Keywords
Lipedema, lipoedema, lymphedema, lipolymphedema, spheroids
Introduction
Lipedema (lipoedema in Europe) meaning fluid or swelling in fat is a painful disorder involving subcutaneous adipose tissue (SAT). Lipedema was first named in the literature in 1940 by Drs. Allen and Hines as a condition occurring almost exclusively in women who suffer from enlargement of fat tissue of the lower extremities and buttocks [1]; older literature also contains descriptions of women with lipedema [2,3]. In more recent literature, lipedema is described as a bilateral condition that does not affect the hands or feet [4] with a disproportion between a smaller upper body and a “voluminous” lower body [5].
There are three stages of lipedema that refer primarily to changes in the skin [6,7]:
Stage 1 in which there is a normal skin surface with enlarged hypodermal SAT; Stage 2 with indentations of the skin and underlying SAT similar to a mattress [8] containing larger mounds of SAT that grow as non-encapsulated masses, lipomas and angiolipomas; Stage 3 where large extrusions of tissue (skin and SAT) cause gross deformations especially on the thighs and around the knees. Lymphedema, where lymph fluid develops dependently on the feet and hands increasing cranially due to dysfunctional lymphatics, can develop during any stage of lipedema, and is called lipolymphedema or Stage 4 lipedema. Lipedema therefore is a pre-lymphedema condition; though not everyone with lipedema will go on to develop lymphedema.
The authors found in clinical practice that lipedema fat tissue was found more extensively on the body than is currently described in the literature. In addition, women with stage 3 lipedema appeared to have greater and more serious complaints than women with earlier stages of lipedema. The goal of this report was to gain a greater understanding of the extent of lipedema tissue on the body in all stages, and to determine if a later stage of lipedema was associated with a greater number of signs and symptoms suggestive of a serious decline in health.
Methods
Protocol: Chart review from a subspecialty Endocrinology clinic at the University of California, San Diego (UCSD), to which patients self-referred or were formally referred for evaluation and recommendations for treatment, from June 2012 to February 2013. Patients were included in consecutive order if they had or were given a diagnosis of lipedema, had a charted physical exam, and a complete review of systems. This research was considered exempt by the UCSD Human Research and Protection Program.
Fat assessment: Lipedema fat has been astutely described as feeling like small firm beans in a bag [9]. These small, approximately 5 x 5 - 10 x 10 mm “beans”, are rounded fat lobules, distinct from one another yet closely packed together, that resemble spheroids, the buck-shot sized, hard, calcified, subcutaneous nodules resulting from fat necrosis present in connective tissue disorders [10]. In this report, fat on the entire body was assessed qualitatively by visualization as increased, normal or decreased, and by hands-on exam in 29 areas of the body from head to dorsal foot examining for spheroids and lipomas. The breasts were not included in the palpation due to the fibrocystic nature of breast tissue and inability to accurately determine the presence of lipedema tissue. When the beans in a bag feel to the fat was encountered by palpation, the fat was recorded as containing spheroids. The fat on the head can be increased with a sponge-like feel in women with later stages of lipedema and was included in the spheroid analyses.
Pain and joints: Determined by numeric scale as average, high and low pain, with zero being no pain and ten being the worst pain ever. Hypermobile joints were assess using the Beighton hypermobility score [11].
Statistics: A one-way between-subjects ANOVA was used to test for the difference in number of areas with spheroids, size of the fat depot and the number of lipomas based on the patient’s lipedema stage. When appropriate, Tukey HSD post-hoc analyses were used. A Pearson Chi-Square analysis was used to test for the difference in the number of Symptoms in Patient’s Past Medical History and Review of Systems (SPSS, International Business Machines Corporations (IBM; Armonk, NY).
Results
Literature review: In a review of 94 articles found under the search term “lipedema/lipoedema” in PubMed in March 2015, 65 were available with full-text for review, and 49 were available in English. This review focused on articles in English to avoid mistakes in the translation of articles on computergenerated translators. Out of the 42 articles on lipedema, 8 did not mention the distribution of lipedema tissue. The majority of the remaining articles described lipedema fat as occurring almost exclusively on the lower extremities, with occasional involvement of the buttocks and hips [12]. Fife et al. specifically mentioned that lipedema can spread as far up as the lower waist, and down as far as the medial and lateral malleoli and that upper arms can be affected [6]. Cornely stated in a recent paper that the arms are affected in 80% of women with lipedema [13]. Beninson et al. mentioned that trunk and upper extremities are usually normal in patients affected with lipedema [14]. Dietzel et al. found the disproportion between the upper and lower body was lost when obesity was present with lipedema [15]. Combined, these data in the absence of obesity provide a picture of a woman with lipedema whose lipedema SAT can extend as high as her lower abdomen (up to the umbilicus), primarily located on her legs, and upper arms, but not her hands, feet or trunk.
