Keywords
Lifestyle; Tendinopathy; Treatment; Risk factors; Physical therapy
Introduction
Tendinopathy is an overuse injury of tendons [1]. It occurs frequently in athletes, as 30 to 50 percent of injuries in sports are tendon injuries [1,2]. Athletes participating in a variety of sports are at risk of developing tendinopathy [2]. However, not only athletes suffer from tendinopathy. In a general population, researchers found an incidence rate of 10.52 per 1000 persons per year and a prevalence rate of 11.83 per 1000 persons per year [3]. Physical therapists and other therapists often treat patients with tendinopathy in their daily practice [4]. Tendinopathy has a negative impact on quality of life, work ability and social and sports participation, and it is known for its poor prognosis [3]. Pain, loss in function and structural changes may occur in both upper and lower extremities, which tends to result in incapacity to repeatedly load the tendon [4]. In tendinopathy, the tendonbone attachment is more frequently affected than the mid-tendon [4].While structural changes in tendons are not considered key factors in tendinopathy [4,5], pain and loss in function are important to address [4,5].
Recovery of tendinopathy is on average slow and tendinopathy is difficult to treat [3,6]. Among the multiple treatment options that are described in the scientific literature, load management and slowly progressing exercise programs are generally considered the best methods to treat pain and loss in function [1,6]. A combination of eccentric exercises, isometric exercises, heavy slow resistance training, plyometric exercises and flywheel training can be used [7-9]. Empirical research has found that observable structural changes in tendons are not an explanation for how tendons respond to exercises [4,5]. In addition to exercises and loading modifications, intrinsic factors, which have be found to be risk factors for tendinopathy, such as genes, age, body composition and co-morbidities can play a role in the treatment of tendinopathy [4,10].
Lifestyle factors, which are health-related behaviours or the potential results of such behaviours [11], have also been found to be risk factors for tendinopathy [4,6,10,11]. The purpose of this clinical commentary is to inform physical therapists and other therapists about the role of lifestyle factors both as risk factors and as treatment options in tendinopathy. To this end, lifestyle factors associated with tendinopathy as well as treatment options to modify lifestyle and thereby impact tendon recovery are discussed.
Lifestyle factors as risk factors for tendinopathy
Lifestyle comprises health-related behaviours and their consequences [11]. One can think of behaviours like general activity levels, sleep, nutrition, smoking, alcohol use, and stressrelated behaviour. Unhealthy lifestyle behaviours are associated with a variety of negative outcomes, such as chronic pain, lowgrade inflammation, elevated adiposity, higher waist-to-rib ratio, greater body mass index, overweight, obesity, high cholesterol, metabolic syndrome, diabetes type II, rheumatoid arthritis and inflammatory-related diseases [2,3,6,12-18]. There are guidelines to inform people about a healthy lifestyle [15]. International guidelines agree about the importance of daily movement and recommend 150 minutes of moderate intense movement per week [15]. Moreover, a diet rich in vegetables, fruit, fish and whole-grains fits best in a healthy lifestyle [15]. Recommendations about sleep and psychosocial factors are relatively limited [15]. Nevertheless, experts describe good sleep quality as feeling rested in the morning without having been awake for more than 30 minutes during the night, and good sleep quantity is defined as 7 to 10 hours a night [11]. Stress as a psychological factor is difficult to assess objectively, yet high and chronic stress levels are not recommended [11]. Health guidelines advice against any smoking and alcohol use is only advised in moderation (i.e., not more than 5 glasses a week and not more than 2 glasses a day) [15]. Failure to meet these healthy lifestyle criteria is likely to result in higher risk of developing tendinopathy [2,3,6].
