Mohammadreza Azimi*
Department of Aerospace Group (New Sciences and Technologies), University of Tehran, Amirabad, Iran
- *Corresponding Author:
- Mohammadreza Azimi
Department of Aerospace Group(New Sciences and Technologies),
University of Tehran,
Amirabad,
Iran,
E-mail: m_r_azimi1991@yahoo.com
Received Date: August 09, 2021;Accepted Date: August 23, 2021; Published Date: August 30, 2021
Citation: Azimi M (2021) Iris Recognition for Smokers and Non-Smokers. J BioMed Sci Vol.10 No.5:60.
Smoking is one of the most common habits around the world and the immediate effect of smoking on the performance of voice recognition systems has been studied. Smoking is also known as a social issue that can lead to voice deviations, vocal changes, and acoustics complaints, as reported in which the sub data from the NIST telephone recording database was used.
However, no tests have been conducted to investigate the reliability of iris recognition systems for smokers and nonsmokers. The purpose of this section is to understand whether the biometrics results are better for non-smokers in comparison with heavy smokers. According to the obtained results, the iris recognition system performed very well for both smokers and non-smokers groups.
Keywords
Heavy smokers; Intra ocular pressure; Biomechanical; Hypothesis test
Introduction
The negative impact of pupil dilation on iris recognition performance has been reported by several researchers. Karakaya and Celik, quantified the effects of pupil dilation and gaze angle on real frontal and off-angle images at various levels of dilation [1]. The experiments revealed that larger differences in dilation levels and gaze angles between the compared iris images increase the Hamming distance. Analyzed the impact of drugs on pupil dilation, proposes the use of a biomechanical nonlinear iris normalization scheme along with a key point-based feature matching for mitigating the impact of drug-induced pupil dilation on iris recognition, and investigates differences between drug-induced and light-induced pupil dilation on iris recognition performance [2,3]. In a paper written by the acute effects of smoking on Intra Ocular Pressure (IOP) and pupil size were presented [4]. In their study, 52 healthy habitual cigarette smokers were recruited and the achieved results showed that the photopic pupil sizes of the subjects before and after smoking were significantly different. The mean Intra Ocular Pressure (IOP) after smoking was also significantly higher than the Intra Ocular Pressure (IOP) before smoking. For the hypothesis test, a T-test was used. In another study by the same authors, pupil sizes and total ocular aberrations were assessed by an optical path difference scanning system (OPD-Scan II ARK-10000, NIDEK) and only the right eyes were considered for statistical analysis. Statistical Package for the Social Sciences (SPSS) version 11.0 statistical software system was used for all statistical analyses and was regarded as statistically significant. They reported that the smokers in the study had an abstinence period for at least 12 hours before the measurements; hence the psychological relaxation after smoking in chronic smokers may also cause the inhibition of sympathetic activation in the abstinence period. In one paper, the authors evaluated the acute changes in objective accommodation and Ocular Wavefront Aberrations (OWA) after cigarette smoking.
Materials and Methods
For the purpose of collecting a new database, regular cigarette smoker volunteers from the staff of Babol University of Medical Sciences were recruited in the study. The participants were required to meet the criteria of having smoked 15 or more cigarettes per day for at least a five-year period. Informed consent was obtained from all of the volunteers. Our new database contains 284 iris samples taken from 41 eyes of smokers and 390 iris samples from 87 eyes of non-smokers (Figure 1).
Figure 1: Iris samples-a: non-smoker, b: smoker.
The experiment was specifically designed to investigate whether there is any relation between the accuracy of the iris recognition system and the fact that the users smoked, or not. Personal data were kept separately, in order to guarantee additional security of the personal data. All of the participants were fully aware of the experiment as full detailed information on the study was provided and signed consent forms were also obtained from all of the individuals. The experiment protocol was approved by the Ethics Committee of the Warsaw University of Technology.
In order to calculate the comparison score between samples (for an all vs all comparison scenario), we have again used the University of Salzburg Iris Toolkit (USIT). For iris segmentation, the Weighted Adaptive Hough and Ellipsopolar Transform methodology was used. We have selected a descriptor for feature extraction: the iris coding method based on differences of Discrete Cosine Transform (DCT). In our chosen strategy, all of the images would be compared to the entire database and a score would be obtained for each.
Results and Discussion
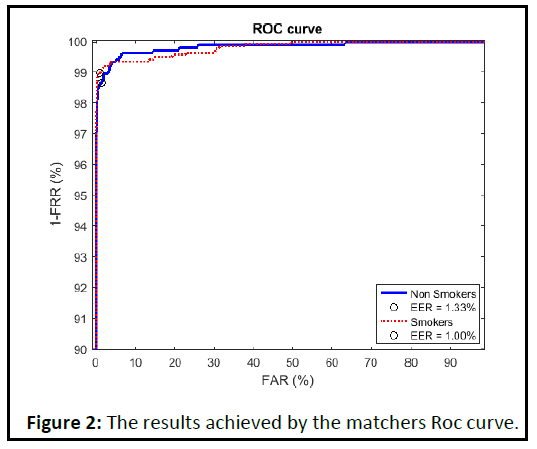
The ROC curve was presented in Figure 2. The methodology used was Discrete Cosine Transform (DCT). As shown in the figure, and according to the results achieved by the matchers, the accuracy of the system is the same when recognizing healthy people and chain smokers using their iris texture images. A very good performance was observed by using the methodology proposed by Discrete Cosine Transform (DCT) [5].
