Key words
Splenic abscess, tuberculosis
Introduction
With epidemics of HIV infection assaulting humanity through recent decades, tuberculosis has resurged as a major health hazard even in developed nations. Due to declining of CD4+ level and subsequent suppression of cell-mediated immunity, vulnerability to tuberculosis and other cellular immunityeradicated parasites is anticipated. In these patients, physical examination may or may not reveal pulmonary tuberculosis; but as well as pulmonary involvement, Extra-pulmonary manifestations of tuberculosis seem to evolve in a more aggressive fashion. However, reticuloendothelial involvement including lymphadenopathy and organomegally is frequently observed. Among these variable conditions, isolated splenic tuberculosis is an extremely rare presentation, and is most often observed in severely immunocompromised patients [1]. We report a 24- year- old HIV-positive man with isolated splenic tuberculosis presenting with splenic abscesses and fever of unknown origin.
Case presentation
A 24-year-old man, injection drug user (IDU) and HIV-positive was admitted to infectious department of Imam Khomeini hospital in February 2010. He complained of fever and chills. Moreover, he mentioned night sweating and significant weight loss from 2 months ago. He had also noted pleuretic chest pain during the last month. On examination, he was febrile; and except for a pale conjunctivae and a palpable spleen, further signs or symptoms were negative. Laboratory examinations revealed anemia (Hb=9.5 gr/dl) and thrombocytopenia (plt=80000 cells/ml). Other remarkable lab data included ESR (Erythrocyte Sedimentation Rate)=85 ml/h and a CD4+ level equal to 230 cells/ml. PPD skin test was not reactive and chest X-ray was also normal. Moreover, he did not receive HAART (highly active anti-retroviral therapy) for HIV infection.
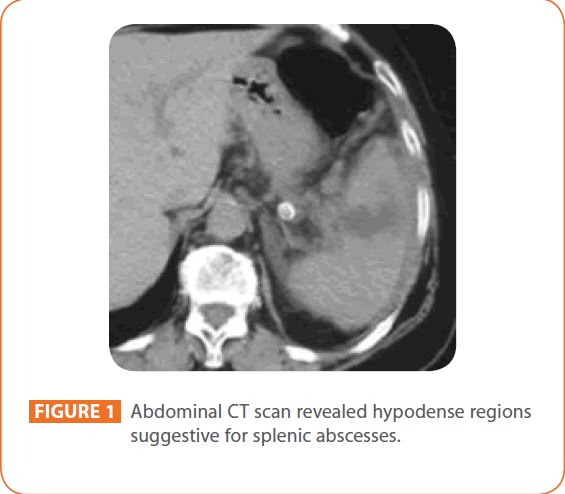
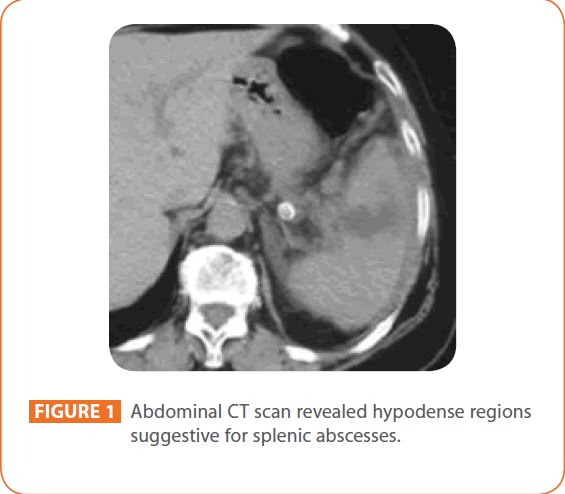
Figure 1: Abdominal CT scan revealed hypodense regions suggestive for splenic abscesses.
Splenomegally, in addition to multiple hypodense regions suggestive for splenic abscesses were identified via abdominal sonography and CT scan.
Considering these findings, several antibiotics including ceftriaxon (1 gr bd), vancomycin (1gr bd) and metronidazole (500mgr 6hourly) were abruptly initiated, but no improvement was recorded within the next 72 hours with the patient yet to be febrile. Other diagnostic procedures including bone marrow aspiration and biopsy were reported as normal. Thereby, diagnostic laparatomy and splenectomy were performed. Further pathological assessments of the spleen revealed chronic granulomatous and caseous inflammation, highly suggestive of tuberculosis infection. Definite tuberculosis infection became evident after that Ziehl- Neelsen staining of the inflammated tissue was performed and suspected acid-fast bacilli of Mycobacterium tuberculosis was detected under microscopy. Moreover, no further sign of tuberculosis was observed wherever else in the patient. Shortly after the diagnosis was established, tuberculostatic treatment including isoniazid (300 mg daily), rifampicin (600 mgr daily) ethambutol (800 mgr daily) and pyrazinamide (1000 mgr daily) was initiated. Prior to initiation of treatment, dosages for ethambutol and pyrazinamide were adjusted to the weight of the patient. He eventually began to improve and the fever resolved within 10 days.