Population characteristics: The majority of the patients in this study had stage 2 lipedema (Table 1) including a single man (age 25 y). Two women with stage 2 lipedema had lipolymphedema (6%) and five women with stage 3 lipedema had lipolymphedema (38.5%), also known as stage 4 lipedema. Body mass index values were available for 46 patients. Four women (8.7%) had normal BMI (<25 kg/m2), three with stage 1 and one with stage 2 lipedema. Seven women (15.2%) were overweight (BMI ≥ 25 ≤ 30 kg/m2, one with stage 2 lipedema and the remainder with stage 3 lipedema; in the latter group, one had stage 4 lipedema. The remainder of the patients, including the man, were obese (76.1%), six of which had stage 4 lipedema.
| Characteristics |
Number |
| Sex M/F |
1/50 |
| Stage 1 |
5 |
| Stage 2 |
33 |
| Stage 3 |
13 |
| Stage 4 |
7 |
| Demographics |
Average ±sem |
| Age (years) |
50 ± 13 |
| Weight (kg) |
103 ± 32 |
| Height (cm) |
165 ± 7 |
| BMI (kg/m2) |
38 ± 12 |
| Age lipedema started (years) |
24 ± 13 |
| Number of children |
1.4 ± 2 |
| Past Medical History |
Percent ±sem |
| Abdominal or pelvic surgery |
48 ± 0.5 |
| Arthritis |
38 ± 0.5 |
| Dyslipidemia |
38 ± 0.5 |
| Hypertension |
31 ± 0.5 |
| Type 2 Diabetes |
2.0 ± 0.1 |
Table 1: Population characteristics, demographics and medical history.
Data on onset of lipedema was available for 41 patients. The median and average age of onset was 20 y and 24.3 ± 2.2 y, respectively. Twenty two (53.7%) stated they developed lipedema by the age of 20 y, eighteen (43.9%)stated they developed lipedema after the age of 20 y, 9.8% after the age of 40 y and only two after the age of 50 years, specifically at 54 y (stage 2) and 63 y (stage 2 and 4).
40% of participants never had children. Sixteen women were multiparous and of these women, two had stage 3 lipedema.
Past Medical and Surgical History: Over 30% of patients had abdominal or pelvic procedures (Table 1). These surgeries included cholecystectomy, loop electrosurgical excision procedure (LEEP), tubal ligation, panniculectomy, Cesarean section, uterine fibroid tumor removal, repeated dilation and curettage (D&C) of the cervix, ovarian cyst removal, or ovarian reconstruction. Over 30% of the patients had arthritis, dyslipidemia or hypertension (Table 1). None of the patients with stage 1 lipedema had hypertension, dyslipidemia or diabetes. Additional past history found in <30% of patients included hypothyroidism (27 ± 0.5%), varicose veins, asthma or hysterectomy (21 ± 0.4% each), fibromyalgia or bariatric surgery (13 ± 0.3% each), and endometriosis (10 ± 0.3%). Less than 10% of the patients had diabetes (Table 1), polycystic ovarian syndrome or gluten allergy (6.3 ± 0.2% each), costochondritis or narcolepsy (4.2 ± 0.2% each), or a factor V Leiden mutation (2.1 ± 0.1%). Of the patients with diabetes, one woman with stage 2 lipedema had type 2 diabetes and one patient had type 1 diabetes. Additionally, three patients had a history of gestational diabetes and two had a history of or had current impaired glucose tolerance for a total of 6 ± 0.3% with insulin resistance or diabetes in their current or past history. The single male had secondary hypogonadism only.
