following cardiac surgery has been an area of research in many studies, but few of them involve brain monitoring [33-37].
Ender et al. have described how the implementation of goalfocused process (creation of a specific cardiac recovery post anesthesia care unit and modifying intraoperative anesthesia) can greatly decrease time to extubation in selected patients (stable hemodynamics without inotropic support, no excessive bleeding and normothermia) [14]. Gooi et al. showed that the preoperative identification of a lower risk patient cohort allowed for earlier extubation in that fast-track group. However, neither study utilized brain monitoring [35].
Wong, et al. showed that increased age, female sex, use of inotropes, excessive bleeding, atrial arrhythmias, and presence of an intra-aortic balloon pump were associated with increased time to extubation. These variables represent potential confounders, but the group in our study showed no difference in age, sex, vasopressor use, excessive bleeding, or dysrhythmias. Also, the group was similar in the median age–adjusted MAC and total anesthesia time (Table 1) showing that anesthesia depth or duration had no effect on extubation times.
Johansen examined the impact of BIS on preoperative care. Anesthesia was maintained at BIS values between 50 and 65 (for at least 34% of time) with surgical duration of about one hour and was associated with earlier emergence and recovery from general anesthesia. In our study we failed to demonstrate a significant effect of BIS monitoring on recovery parameters in our group of patients undergoing coronary bypass surgery. No reduction in time to spontaneous eye opening, neither in earlier ventilator weaning and extubation.
Although most time to extubation studies in cardiac surgery patients have not included brain monitoring, a secondary analysis by Villafranca et al. from the BAGRECALL trial demonstrated that the use of a BIS protocol based on ageadjusted 0.7 MAC. A power analysis showed that 50 patients in each group would be required to detect a 30 minute difference in extubation time at a power of 0.95. Both their study and the present investigation greatly exceed 50 patients in each cohort. The current study confirms the previous findings and adds to the literature by demonstrating comparable results in a separate population.
Our study additionally demonstrates no difference in the secondary outcome of CCU length of stay or overall hospital length of stay. BIS monitor is not routinely employed in the coronary care units in our country; it cannot be concluded from the current study whether BIS monitoring in the CCU is beneficial for earlier extubation time.
Patients undergoing cardiac surgery may require increased depth of anesthesia commensurate with level of surgical stimulus such as sternotomy and pericardiotomy and BIS was designed to be maintained between 40 and 60 ranges. In our study BIS values dropped significantly to below 60 after induction and remained lower throughout CPB, and post CPB period. Scmidlin noted a much lower BIS value (median of 41) during hypothermic CPB (32ºC) with propofol sedation. He attributed it to brain cooling or increased propofol levels due to slow pharmacodynamics during cooling.
BIS monitoring has been used by many investigators in outpatient surgery, to titrate anesthetic depth, reduce exposure to anesthetic agents and facilitate early recovery and discharge. Patient group in our study focused in more selected group comprising of older male patients, predominantly ASA 111 and 1V undergoing elective coronary bypass surgery. A longer duration of anesthesia (5 hours) and physiological variables associated with CPB like hypothermia, hemodilution with change of drugs concentration, would be confounding variables, which preclude comparison with other studies that were performed on relatively healthy patients undergoing outpatient surgery.
Mukherji et al. compared the impact of BIS monitoring on fasttracking of 40 patients undergoing CPB. The study was similar to our study where patients divided in two groups with or without BIS monitoring. Authors found no significant difference between the two groups, not on eye opening, weaning time, time to extubate, and time of patient’s length of stay.
There are some limitations to this study, first, patients who operated late in the evening are ofen kept sedated and ventilated over night because of staffing issues when they may have otherwise been extubated. Thus, time to extubattion or CCU length of stay are potentially skewed by these confounds.
Second, because the initial trial involves awareness prevention, there were no lower limit alarms for BIS, and upper limit alarm for MAC, which might have altered anesthetic management in a way that influenced time to extubation.
