Diem Kieu Thi Tran1*, Michael Young2,Li-Mei Lin1Frank PK Hsu1
1Department of Neurological Surgery, University of California, Irvine
2Department of Neurology, University of California, Irvine
*Corresponding Author:
Diem Kieu Thi Tran
Department of Neurological Surgery, University of California, Irvine, USA
Tel: 8164472818
E-mail: diemkt@uci.edu
Received Date: June 14, 2015; Accepted Date: July 30, 2015; Published Date: July 31, 2015
Citation: Tran DKT, Young M, Lin L. Limb Hypertrophy and Urinary Retention in Parkes Weber: A Case Report. J Neurol Neurosci. 2016, 6:1. DOI: 10.21767/2171-6625.100015
Keywords
Parkes weber; Spinal avm; Arteriovenous malformation; Limb hypertrophy
Introduction
Vascular malformations are developmental abnormalities of the vascular system, which may involve any part of the vascular tree: arteries, veins, or capillaries. Arteriovenous malformations (AVM) are the most common among these types [1]. High flow arteriovenous malformation lead to shunting of arterial blood into the venous system.
These can cause hemodynamic instability and manifest with arteriolisation with large venous engorgement, organomegaly, or high output cardiac failure.
Parkes weber syndrome usually presents with varicose veins, single limb hypertrophy, and port-wine stain with clinical evidence of AV fistula. Patients with Parkes Weber Syndome can have large ateriovenous malformations that can lead to organomegaly involving usually one of the lower extremities [2]. They can also have associated spinal AVMs that can cause significant compression of the spinal cord, which in turn can lead to lower extremities myelopathies [3]. The presence of arteriovenous (AV) fistulas differentiates this high-flow disorder from Klippel-Trenaunay syndrome (KTS). Once thought to be a purely sporadic disorder, Parkes Weber syndrome with multifocal capillary malformations has been found to be associated with RASA1 mutation [4]. This mutation is has not been seen in KTS.
Case presentation
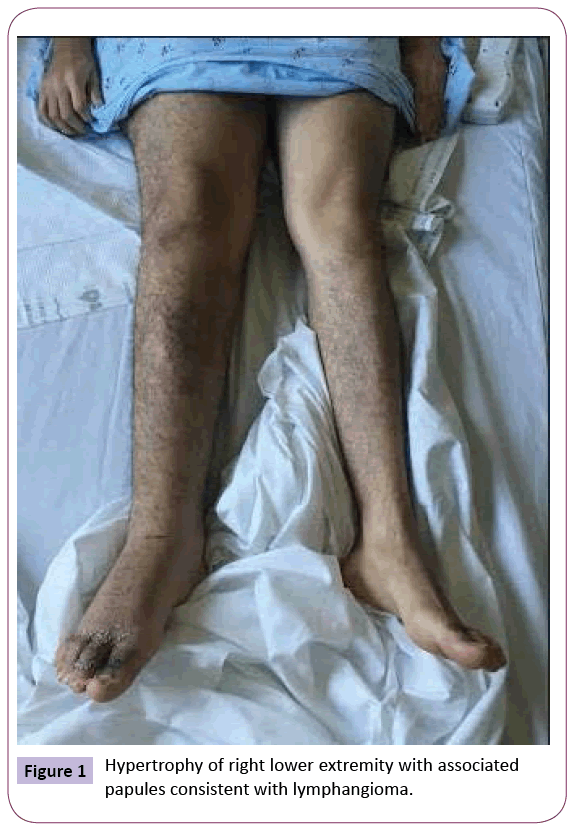
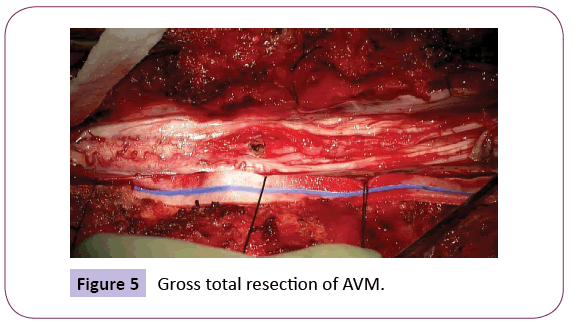
A 21-year-old male patient presented with worsening right lower extremity edema and urinary retention. He reported unprovoked intermittent low back pain that was aggravated prior to presentation by heavy lifting. He also described a shooting pain that radiated down both legs, with left greater than right along with weakness and numbness of his right leg. He stated that his right leg has always been larger compared to the left, but that it became progressively more swollen over the past 3 weeks (Figure 1). Then, over the past week prior to presentation, he developed urinary retention, which worsened over the past couple days, and prompted his visit to the ED. He reported normal bowel movements and denied saddle anesthesia.