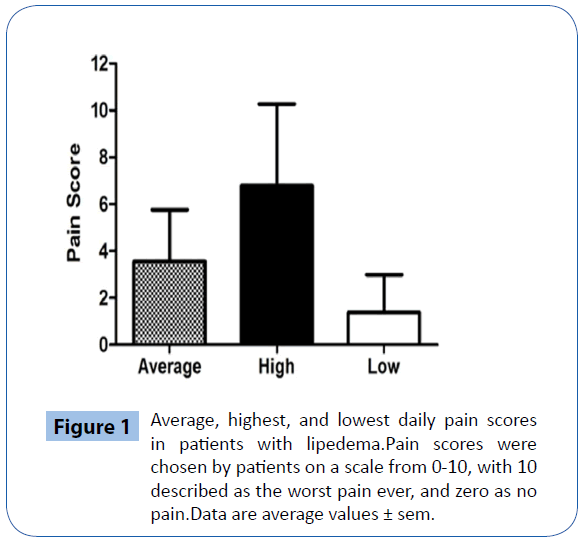
Pain and joints: Data for pain was not available for twelve patients. Four patients with lipedema denied having any pain (10.3%) while the remainder (89.7%) had daily pain (Figure 1). Of the patients that had no pain, one had stage 1, two had stage 2, and one had stage 2 with lipolymphedema. A majority of patients had pain in the joints (57 ± 0.5%), fat (49 ± 0.5%), back (44 ± 0.5%), legs (39 ± 0.5%) and muscle (37 ± 0.5%). Pain was also noted in the head (25 ± 0.4%), arms (25 ± 0.4%), feet (23 ± 0.4%), stomach (16 ± 0.4%), eyes (14 ± 0.4%), and ribs (14 ± 0.4%). The man with lipedema had an average daily pain of 5, with highest pain a 7 and lowest a 2 on a daily basis in his eyes, muscles and joints. There was a trend to difference between the groups in the lowest level of daily pain (P=0.07), but not in the highest daily pain (P=0.88) or average daily pain (P=0.18). The average Beighton score for hypermobile joints among all patients was 4.2 ± 0.5. There was no difference in Beighton scores between groups; the percentage of patients in stage 1, 2 and 3 that had a Beighton score of 5 or more was 40%, 54% and 50%, respectively. There was also no correlation between pain scores and Beighton scores (data not shown).
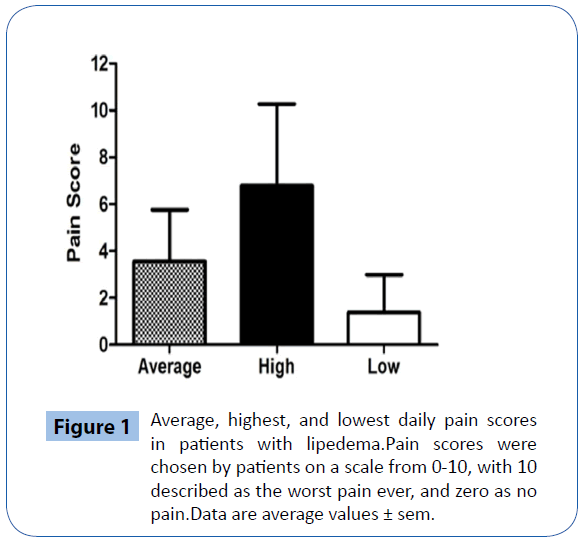
Figure 1: Average, highest, and lowest daily pain scores in patients with lipedema.Pain scores were chosen by patients on a scale from 0-10, with 10 described as the worst pain ever, and zero as no pain.Data are average values ± sem.
Location and type of fat: Fat was noted on physical exam as: 1) Visibly increased in size (amount) from normal; 2) Palpable as small firm spheroids [16]; or 3) Containing lipomas. These three types of fat were compared across the three groups of patients (stages 1, 2, and 3 lipedema). Out of twenty-nine areas assessed for fat size, there was no significant difference (P=0.7) in the average number of enlarged fat depots between stage 1 (3 ± 2.6), stage 2 (3.7 ± 0.5) and stage 3 lipedema (3.9 ± 0.8). No patient had fat atrophy in any area.