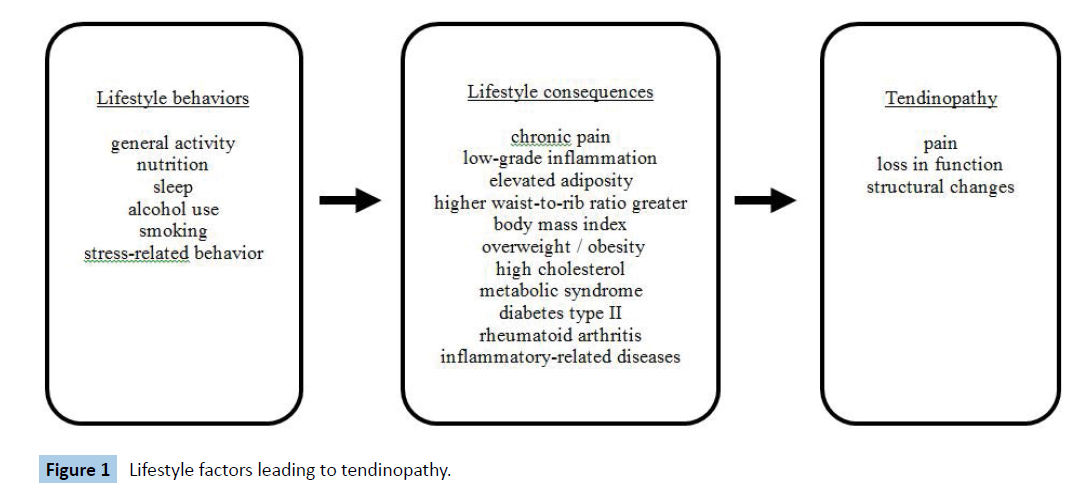
One can distinguish between intrinsic and extrinsic risk factors for tendinopathy, for upper and lower extremity tendinopathy and in both athletes and inactive persons [6]. Extrinsic risk factors for tendinopathy are general activity levels, changes in loading, footwear and training surface [6]. Intrinsic risk factors for tendinopathy are previous limb injury, recent injury of any type, older age (>30 years), gender (women), higher waist-to-rib ratio, greater body mass index, overweight, obesity, lower muscle power, lower muscle strength, lower muscle endurance, reduced ankle dorsiflexion, foot pronation, improper foot alignment, steroid exposure, antibiotic treatment, diabetes mellitus, high cholesterol and rheumatological disease [2,3,6,10-13,18]. While some risk factors are difficult to influence, most lifestyle-related risk factors are modifiable [6]. Among lifestyle-related risk factors for tendinopathy are first of all lifestyle behaviours such as general activity levels, nutrition, sleep, alcohol use, smoking and stressrelated behaviour. Secondly, consequences of an unhealthy lifestyle are also risk factors for tendinopathy, including chronic pain, low-grade inflammation, elevated adiposity, higher waistto- rib ratio, greater body mass index, overweight, obesity, high cholesterol, metabolic syndrome, diabetes type II, rheumatoid arthritis and inflammatory-related diseases [2,3,6,10,12-14,18]. Especially overweight and obesity play an important role in tendinopathy because of the increased load on tendons in overweight and obese people and because of an increase in lipocytes and free fatty acids and higher cholesterol levels and an increased metabolic activity of pro-inflammatory cytokines (e.g. interleukin-6, tumor necrosis factor alpha and C-reactive protein) released by adipose tissue [3,14,19,20]. Figure 1 shows how lifestyle factors are related and can lead to tendinopathy.
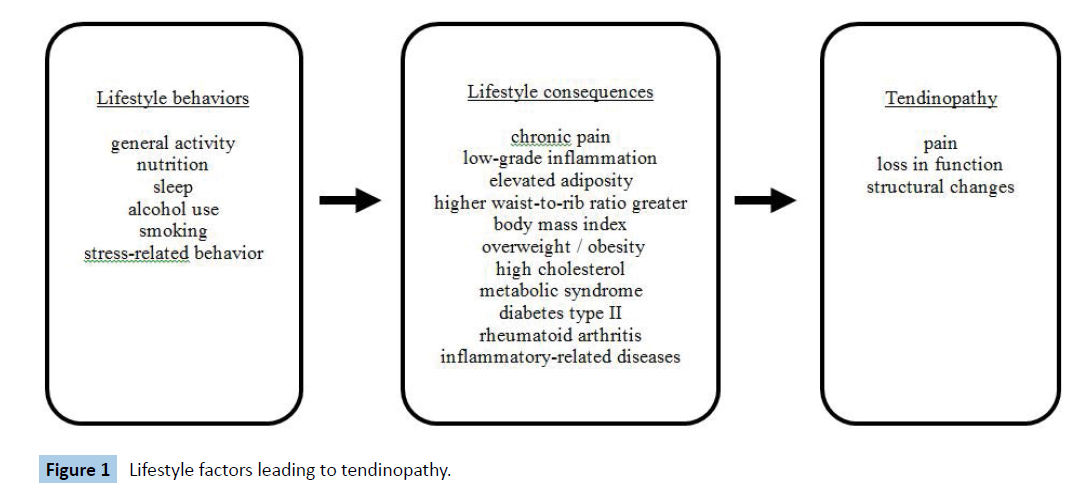
Figure 1: Lifestyle factors leading to tendinopathy.