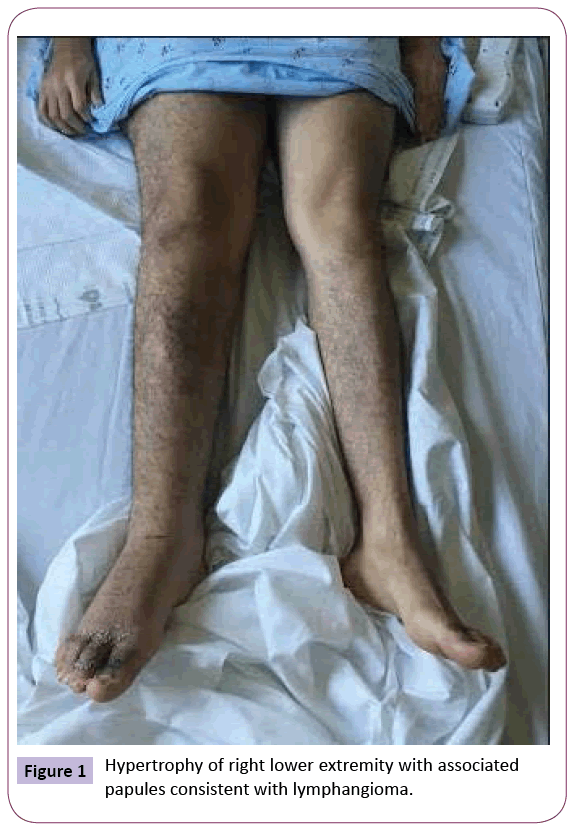
Figure 1: Hypertrophy of right lower extremity with associated papules consistent with lymphangioma.
On examination, his entire right lower extremity was noted to be circumferentially much larger than the left. He had mild right lower extremity weakness in hip flexion, knee flexion, dorsiflexion, and plantar flexion. There was also patchy hypesthesia of the right lower extremity. Additionally, there was a large port wine stain on his right buttocks and varicose veins on his right hip(not pictured). Dermatology evaluated the patient and reported innumerable papules consistent with lymphangioma.
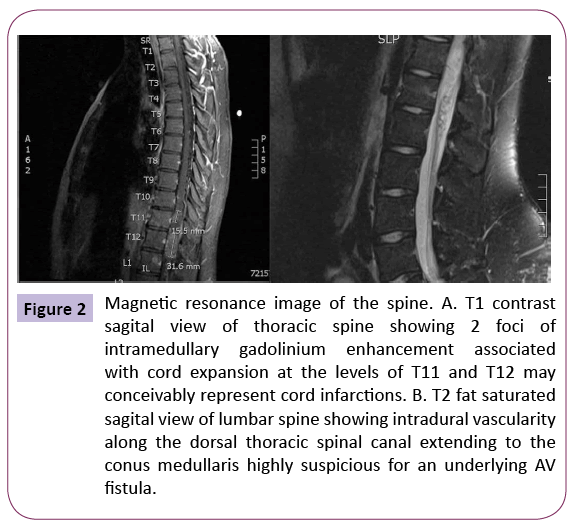
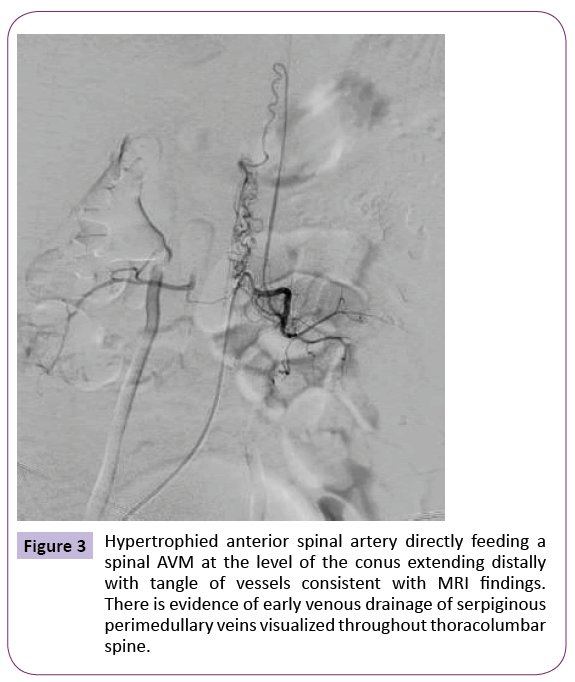
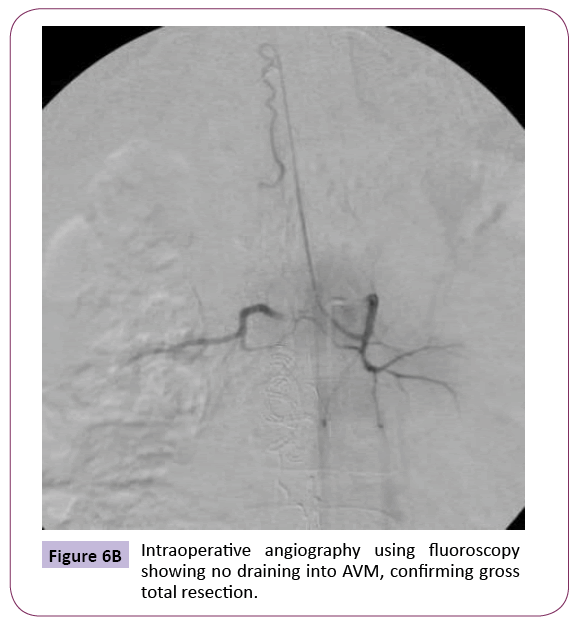
An MRI of the thoracolumbar spine with and without contrast was performed which showed intradural vascularity along the dorsal thoracic spinal canal extending to the conus medullaris highly suspicious for an underlying AV fistula (Figure 2). Because of these findings, he was taken for diagnostic spinal angiography, which demonstrated a conus medullaris spinal arteriovenous malformation (AVM) fed directly by hypertrophied anterior spinal