Gascón-Rubio MC1, Vereas-Martínez A2 and Ubis-Rodríguez E3
1Otorhinolaryngology Department, Hospital Santiago Apóstol, Miranda de Ebro, Burgos, Spain
2Pediatrics Department, Hospital Santiago Apóstol, Miranda de Ebro, Burgos, Spain
3Radiology Department, Hospital Santiago Apóstol, Miranda de Ebro, Burgos, Spain
*Corresponding Author:
Cristina Gascón-Rubio
Otorhinolaryngology Department
Hospital Santiago Apóstol, Burgos, Spain
Tel: 947349000
Email: crisgascon81@hotmail.com
Received Date:February 25 2016; Accepted Date:December 25 2016; Published Date:December 30 2016
Citation: Gascón-Rubio MC, Vereas-Martínez A, Ubis-Rodríguez E. Juvenile Recurrent Parotitis: A Case Report. Ann Clin Lab Res. 2016, 4:4. doi: 10.21767/2386-5180.1000143
Keywords
Juvenile recurrent parotitis, Sialography, Ultrasonography
Clinical Case
We report the case of a boy of 5 years old with no history of personal interest or family. The patient was referred by his paediatrician for filing in the past 10 months three episodes of parotid swelling. The episodes are self-limiting in 3-5 days duration and have given anti-inflammatory outlet. In the first episode he was prescribed antibiotics amoxicillin plus clavulanic acid orally because it showed low-grade fever. None of the episodes great malaise occurred.
In clinical examination consultation coinciding with the fourth episode of mumps it was performed. The patient had a diffuse increase the right parotid gland. He showed no trismus or alterations in the oropharynx. By bimanual palpation no collections were detected and only diffuse enlargement of the parotid gland was assessed. Culture samples of saliva were taken by the duct Stennon resulting in normal flora.
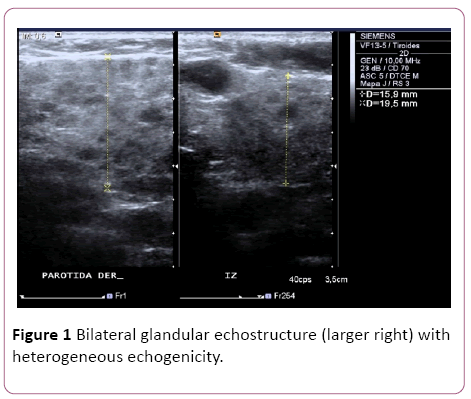
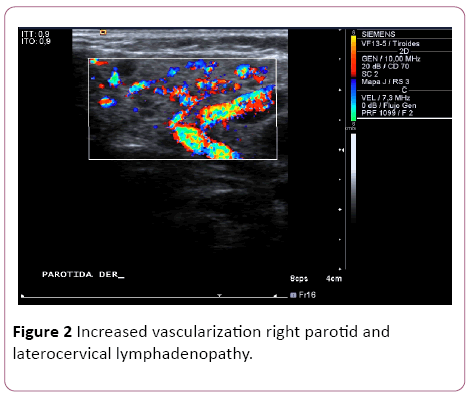
Ultrasonography of the acute process showed a diffuse alteration of bilateral glandular echostructure (larger right) with heterogeneous echogenicity echostructure no collections formed by multiple hypoechoic nodular formations (Figure 1). Increased vascularization right parotid and laterocervical lymphadenopathy (Figure 2).
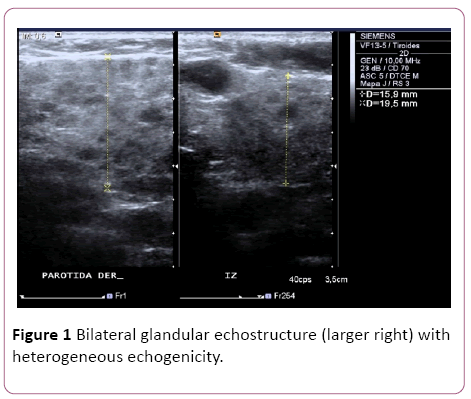
Figure 1: Bilateral glandular echostructure (larger right) with heterogeneous echogenicity.