Discussion
Extra-pulmonary tuberculosis is one of the most prevalent opportunistic infections reported among HIV infected patients, especially in tuberculosis endemic regions of the world [2]. In particular, it has been shown that extra-pulmonary tuberculosis is the commonest cause of fever of unknown origin in HIV infected patients. Although atypical manifestations are common among this group, abdominal involvement has been rarely described to date. Some reports have implicated a higher incidence of spleen tuberculosis within HIV infected patients. As a matter of fact, almost every system is essentially involved during miliary tuberculosis, with the spleen being the third most frequently affected organ after lung and liver; but primary or isolated forms of splenic involvement have been rarely reported [3-4].
Immunocompromised patients are drastically predisposed to evolution of various complications such as splenic abscesses [5- 8]. In fact, considering rarity of splenic abscesses, these lesions are more frequently observed in immunocompromised hosts, such as in HIV infected patients or those with malignancies [8]. Under this circumstance, ischemia and subsequent infarction of the spleen provokes infections and development of multiple abscesses. Moreover, immunocompromised state is also correlated with poor prognosis and higher mortality rates among these patients [8]. Taking into consideration the possibility of spleen abscesses in IDU patients, endocarditis as well as other hematogenous means is suspected to be the main underlying reason that facilitates abscess formation by opportunistic etiologies [6 - 9]. Such opportunistic germs including mycobacteria are primarily known to account for abscess development, while other associates to this condition include staphylococci, streptococci, some certain gram negative bacilli and anaerobes [8]. It must also be noted that mycobacteria often cause caseating necrosis lesions and abscess development is a rare entity in these infections; whereas in our patient, splenic abscesses and caseating lesions were concomitantly observed.
Until 1992, only six cases of primary splenic tuberculosis have been reported throughout English, French and German literature. In 2008, a primary case of splenic TB has been reported in an Iranian immunocompetent patient [10].
Several other studies have implicated development of splenic abscess in immuncompetent patients [6, 11-13]. In all of these studies, fever and left hypochondrial pain were the most frequently noted symptoms, whereas our patient was referred with malaise, fever and chills. Additionally, we did not recognize any signs of cardiovascular involvement in our patient and his lab data were merely suggestive for a high inflammatory index. The primary involvement of spleen with no evidences of miliary tuberculosis was established with detection of multiple abscesses via imaging modalities. A case series study in India has proposed ultrasonography of the spleen as an affordable, non-invasive imaging modality which can be useful in diagnosis of splenic abscess [3].
Our case represents an atypical form of extra-pulmonary tuberculosis in HIV-positive patients. Under this circumstance, splenectomy in addition to standard tuberculostatic treatment has been suggested [6]. Additional studies are required to highlight the implication of CD4+ level in development of such complications.
217
References
- Pramesh CS, Tamhankar AP, Shah SR (2002) Splenictuberclosis and HIV-1 infection. Lancet 26: 353-369.
- Murray JF (2005) pulmonary complications of HIV-1 infection among adults living in sub-saharan Africa. Int J Tuberc Lung Dis 9: 826-835.
- Sharma SK, Smith-Rohrberg D, Tahir M, Mohan A, Seith A (2007) radiological manifestations of splenic tuberculosis: a 23 patient case series from India. Indian J Med Res 125: 669-678.
- Arab M, Mansoori D, Abbasidezfouli A, Sjadmehr M, Afsari M (2002) splenic tuberculosis: a case report. ActaMedicaIranica 40 (1): 26-28.
- Dixit R, Arya MK, Panjabi M, Gupta A, Paramez AR (2010) clinical profile of patients having splenic involvement in tuberculosis. Indian J Tuberc 57(1): 25-30.
- Saber A (2009) multiple splenic abscesses in a rather healthy woman: a case report. Cases J 23(2):7340.
- Barone B, Kreuzig PL, Gusmao PM, Chamie D, Bezerra F, et al (2006) case report of lymph nodal, hepatic and splenic tuberculosis in an HIV-positive patient. Braz J Infec 10(2): 149-153.
- Chang KC, Chuah SK, Changchien CS, Tsai TL, Lu SN, et al (2006) clinical characteristics and prognostic factors of splenic abscess: a review of 67 cases in a single medical center of Thaiwan. World J Gasteroenterol 12(3) 460-464.
- Ayaslioglu E, Basar H, Duruyurek N, Kalpaklioglu F, Gocmen S, et al (2009) disseminated tuberculosis with lymphatic, splenic and scrotal abscesses: a case report. Cases J 2:6995.
- Fooladi AA, Hosseini MJ, Azizi T (2009) splenic tuberculosis: a case report. Int J of Infec Dis 13: 273-275.
- Jain M, Singh S, Thomas S, Jain D (2008) acid fast bacilli isolated tubercular splenic abscess in a HIV-negative patient. Indian J PatholMicrobiol 51:74-75.
- Murray AW, Mcgregor AB (2000) a case of multiple splenic abscesses managed non-operatively. J R CollSurgEdinb 45: 189-191.
- Udgaonkar U, Kulkarni S, Shah S, Bhave S (2010) asymptomatic isolated tubercular abscess in an immunocompetentperson. Indian J of Med Microbiol 28(2): 172-173.