The role of lifestyle factors in treating tendinopathy
Unhealthy lifestyle factors place a person not only at higher risk for developing tendinopathy but also influence pain, recovery and tendon healing [11,20]. After assessing a patient’s lifestyle, physical therapists and other therapists can target lifestyle factors in the treatment of tendinopathy. Physical therapists and other therapists have a role in advising and coaching a patient towards a healthy lifestyle in line with international guidelines [15] and they can opt for interventions targeting a single lifestyle factor or choose combined intervention programs that target multiple lifestyle factors [21,22]. Combined lifestyle interventions are effective in reducing body weight and improving dietary habits leading to reduced incidence of metabolic diseases such as the metabolic syndrome and diabetes type II [21]. These interventions involve coaching regarding physical activity, dietary behaviours sleep and stress [21]. Other lifestyle factors such as alcohol use, smoking behaviour and psychosocial factors can also be targeted in a combined lifestyle intervention. In what comes next, specific treatment options per lifestyle factor are discussed, which can be implemented as single or combined lifestyle interventions.
First of all, exercise and movement are common therapeutic interventions and can effectively be used for tendinopathy patients who experience the negative consequences of an unhealthy lifestyle, such as elevated adiposity, obesity or diabetes type II [23]. However, a concern is that these persons have a higher risk for developing tendon injuries when they start moving more [20]. Exercises and movement as medicine should therefore be prescribed carefully [23]. That is, patients with elevated adiposity, overweight, obesity and/or diabetes type II should be guided individually during exercises and movement [23]. Importantly, tendinopathy patients with a healthy weight and without diabetes or metabolic syndrome can also lack daily movement, especially if they are injured, and should also be advised to move and exercise more. Injured athletes who cannot perform their sports should be encouraged to do other forms of movement or exercise [4,8]. Fear of injury and lack of motivation and time are some of the barriers to be more physically active [23]. In particular when these barriers are present, individually guided behavioural interventions are more effective than remote or group interventions and cognitive interventions. Behavioural interventions are for example goal setting, contracting, selfmonitoring, cues and rewards [23]. Examples of cognitive interventions - although less effective - are decision making, health education and provision of information [23].
Second, nutritional interventions have recently been suggested as treatment of chronic pain and can therefore help tendinopathy patients since they often experience chronic pain [24,25]. Researchers have also concluded that nutrition may influence the metabolism of tendons and that it can be used as an intervention for tendinopathy [24]. Examples of nutritional interventions are a low-saturated fat and low-added sugar diet and plant-based diets [16,25]. When treating tendinopathy patients with elevated adiposity, overweight, obesity and/or diabetes type II, nutritional interventions and dietary changes can influence adiposity, weight, low-grade inflammation and diabetes and thereby influence tendinopathy [11,16,20]. Nutritional interventions in combination with other lifestyle changes, such as more exercise and movement, are more effective than nutritional interventions alone [21]. Specific nutrition as a solo intervention can nonetheless have a positive influence on tendon recovery. Nutritional interventions that improve tendon health and aid tendinopathy recovery are vitamin C-enriched gelatine, glycine, green tea in combination with glycine and a combination of spirulina, glucosamine sulphate, ginseng, selenium, sillicium, iron, vitamin E and zinc [26-29]. Vitamin C-enriched gelatine is proven to improve collagen synthesis and can thereby play an important role in the recovery of tendinopathy [26]. Glycine alone and glycine in combination with green tea result in a higher concentration of collagen components (i.e., hydroxproline, glycosaminoglycans and matrix metalloproteinases) and higher birefringence, ultimately leading to a better organization of collagen fibres of tendons [27,28]. A combination of spirulina, glucosamine sulphate, ginseng, selenium, sillicium, iron, vitamin E and zinc have anti-inflammatory effects on tendon cells, which results in improved recovery of tendinopathy [29]. Another combination of nutrition’s that has been found to have a significant effect on tendon healing consists of protein, amino acids (leucine, arginine and glutamine), vitamin C, vitamin D, manganese, copper, zinc and phytochemicals [32]. Research suggests that nutritional interventions involving a combination of nutrition’s may be more effective than single nutrient interventions [30-32]. Research also suggests the intake of omega-3 and antioxidants in the treatment of tendinopathy [33]. All these nutritional components can be recommended to a tendinopathy patient, either as supplements or via specific nutrition.