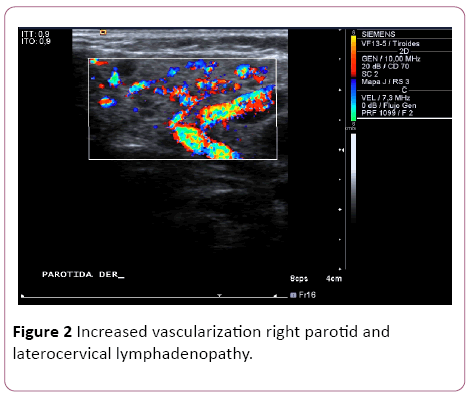
Figure 2: Increased vascularization right parotid and laterocervical lymphadenopathy.
Analytical study including blood count, C-reactive protein (which was the only high value 5.9 mg/L (0-5)), biochemistry, erythrocyte sedimentation rate, electrolytes, glucose, immunoglobulins and serological survey was conducted against Cytomegalovirus (CMV), Human Immunodeficiency Virus (HIV), Epstein-Barr Virus (EBV), all results being within the normal range.
The patient received outpatient treatment with antiinflammatory with very good performance and picture resolution in 5 days. At present it has no new episodes for more than a year ago.
Discussion
Juvenile chronic recurrent parotitis is characterized by nonspecific sialoadenitis recurrent episodes of edema of the parotid glands. The first episode typically occurs between the first and second years, in most cases it is not diagnosed; unnoticed or confused with otitis, parotitis or pharyngitis.
The etiology is not simple [1,2], have been postulated as factors ductal birth defects, genetic factors, allergies, bacterial or viral infections, autoimmune diseases and immunodeficiencies.
The main diagnosis should be done diferencial [3] and bacterial epidemic mumps, the parotid duct stones, tumors of the gland and systemic diseases (syndrome Heerfordt, Mikulick syndrome, Sjögren's syndrome). Also they included in the differential diagnosis viral infections (CMV, EBV, HIV), diabetes mellitus or cystic fibrosis.
The diagnosis [4] is clinical and is usually carried out after the third or fourth episodes due to recurrent history of clinical symptoms. There is no clear consensus about the test, traditionally had considered sialografía [5] main imaging study. The sialographic findings show a dilated acinar sialectasias system as "fruit tree" 1 mm to 2 mm. This test involves a great difficulty for implementation in children, in addition to the use of ionizing radiation.
Recent studies [6] conclude that ultrasonography is the test of choice for the diagnosis and monitoring. The typical ultrasound shows a hypoechoic image with multiple hypodense, vacuoles and dilated Stenon [7] areas.
The involvement is unilateral in most episodes, with a predominance of males. The natural history tends to spontaneous remission during the pubertal period, but may persist into adulthood episodes. Recent studies [8] suggest that juvenile recurrent acute exacerbations Parotitis based on a slowly progressive destruction of the gland is producing.
The aim terapéutico [9] the acute phase is to relieve symptoms and prevent damage to the glandular parenchyma. Usually sufficient treatment with analgesic, anti-inflammatory, heat and massage. If signs of bacterial infection antibiotic treatment was associated. Although there is no evidence, some authors [10] point to the possibility that antibiotic therapy shorten the symptoms and decrease the damage of the pancreas, but the prophylactic treatment of future episodes shown antibiotic ineffective.
Endoscopy of the salivary gland is a relatively new diagnostic and therapeutic technique. The first flexible sialoendoscopia was described in 1993 and shortly after the 1994 rigid sialoendoscopia described. According to the work of Ramakrishna [11] systematic review of the use of sialoendoscopia in PRJ, ductal diameter is not significantly different in pediatric patients, so it would be possible to carry out interventions and direct ductal display at any age.
Schneider [7] work valued in a retrospective comparison of differences between sialoendoscopia and conservative treatment in JPR. Although it concludes that both options are valid shows the potential benefits of endoscopy salivary gland because it is a good diagnostic tool may also have therapeutic effects during non-acute phase of JPR.