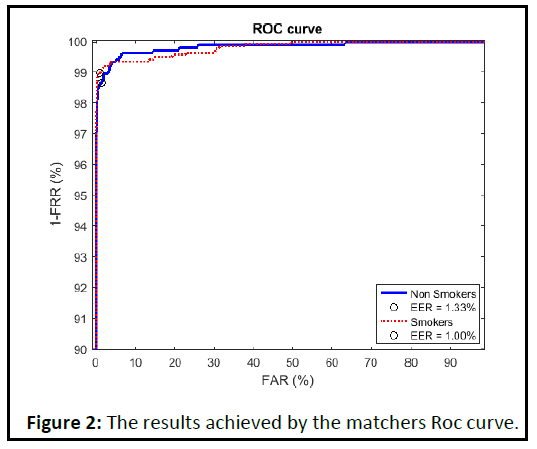
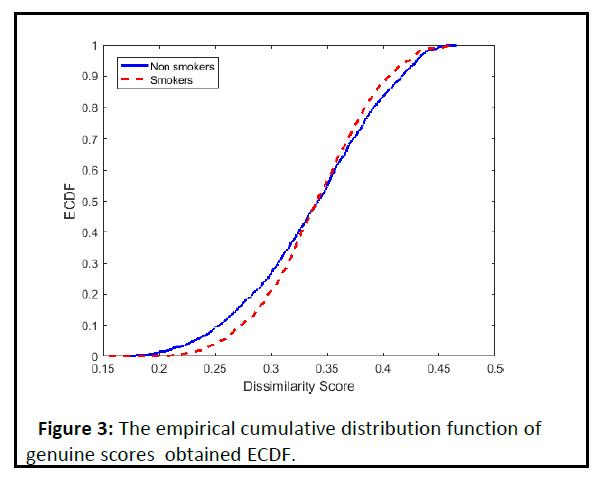
Figure 2: The empirical cumulative distribution function of genuine score s obtaine d ECDF ..
As shown from Figure 3, the empirical cumulative distribution function of genuine scores obtained by Discrete Cosine Transform (DCT) codes does not show any observable differences between those comparison scores obtained by comparing iris samples donated by smokers and those matching results achieved by a comparison of iris pattern images taken from healthy irides. Iris recognition effectiveness is same for both smokers and non-smokers.
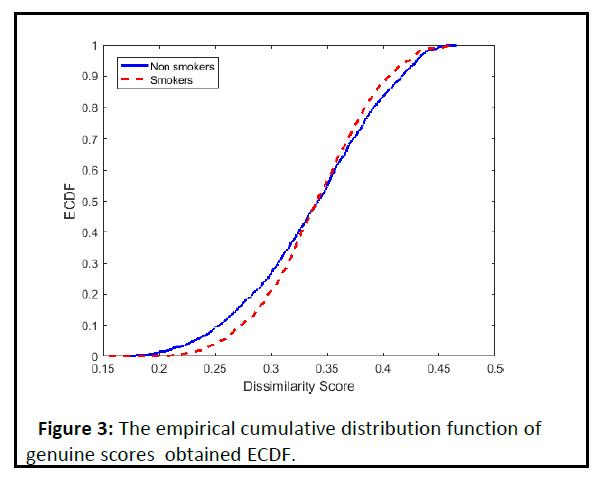
Figure 3: The results achieved by the matchers Roc curve.
Conclusion
To address whether cigarette smoking actually has an effect of reducing the matching accuracy of iris recognition systems, our study examined the effect of smoking on the reliability of an iris identification system. Our newly offered database consists of 674 NIR iris images taken from 128 eyes by using a monocular Iri Shield camera. In order to segment the iris and calculate the comparison score between samples, the University of Salzburg Iris Toolkit (USIT) was successfully used. We conducted the same test with four different iris recognition systems, to make sure we were testing the eyes, and not the quality of the various algorithms. In each case, the results were the same. We can confidently state that “Iris recognition is robust against the smoking condition of the users.”
39333
References
- Mahmut Karakaya, Elif T Celik (2019) Effect of pupil dilation on off-angle iris recognition. J Electronic Imaging 28:033022.
- Inmaculada Tomeo-Reyes, Arun Ross, Vinod Chandran (2016) Investigating the impact of drug induced pupil dilation on automated iris recognition.
- Uzeyir Erdem, Gokcen Gokce, Fatih Cakir Gundogan, Atilla Bayer, Gungor Sobaci (2011) Effect of Smoking on Intra Ocular Pressure Wavefront Aberrations and Pupil Changings. Investi Ophthalmol Visual Sci 52:5191.
- Uzeyir Erdem, Fatih C Gundogan, Umut AslÃÂâÂÂÃÂñ Dinc, Umit Yolcu, Abdullah Ilhan, et al. (2015) Acute Effect of Cigarette Smoking on Pupil Size and Ocular Aberrations: A Pre- and Post-smoking Study. J Ophthalmol 5:625470
- Handan Bardak, Murat Gunay, Yavuz Bardak, Yesim Ercalik, Serhat Imamoglu, et al. (2017) Evaluation of the acute changes in objective accommodation, pupil size and ocular wavefront aberrations after cigarette smoking. Cutaneous and Ocular Toxicology 36:25-28.