Conclusions
There was no difference in time to extubation between BIS guided group and conventional group in patient population well matched for co morbidities and for potential confounders for prolonged intubation. There also were no statistically significant differences in CCU and total post operative hospital length of stay. Data from this study suggested that the use of the BIS monitor during cardio pulmonary bypass does not confer an advantage in earlier extubation.
We speculated that the advantages in BIS monitoring were minimized by other complex nature and duration of the surgery, hypothermia, inability to initiate ventilator weaning in the immediate post operative period unlike surgery in other setting.
9490
References
- Liu J, Singh H, White PF (1996) Electroencephalogram bispectral analysis predicts the depth of midazolam-induced sedation. Anesthesiology 84: 64-69.
- De Deyne C, Struys M, Decruyenaere J, Creupelandt J, Hoste E, et al. (1998) Use of continuous bispectral EEG monitoring to assess depth of sedation in ICU patients. Intensive Care Med 24: 1294-1298.
- Nasraway SAJr, Wu EC, Kelleher RM, Yasuda CM, Donnelly AM (2002) How reliable is the Bispectral Index in critically ill patients? A prospective, comparative, single-blinded observer study. Crit Care Med 30: 1483-1487.
- Simmons LE, Riker RR, Prato BS, Fraser GL (1999) Assessing sedation during intensive care unit mechanical ventilation with the Bispectral Index and the Sedation-Agitation Scale. Crit Care Med 27: 1499-1504.
- Johansen JW, Sebel PS, Sigl JC(2000) Clinical impact of hypnotic-titration guidelines based on EEG bispectral index (BIS) monitoring during routine anesthetic care. J ClinAnesth 12:433-443
- Wong J, Song D, Blanshard H, Grady D, Chung F (2002) Titration of isoflurane using BIS index improves early recovery of elderly patients undergoing orthopedic surgeries. Can J Anaesth 49: 13-18.
- Sebel PS, Bowdle TA, Ghoneim MM (2004) The incidence of awareness during anesthesia: a multicenter United States study. AnesthAnalg 99: 833-839
- Pavlin DJ, Hong JY, Freund PR, Koerschgen ME, Bower JO, et al. (2001) The effect of bispectral index monitoring on end-tidal gas concentration and recovery duration after outpatient anesthesia. AnesthAnalg 93: 613-619.
- Zohar E, Luban I, White PF, Ramati E (2006)Bispectral index monitoring does not improve early recovery of geriatric outpatients undergoing brief surgical procedures. Can J Anesth 53: 20-25.
- Song D, Joshi GP, and White PF (1997) Titration of volatile anesthetics using Bispectral Index facilitates recovery after ambulatory anesthesia. Anesthesiology 87: 842-848.
- Myles PS, Leslie K, McNeil J, Forbes A, Chan MT (2004) Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet 363: 1757-1763.
- Afanador C, Marulanda L, Torres G, Marín A, Vidal C, et al. (2010) Effect of intraoperative use of dexmedetomidine on anesthetic requirements and time to tracheal extubation in elective adult heart surgery patients. A retrospective cohort study. Internet Journal of Anesthesiology 22: 24
- Caputo M, Alwair H, Rogers CA, Pike K, Cohen A, et al. (2011) Thoracic epidural anesthesia improves early outcomes in patients undergoing off-pump coronary artery bypass surgery: A prospective, randomized, controlled trial Anesthesiology 114: 380-390.
- Ender J, Borger MA, Scholz M, Funkat AK, Anwar N, et al. (2008) Cardiac surgery fast-track treatment in a postanesthetic care unit: Six-month results of the leipzig fast-track concept Anesthesiology 109: 61-66.
- Georghiou GP, Stamler A, Erez E, Raanani E, Vidne BA, et al (2006). Optimizing early extubation after coronary surgery Asian Cardiovascular & Thoracic Annals, 14: 195-199.
- Quinlan JJ, Homanics GE, Firestone LL (1998) Anesthesia sensitivity in mice that lack the beta3 subunit of the gamma-aminobutyric acid type A receptor. Anesthesiology 88: 775-780.
- Rampil IJ, Mason P, Singh H (1993) Anesthetic potency (MAC) is independent of forebrain structures in the rat. Anesthesiology 78: 707-712.