The current literature states that are performing well in the treatment of JPR with the application of corticosteroids by sialoendoscopia (in most studies the dose used is 100 mg hydrocortisone) [12]. Roby [13] in a retrospective study compares the sialoendoscopia in which corticosteroids were applied with the direct administration of corticosteroids in parotid duct. The study concludes that the application of corticosteroids ductal sialoendoscopia level not causing the improvement in symptoms, so the sialoendoscopia be reserved for rule changes parotid duct.
Despite these recent studies the controversy regarding the sialoendoscopia in JPR remains as indicated Schneider concluding that greater number of prospective trials with longer follow-up and larger sample size to solve the paradigm is needed that today remains the choice of treatment.
Summary
Juvenile recurrent Parotitis is a rare condition whose diagnosis often goes unnoticed. The aim of this paper is to review the clinical symptoms and the effectiveness and safety of current treatments, all to avoid reducing the functionality of the gland.
We report the case of a patient from which conducted the search of the current literature.
The review concludes that there are no statistically significant differences between conservative treatment and sialoendoscopia. The latter may reserve to rule and treat abnormal parotid duct. Another therapeutic option is the application of corticosteroids ductal level, which is minimally invasive and gets good clinical results.
Despite these recent studies larger number of prospective trials with larger sample number and greater long-term monitoring are still needed
17933
References
- Katz P, Hartl DM, Guerre A (2009) Treatment of juvenile recurrent parotitis. Otolaryngolclin North Am 42: 1087-1091.
- Morales-Bozo I, Urzúa-Orellana B, Landaeta M, Montalbán R (2007) Molecular alterations of parotid saliva in infantile chronic recurrent parotitis. Pediatr Res 61: 203-208.
- González Benavides A, Vaquero Íñigo I, MendizábalDíez M, Martínez Merino M, Herranz Aguirre M (2015) Juvenile Recurrent Chronic Parotiditis. Rev Pediatr Aten Primaria17: 147-149.
- Tapia Ceballos L, Del Río Camacho G, Picazoangelín B, Ruiz Moreno JA, Badaraco M (2004) Parotiditisrecurrente. An Pediatr (Barc) 60:85-86.
- ConcheiroGuisán A, BellverCastañón E, Garrido Romero R (2000) Juvenile Recurrent Chronic Parotiditis. An Esp Pediatr 53:418-421.
- Shimizu M, Umuler J, Donath K, Yoshiura K, Ban S, et al. (1998) Sonographic analysis of recurrent parotitis in children: A comparative study with sialographic findings. M. Oral Surg Oral Med Oral Pathol Oral Radiol Endod86:606-615.
- Schneider H, Koch M, Künzel J, Guillespie MB, Grundtner P, et al. (2014) Juvenile recurrent parotitis: A retrospective comparison of sialendoscopy versus conservative therapy. Laryngoscope 124:451-455.
- Huisman T, Holzmann D, Nadal D (2001) MRI of chronic recurrent parotitis in childhood. J Comput Assist Tomogr 25:269-273.
- Chrite VV, Premchandra DJ (1997) Recurrent parotitis. Arch Dis Child 77:359-363.
- Adeboye SO, Macleod I (2014) Recurrent parotitis of childhood or juvenile recurrent parotitis:A review and report of two cases. Dent Update 41:73-76.
- Ramakrishna J, Strychowsky J, Gupta M, Sommer DD (2015)Sialendoscopy for the management of juvenile recurrent parotitis: A systematic review and meta-analysis. Laryngoscope 125:1472-1479.
- Capaccio P, Sigismund PE, Luca N, Marchisio P, Pignataro L (2012) Modern management of juvenile recurrent parotitis. J LaryngolOtol12:1254-1260.
- Roby BB, Mattingly J, Jensen EL, Gao D, Chan KH (2015) Treatment of juvenile recurrent parotitis of childhood. An analysis of effectiveness. JAMA Otolaryngol Head Neck Surg 141: 126-129.