Jomal Mathew*
Department of Neurology, Little Flower Hospital and Research Centre, Angamaly, Kerala, India
- *Corresponding Author:
- Jomal Mathew
Department of Neurology
Little Flower Hospital and Research Centre
Angamaly, Kerala, India
E-mail: admin@lfhospital.org
Received Date: March 04, 2021; Accepted Date: March 18, 2021; Published Date: March 25, 2021
Citation: Mathew J (2021) Isolated Orthopnea in Myasthenia Gravis. J Neurol Neurosci Vol.12 No.3:356.
Keywords
Thymoma; Orthopnea; Myasthenia gravis; Diaphragmatic palsy
Main Document
A 62 year male presented to emergency at midnight with acute onset hortness of breath for few hours duration present only in the supine state and relieved in sitting position. There was low grade fever for 2 days along with cough, scanty mucoid expectoration and frequent hiccoughs for which he had been given antipyretics and cough expectorants at local hospital. There was no associated drooping of eyelids, speech difficulty, limb weakness, chest pain or palpitations. Two years back he was diagnosed with myasthenia gravis and invasive thymoma for which he underwent thymectomy and resection of left phrenic nerve with left hemidiaphragmatic plication, followed by radiotherapy. He was on treatment with pyridostigmine 180 mg/day and azathioprine 50 mg daily. There was no history of coronary artery disease, diabetes or hypertension.
On examination, patient was conscious, alert and comfortable in room air in sitting position. The vital signs were normal. Paradoxical movement of diaphragm was the only significant neurological finding. Cardiovascular examination was normal. Respiratory examination showed reduced air entry on the left with no added sounds. The clinical impression was orthopnoea due to diaphragmatic weakness resulting from exacerbation of myasthenia by the lower respiratory infection or recurrence of thymoma. An impending myasthenic crisis was closely watched for. A possible cardiac cause for orthopnea was also considered.
The hematological investigations showed elevated total leukocyte count of 14450/mm3 with 92 % neutrophils and 7% lymphocytes. Biochemical parameters including liver function renal function and serum electrolytes were normal. An electrocardiogram and echocardiography ruled out cardiac pathology. The serum acetylcholine receptor antibody was positive 29.29 nmol/L by radioimmunoassay .Contrast enhanced CT chest showed collapse consolidation and mild bronchiectasis on the left paracardiac lung likely old infection with reactivation and mild enlarged mediastinal and sub carinal lymph nodes. Whole body PET CT scan was normal with no e/o thymoma recurrence / metastases.
The patient was started on piperaciilin /tazobactum and the dose of pyridostimine increased to 240 mg daily. The patient developed worsening respiratory distress after 12 hours of admission with oxygen desaturation(<80%) even in sitting state which promptly responded to neostigmine 1.5 mg intramuscular with atropine (0.6 mg intravenous) premedication four times daily along with oxygen 2litres /min. His respiratory distress improved gradually over 4-5 days.He was started on low dose prednisolone 20 mg daily and azathioprine dose increased to 100 mg daily. He was closely monitored for any need for mechanical ventilation and plasma exchange but could be managed conservatively.
Results and Discussion
Myasthenia gravis is common neuromuscular illness characterized by fatiguable and fluctuating weakness of commonly the extra ocular muscles, the bulbar muscles, neck and the proximal muscles of the extremities. Acute exacerbation in a myasthenic patient already on treatment is known to be triggered by infections, certain drugs, emotional stress, surgery, climate change etc [1]. Recurrence of thymoma is another potential cause for worsening of weakness [2]. The patients present with worsening weakness of ocular, bulbar, neck or limb muscles and in severe cases respiratory muscles are involved necessitating mechanical ventilation (myasthenic crisis). Isolated involvement of respiratory muscles and presentation with respiratory symptoms alone during exacerbation of myasthenia is unusual and has been rarely reported [3,4]. The patient in this case presented with acute onset orthopnea due to diaphragmatic palsy with no systemic features of myasthenia ( no ptosis on prolonged upgaze>1 minute e and the forearm abducton time was>3 minutes ) [1]. A new onset diaphragmatic weakness due to neuromuscular pathology or right phrenic nerve palsy was considered. The prompt response of orthopnea to parenteral neostigmine suggested myasthenia related weakness. The lower respiratory tract infection seemed to be the only trigger factor. Repetitive nerve stimulation study was not feasible as the patient was on pyridostigmine which could not be discontinued. Isolated involvement of phrenic nerve due to brachial neuritis is a rare cause for diaphragmatic palsy but the prompt response of orthopnea to parenteral choline esterase inhibitor is against it [5].