Nutritional interventions can also improve tendinopathy-related symptoms such as reduced muscle strength, bone problems, pain and low-grade inflammation. Extra protein and vitamin D intake improve muscle and bone health [16,30], while vegan, vegetarian and Mediterranean diets decrease pain. Chronic pain is related to a higher intake of added sugar and saturated fat and to a lower intake of macronutrients (protein, lipids, carbohydrates), calcium, folic acid, folate, selenium zinc, magnesium, vitamin A, vitamin K and vitamin B6 [16,25]. Diet patterns (e.g. Mediterranean diet), whole foods (e.g. blueberries), specific bioactive nutrients (e.g. fibers), fatty acids (e.g. omega-3) and polyphenols can all lower low-grade inflammation markers [31].
As a third type of lifestyle intervention, sleep coaching can have an influence on tendon recovery. Lower sleep quality increases the risk of tendinopathy and is a risk factor for the onset and persistence of chronic pain, which is a symptom of tendinopathy [32-34]. Pain modulation occurs mainly during sleep and it is therefore recommended to address sleeping problems as part of the treatment of chronic pain related to tendinopathy [11]. Moreover, recovery of tissue like tendons is dependent on the quantity and quality of sleep [35]. Because adrenaline and cortisol levels are low during hours of sleep, cells divide more easily and growth hormones are released [34]. Growth hormones are endocrine anabolic hormones that increase protein synthesis [34]. Cell division and protein synthesis are important precursors of tissue healing and thereby aid in recovery of tendinopathy [34]. Another precursor of tissue healing is low-grade inflammation, which is increased by disturbed sleep [36,37]. Sleep interventions can focus on providing education on the relationship between sleep and tendinopathy (and other health outcomes), coaching in sleep hygiene, providing an exercise program and giving advice about sleep positioning and bed mobility [35].
Fourth, psychosocial interventions should be considered if the patient with tendinopathy has psychosocial problems. Having an injury like tendinopathy -which is known for its poor prognosis, long recovery time and impact on daily function and social and sports participation — can be an stressor in and of itself [36,37]. Although studies on psychosocial factors as risk factors for tendinopathy are scant [6,18], psychological distress has been associated with sports injuries such as tendinopathy [36]. Distress is known to hinder tissue healing because cortisol and pro-inflammatory cytokines are released during distress, affecting the healing process [37]. Moreover, people with higher distress often have less healthy lifestyle behaviours reflected in their diet, sleep, exercise, smoking and alcohol use [37]. Patients with tendinopathy can therefore find themselves in a vicious spiral of pain, distress, unhealthy lifestyle and impaired healing. Psychosocial interventions can be used to effectively address factors such as distress and to help patients get out of the vicious spiral. Psychological factors such as anxiety, depression and catastrophizing beliefs are associated with the onset and persistence of chronic pain, poorer prognosis of pain conditions like tendinopathy and impaired healing of body tissue [11,37]. Research has also shown that lack of co-worker and supervisor support is a risk factor for shoulder tendinopathy [13]. Interventions can therefore focus on prescribing exercises, stress management, relaxation and social support [21,22,37].
Finally, interventions regarding smoking behaviour and alcohol use are available for patients with tendinopathy. Alcohol impairs tissue healing because of negative changes in cell division, delayed collagen synthesis and cardiac and immune dysfunction, and tissue healing is slower in smokers than in non-smokers because of the toxins in cigarette smoke, which impair peripheral oxygen supply and collagen proliferation [37]. Physical therapists and other therapists can educate advice and/or coach a patient with tendinopathy about the effects of alcohol and smoking on their recovery [22]. In collaboration with the patient’s physician, they can be recommended to start an alcohol or smoking cessation program [22].