artery that arises from the left L2 lumbar artery with evidence of early venous drainage via serpiginous, prominent perimedullary veins coursing superiorly up the thoracic spine (Figure 3). Because the patient was already symptomatic from this spinal arteriovenous malformation, with evidence of significant spinal cord edema on the MRI, the decision was made to treat the AVM.
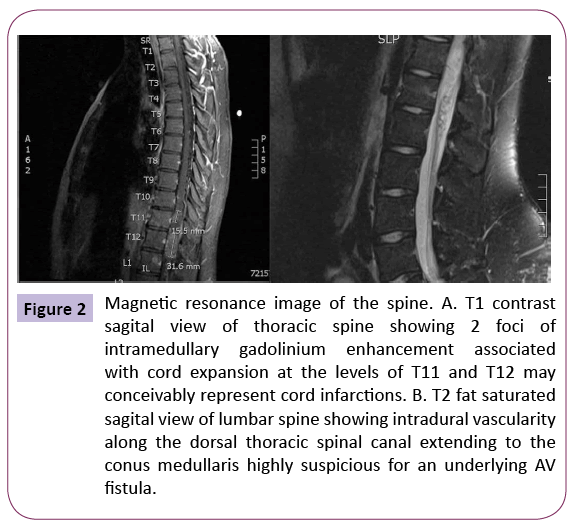
Figure 2: Magnetic resonance image of the spine. A. T1 contrast sagital view of thoracic spine showing 2 foci of intramedullary gadolinium enhancement associated with cord expansion at the levels of T11 and T12 may conceivably represent cord infarctions. B. T2 fat saturated sagital view of lumbar spine showing intradural vascularity along the dorsal thoracic spinal canal extending to the conus medullaris highly suspicious for an underlying AV fistula.
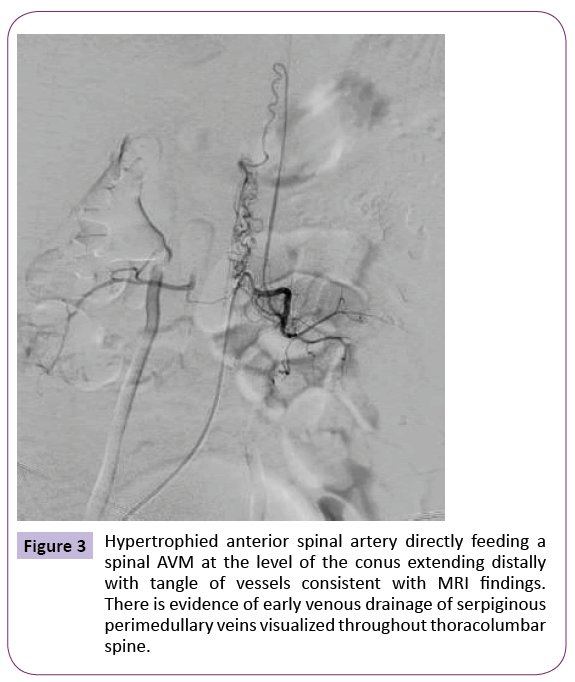
Figure 3: Hypertrophied anterior spinal artery directly feeding a spinal AVM at the level of the conus extending distally with tangle of vessels consistent with MRI findings. There is evidence of early venous drainage of serpiginous perimedullary veins visualized throughout thoracolumbar spine.