- Rampil IJ (1994) Anesthetic potency is not altered after hypothermic spinal cord transection in rats. Anesthesiology 80: 606-610.
- Antognini JF, Schwartz K (1993) Exaggerated anesthetic requirements in the preferentially anesthetized brain. Anesthesiology 79: 1244-1249.
- KissinI (1993) General anesthetic action: an obsolete notion? AnesthAnalg 76: 215-218.
- Lysko GS, Robinson JL, Casto R, Ferrone RA (1994) The stereospecific effects of isoflurane isomers in vivo. Eur J Pharmacol 263: 25-29.
- Morgan PG, Usiak MF, Sedensky MM (1996) Genetic differences affecting the potency of stereoisomers of isoflurane. Anesthesiology 85: 385-392.
- Iselin-Chaves IA, Flaishon R, Sebel PS (1998) The effect of inter-action of propofol and alfentanil on recall, loss of consciousness, and the bispectral index. AnesthAnalg87: 949 -955.
- Kearse LA Jr, Rosow C, Zaslavsky A(1998)Bispectral analysis of the electroencephalogram predicts conscious processing of in-formation during propofol sedation and hypnosis. Anesthesiol-ogy 88: 25-34.
- Mi WD, Sakai T, Singh H, Kudo T, Kudo M, et al. (1999) Hypnotic endpoints vs. the bispectral index, 95% spectral edge frequency and median frequency during propofol infusion with or without fentanyl. Eur J Anaesthesiol 16: 47-52.
- Sleigh JW, Andrzejowski J, Steyn-Ross A, Steyn-Ross M (1999) Thebispectral index: a measure of depth of sleep? AnesthAnalg 88: 659-661.
- Schnider TW, LuginbuÈ hl M, PetersenFS, Mathis J (1998)Unrea-sonably low bispectral index values in a volunteer with genet-ically determined low-voltage electroencephalographic signal. Anesthesiology 89:1607-1608.
- Katz SM (1999) The media and the BIS monitor. Anesthesiology 90: 1796-1798.
- Chong JL, Grebenik C, Sinclair M, Fisher A, Pillai R, et al. (1933)The effect of a cardiac surgical recovery area on the timing of extubation. J CardiothoracVascAnesth7: 137-141.
- Kertai MD, Pal N, Palanca BJ, Lin N, Searleman SA, et al.(2010)Association of perioperative risk factors and cumulative duration of low bispectral index with intermediate-term mortality after cardiac surgery in the B-Unaware Trial. Anesthesiol 112:1116-1127.
- Whitlock EL, Torres BA, Lin N, Helsten DL, Nadelson MR, et al. (2014) Postoperative delirium in a substudy of cardiothoracic surgical patients in the BAG-RECALL clinical trial. AnesthAnalg 118:809-817.
- Chan MT, Cheng BC, Lee TM, Gin T (2013)BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J NeurosurgAnesthesiol 25:33-42.
- Tyson GS, Sladen RN, Spainhour V, Savitt MA, Ferguson TB Jr, et al. (1989) Blood conservation in cardiac surgery. Preliminary results with an institutional commitment. Ann Surg 209: 736-742.
- Fritz BA, Rao P, Mashour GA, Abdallah AB, Burnside BA, et al. (2013) Postoperative recovery with bispectral index versus anesthetic concentration-guided protocols. Anesthesiology 118: b1113-1122.
- Gooi J, Marasco S, Rowland M, Esmore D, Negri J, et al. (2007) Fast-track cardiac surgery: application in an Australian setting. Asian CardiovascThorac Ann 15:139-143.
- London MJ, Shroyer AL, Coll JR, MaWhinney S, Fullerton DA, et al. (1998) Early extubation following cardiac surgery in a veterans population. Anesthesiology 88: 1447-1458.
- Cheng DC, Karski J, Peniston C, Raveendran G, Asokumar B, et al. (1996) Early tracheal extubation after coronary artery bypass graft surgery reduces costs and improves resource use. A prospective, randomized, controlled trial. Anesthesiol 85:1300-1310.