Importantly, most lifestyle factors are interrelated. Lack of physical activity and daily movement are for example not only associated with overweight but also with poorer sleep quantity and quality [21,23]. Similarly, nutrition, sleep and psychological distress are closely related [11]. In fact, the lifestyle factors discussed in this article all have a reciprocal relationship with each other [21]. The implication is that improving a single lifestyle factor can have cascading events. For instance, more movement and exercise will be effective for the tendon itself (in terms of better structure, less pain and less dysfunction) but also holistically affect one’s physical and mental health, thereby influencing tendinopathy (in terms of less pain, improved neuroplasticity, better cognitive function, better blood levels, less adiposity and lower low-grade inflammation) [5,8,11,23-37].
Discussion and Conclusion
Multiple lifestyle factors have been found to be risk factors for tendinopathy. Unhealthy lifestyle factors can cause chronic pain, low-grade inflammation, elevated adiposity, higher waistto- rib ratio, greater body mass index, overweight, obesity, high cholesterol, metabolic syndrome, diabetes type II, rheumatoid arthritis and inflammatory-related diseases, which are the main factors explaining the association between lifestyle factors and tendinopathy. This article has discussed the lifestyle factors of exercise and movement, nutrition, sleep and psychosocial factors and how they are often interrelated and can create a vicious spiral for patients with tendinopathy.
Single or combined lifestyle interventions can be considered in the treatment of patients with tendinopathy. Exercise and nnutritional interventions can improve tendon health and recovery of tendinopathy, both indirectly - by decreasing adiposity, weight, diabetic symptoms and low-grade inflammation and by increasing blood, bone and muscle health - and directly by improving collagen synthesis of tendons, tendon function and tendon-related pain. Sleep and psychosocial factors also affect tendon pain and tissue healing. Physical therapists and other therapists can apply lifestyle interventions to improve sleep and positively affect psychosocial factors as part of the treatment of tendinopathy. Finally, smoking behavior and alcohol use negatively affect tendon recovery and should therefore be discouraged to improve tendon recovery.
37574
References
- Lorenz D, Reiman M (2011) The role and implementation of eccentric training in athletic rehabilitation: tendinopathy, hamstring strains and acl reconstruction. Int J Sports Phys Ther 6: 27-44.
- Goes RA, Lopes LR, Cossich VRA, de Miranda VAR (2020) Musculoskeletal injuries in athletes from five modalities: a cross-sectional study. BMC Musculoskel Disord 21: 1-9.
- Albers IS, Zwerver J, Diercks RL, Dekker JH (2016) Incidence and prevalence of lower extremity tendinopathy in a Dutch general practice population: A cross sectional study. BMC Musculoskel Disord 17: 1-6.
- Cook JL, Purdam CR (2009) Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med 43: 409-416.
- Drew BT, Smith TO, Littlewood C, Sturrock B (2012) Do structural changers (eg, collagen/matrix) explain the response to therapeutic exercises in tendinopathy: A systematic review. Br J Sports Med 48: 966-972.
- O’Neill S, Watson PJ, Barry S (2016) A delphi study of risk factors for achilles tendinopathy - opinions of world tendon experts. Int J Sports Phys Ther 11: 684-697.
- Escrische-Escuder A, Casan J, Cuesta-Vargas AI (2019) Progression criteria in loading exercise programmes in lower limb tendinopathy: A protocol for a systematic review and meta-analysis. BMJ Open 9: 1-5.
- Cardosa TB, Pizzari T, Kinsella R, Hope D (2019) Current trends in tendinopathy management. Best Pract Res Clin Rheumatol 33: 122-140.
- Wonders J (2019) Flywheel training in musculoskeletal rehabilitation: A clinical commentary. Int J Sports Phys Ther 14: 994-1000.
- Loiacona C, Palermi S, Massa B, Belviso I (2019) Tendinopathy: Pathophysiology, Therapeutic Options, and Role of Nutraceutics. A Narrative Literature Review. Medicina 55: 1-12.
- Hecke O, Torrance N, Smith BH (2013) Chronic pain epidemiology -where do lifestyle factors fit in? Br J Pain 7: 209-217.
- Del Buono A, Battery L, Denaro V, Maccuaro G (2011) Tendinopathy and inflammation: some truths. Int. J. Immunopathol. Pharmacol 24: 45-50.
- Werner RA, Franzblau A, Gell N, Ulin SS (2005) A Longitudinal Study of Industrial and Clerical Workers: Predictors of Upper Extremity Tendonitis. J Occup Rehabil 15: 37-46.