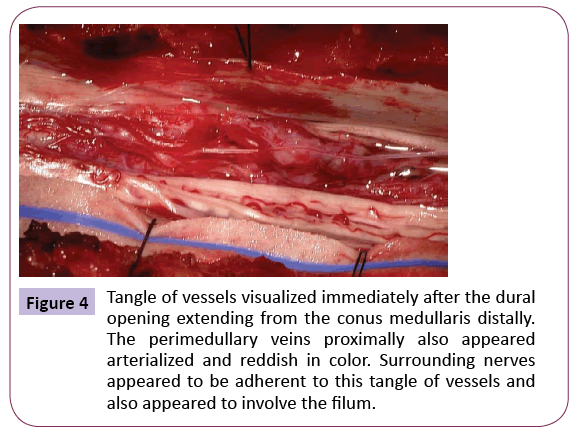
Given that this conus medullaris AVM was fed by a hypertrophied anterior spinal artery, an endovascular approach for treatment was not pursued. An open microsurgical resection was undertaken via a posterior approach to the thoracolumbar spine with bilateral laminoplasty from T11-T12, T12-L1, L1-L2 and L2-L3. Once the laminoplasty was removed exposing the dura, intraoperative ultrasound was then used to confirm presence of underlying spinal AVM. A long midline dural opening was then made. The microscope was subsequently used for the microsurgical dissection and resection of the AVM (Figure 4). After achieving apparent gross total resection of the visualized AVM (Figure 5), intraoperative indocyanide green (ICG) videoangiography was performed to ensure no evidence of early venous drainage (Figure 6A). A subsequent intraoperative spinal angiography was then performed which confirmed complete angiographic obliteration of the spinal AVM (Figure 6B).
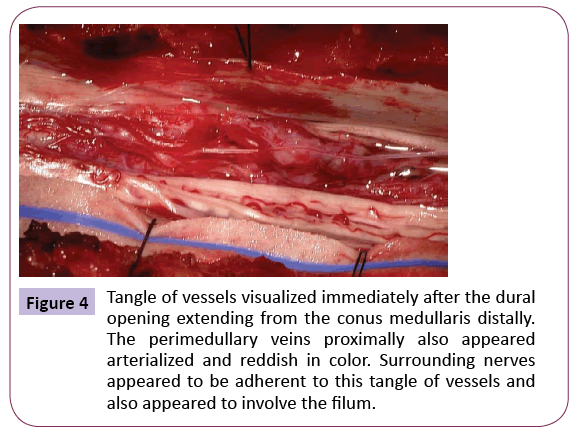
Figure 4: Tangle of vessels visualized immediately after the dural opening extending from the conus medullaris distally. The perimedullary veins proximally also appeared arterialized and reddish in color. Surrounding nerves appeared to be adherent to this tangle of vessels and also appeared to involve the filum.
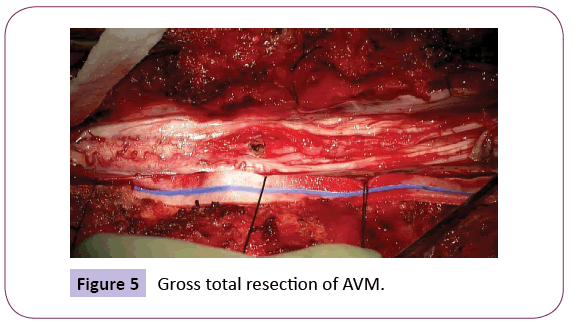
Figure 5: Gross total resection of AVM.

Figure 6A: Intraoperative ICG showing no early venous drainage.