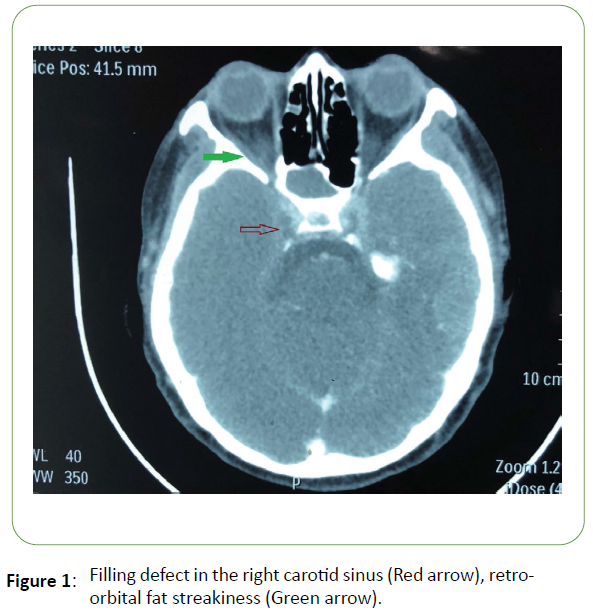
The preexisting subclinical diaphragmatic dysfunction with superimposed myasthenic weakness may explain the rare presentation of myasthenia exacerbation as isolated orthopnea. Recurrence of thymoma which could cause diaphragmatic palsy and exacerbate myasthenia was ruled out by appropriate imaging studies. About 95% and 70% of thymoma (regardless of age) patients have titin and RyR antibodies respectively. Anti RyR antibody is associated with neck weakness,respiratory and bulbar symptoms at the onset while titin antibody is linked to respiratory symptoms [2,6,7]. The reason for the selective weakness of bulbar and respiratory muscles in association with these antibodies is not known. The patient at the diagnosis of myasthenia 2 years back had presented with swallowing difficulty, drooping of eyelids and neck weakness indicating the probable presence of these antibodies. He was negative then for acetylcholine receptor antibody but turned positive now (Figure 1)
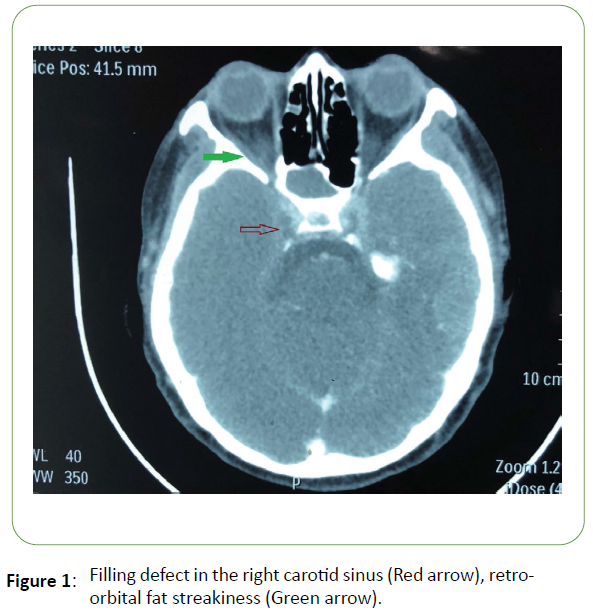
Figure 1: Filling defect in the right carotid sinus (Red arrow), retroorbital fat streakiness (Green arrow).
Conclusion
Removal of thymoma is not associated with disappearance of anti-titin, anti RyR and anti-AChR antibodies. Serum anti titin antibody and Ryanodine receptor (RyR) antibody assay was considered but was not available.The case is being highlighted for the rare occurrence of isolated orthopnea in myasthenia and its implications with regard to thymoma and antibody profile.
Acknowledgement
All authors wish to acknowledge the staff in EDXRF laboratory at Centre for Energy Research and Development, Obafemi Awolowo University, Ile-Ife for their support during sample preparation and analysis.
35814
References
- Gold R, Hohlfeld R, Toyka K V (2008) Progress in the Treatment ofnMyasthenia Gravis. Therapeutic Advances Neurol Disorders 1:n99-114.
- Romi F (2011) Thymoma in Myasthenia Gravis: From Diagnosis tonTreatment. Autoimmune Dis 14:101-110.
- Ray A, Nangia V, Chatterji R, Bante N (2017) Respiratory Failure inna Patient with Treated Thymoma: A Blast from the Past. Egypt JnBronchol 11:168-170.
- Kim W H, Kim J H, Kim E K, Yun S P, Kim K K, et al. (2010)nMyasthenia Gravis Presenting as Isolated Respiratory Failure: anCase Report. Korean J Intern Med 25: 101.
- Nardone R, Bernhart H, Pozzera A, Taddei M, Tezzon F(2000).nRespiratory Weakness in Neuralgic Amyotrophy: Report of TwonCases with Phrenic Nerve Involvement. Neurol Sci 21: 177-181.
- Romi F, Aarli J A, Gilhus N E. (2007) Myasthenia Gravis Patientsnwith Ryanodine Receptor Antibodies has Distinctive ClinicalnFeatures. Eur J Neurol 14: 617-620.
- Baggi F, Andreeta F, Antozzi C, Simoncini O, Confalonieri P, et al.n(1998) Anti-Titin and Antiryanodine Receptor Antibodies innMyasthenia Gravis Patients with Thymoma. Annals New York AcadnSci 841: 538-541.