- Gaida JE, Ashe MC, Bass SL, Cook JJ (2009) Is adiposity an under-recognized risk factor for tendinopathy? A systematic review. Arthritis Rheum 61: 840-849.
- Khanji MY, van Waardhuizen CN, Cicalho VVS, Ferket BS (2018) Lifestyle advice and interventions for cardiovascular risk reduction: A systematic review of guidelines. Int J Cardiol 264: 142-151.
- Elma Ö, Yilmaz ST, Deliens T, Coppetiers I (2020) Do nutritional factors interact with chronic musculoskeletal pain? A systematic review. J Clin Med 9:702-725.
- Norde MM, Fisberg RM, Marchioni DML, Rogero MM (2020) Systemic low-grade inflammation associated lifestyle, diet, and genetic factors: A population-based cross-sectional study. Nutrition 70: 1-6.
- Worp H, Ark M, Roerink S, Pepping GJ (2012) Risk factors for patellar tendinopathy: a systematic review of the literature. Br J Sports Med 45: 446-452.
- Gaida JE, Cook JL, & Bass SL (2008) Adiposity and tendinopathy. Disabil Rehabil 30: 1555-1562.
- Scott A, Zwerver J, Grewal N, De Sa A (2015) Lipids, adiposity and tendinopathy: is there a mechanistic link? Critical review. Br J Sports Med 49: 984-988.
- Rinsum C van, Gerards S, Rutten G, Phillipens N (2018) The Coaching on Lifestyle (CooL) intervention for overweight and obesity: a longitudinal study into participants’ lifestyle changes. Int J Environ Res Public Health 15: 680-707.
- Dean E (2009) Physical Therapy in the 21st Century (Part I): Toward Practice Informed by Epidemiology and the Crisis of Lifestyle Conditions. Physiother Therapy Pract 25: 330-335.
- Crooke R, Haseler C, Haseler T, Collins J (2020) Physical activity and moving more for health. R Coll Physicians Edinb 50: 173-180.
- Scott A and Nordin C (2016) Do dietary factors influence tendon metabolism? Adv Exp Med Biol 920: 283-289.
- Nijs J, Yilmaz ST, Elma Ö (2020) Nutritional intervention in chronic pain: An innovative way of targeting central nervous system sensitization? Expert Opin Ther Targets 28: 1-11.
- Shaw G, Lee-Barthel A, Ross MLR, Wang B (2017) Vitamin C-enriched gelatin supplementation before intermittent activity augments collagen synthesis. Am J Clin Nutr 105: 136-143.
- Viera CP, De Oliveira LP, Da Ré Guerra F, Almeida MS (2015) Glycine improves biochemical and biomechanical properties following inflammation of the achilles tendon. Anat Rec298: 538-545.
- Viera CP, Da Ré Guerra F, de Oliveira LP, Almeida MS (2015) Green tea and glycine aid in the recovery of tendinitis of the Achilles tendon of rats. Connect Tissue Res 56: 50-58.
- Baugé C, Leclerq S, Conrozier T, Boumediene K (2015) TOL19-001 reduces inflammation and MMP expression in monolayer cultures of tendon cells. BMC Complement Altern Med 15: 217-227.
- Mangano KM, Sahni S, Kiel DP, Tucker KL (2017) Dietary protein is associated with musculoskeletal health independently of dietary pattern: The Framingham Third Generation Study. Am J Clin Nutr 105: 714-22.
- Calle MC and Andersoen CJ (2019) Assessment of dietary patterns represents a potential, yet variable, measure of inflammatory status: A review and update. Dis Markers 2019: 1-13.
- Curtis L (2016) Nutritional research may be useful in treating tendon injuries. Nutrition 32: 617-626.
- Lewis JS and Sandfort FM (2009) Rotator cuff tendinopathy: Is there a role for polyunsaturated Fatty acids and antioxidants? J Hand Ther 22: 49-55.
- Siengsukon CF, Al-dughmi M, Stevens S (2017) Sleep health promotion: Practical information for physical therapists. Phys Ther 97: 826-836.
- Laux P, Krumm B, Diers M, Flor H (2015) Recovery-stress balance and injury risk in professional football players: a prospective study. J Sports Sci 33: 2140-2148.
- Christian LM, Graham JE, Padgetta DA, Glasera R (2006) Stress and Wound Healing. Neuroimmunomodulation 13: 337-346.