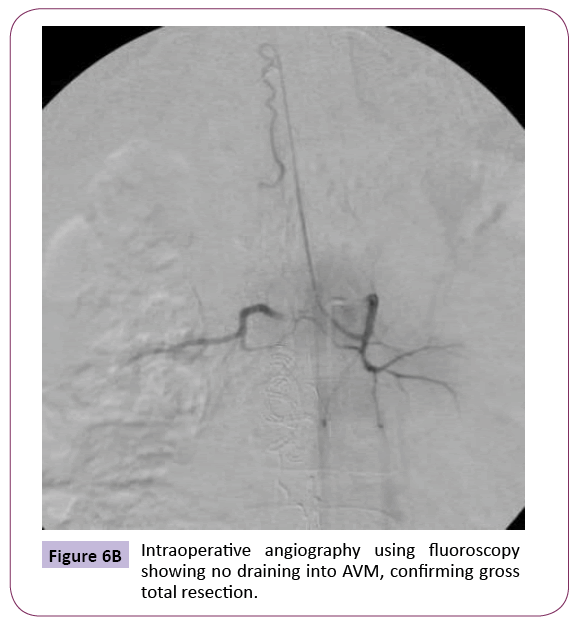
Figure 6B: Intraoperative angiography using fluoroscopy showing no draining into AVM, confirming gross total resection.
Postoperatively, the patient continued to have urinary retention and mild weakness of the right lower extremity, however, slightly
improved by postoperative day four. The patient was discharged to an acute rehab unit postoperative day five. There, he continued to improve with strength, now back to full strength in bilateral lower extremities with minimal urinary retention. The patient was discharged home from acute rehab unit postoperative day fifteen without complications. He was seen in follow up two weeks and again at six weeks post discharge from acute rehab and was found to have full strength and no urinary retention.
Discussion
Parkes weber syndrome was first described in 1907 by a dermatologist, Dr. Fredrick Weber [5]. He reported a syndrome involving proportionate hemi-hypertrophic limb with vascular malformations. At the time, there was no vascular imaging, and vascular malformations were an unknown entity. The syndrome is rare and characterized by high- flow AV fistulas, vascular malformations, and soft tissue and bone hypertrophy [6]. Due to the rarity of the disease, no epidemiological studies have been done and the incidence is unknown. Most cases are sporadic, however they are usually associated with RAS1 gene mutation [7]. Prompt recognition of this rare disorder is essential to the appropriate diagnosis and treatment to prevent further progression of symptoms.
Treatment usually involves repeated endovascular embolism or surgical obliteration of the malformation [4]. The disease, however, is a progressive disease with continued development of AVMs requiring regular follow-ups with repeat imaging. If this syndrome is not caught early enough, it can lead to limb amputation and death from cardiac failure [8].
In our case, the patient’s symptoms may have been prevented had this syndrome been recognized and treated earlier. He may not have progressed to developing urinary retention. While the resection is not curative, it is expected to prevent progression of his myelopathy. Furthermore, prompt recognition will also obviate the need for superfluous imaging and consultations.
Conclusion
In this article, we report a case of Parkes Weber syndrome involving a spinal ateriovenous malformation that required surgical resection. The patient was safely treated with full recovery of lower extremity weakness and resolution of his urinary retention at six weeks postoperative. The patient will continue to follow up with repeat imaging periodically.
6724
References
- Niimi Y, Ito U, Tone O, Yoshida K, Sato S, et al. (1998) “Multiple spinal perimedullaryateriovenous fistulae associated with the Parkes Weber Syndrome.” Interventional Neuroradiology 4: 151-157.
- Garzon MC, Huang JT, Enjolras O, Frieden IJ (2007) Vascular malformations: Part II. J Am AcadDermatol 56:541-564.
- Namba K, Nemoto S (2013) Parkes Weber Syndrome & Spinal Arteriovenous Malformations. American Journal of Neuroradiology 34: E110- E112.
- Girron VO, López GJC, Fernández PI (2003) Diagnosis & Treatment of Parkes Weber Syndrome: A Review of 10 consecutive patients. Annals of Vascular Surgery 6: 820-825.
- Weber FP (1907) "Angioma-formation in connection with hypertrophy of limbs and hemi-hypertrophy". British Journal of Dermatology 19: 231–235.
- Parkes-Weber F: Haemangiectatic hypertrophy of limbs congenital phlebarteriectasis and so-called congenital varicose (1918) Brit J Child Dis 15: 13-23.
- Revencu N, Boon LM, Dompmartin A, Rieu P, Busch WL, et al. (2013) Germline Mutations in RASA1 Are Not Found in Patients with Klippel-Trenaunay Syndrome or Capillary Malformation with Limb Overgrowth. Molecular Syndromology 4: 173-178.
- Manresa-Manresa F (2015) Parkes Weber Syndrome. Images in cardiology 68: 6.