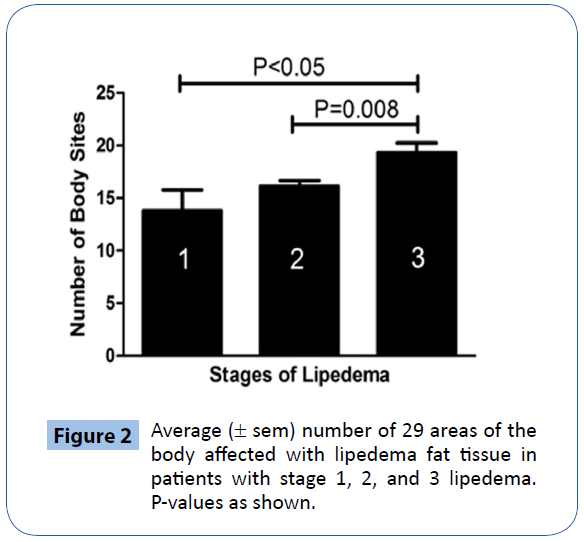
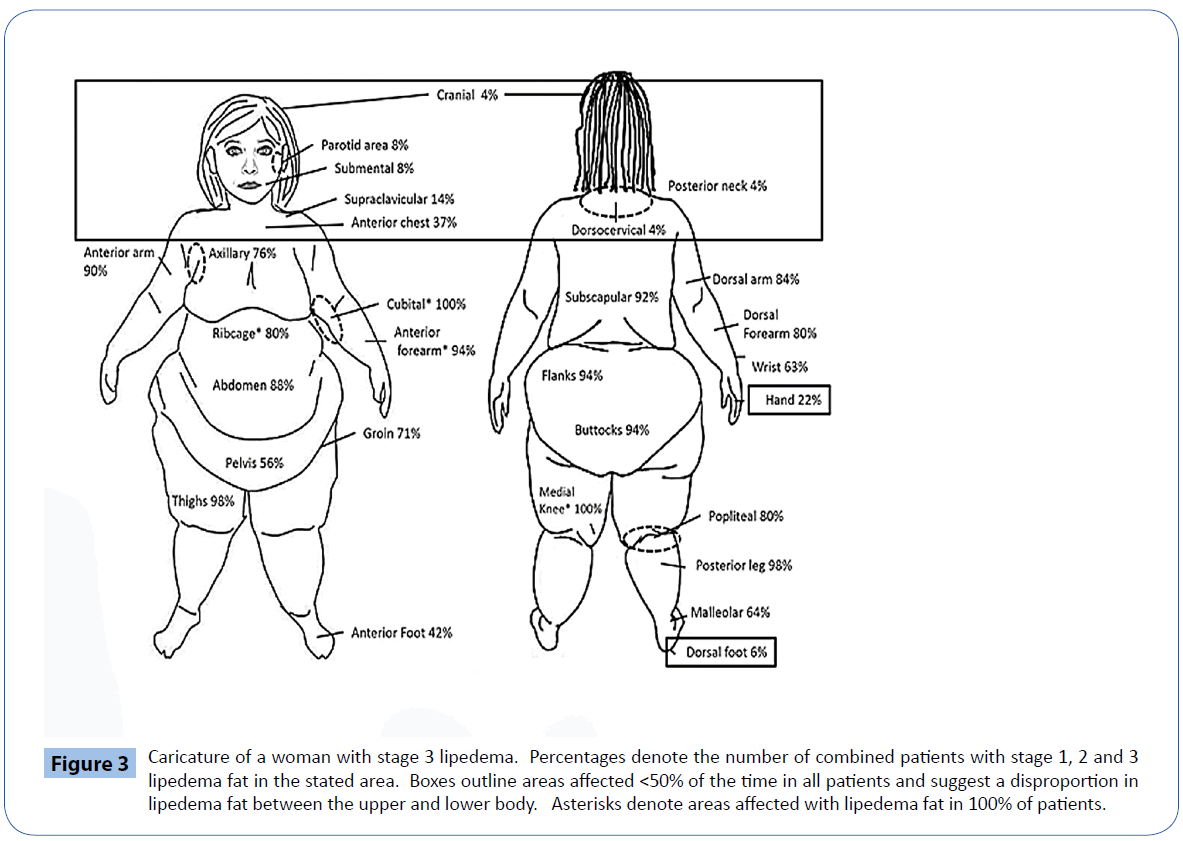
The amount of lipedema tissue containing spheroids differed significantly across the three groups of patients, F (2, 48) = 6.57 (p = 0.003). Tukey post-hoc comparisons of the three groups indicated that the amount of spheroids increased by stage (Figure 2), and was significantly greater in people with stage 3 (M = 19.31, SD = 3.38) compared to stage 1 (M =13.80, SD = 4.44; P<0.05) and stage 3 compared to stage 2 (M =16.12, SD = 3.07; P=0.008; Figure 2). There was not a significant difference in extent of tissue with spheroids in patients with stage 1 compared to stage 2 lipedema. The fat depots in which spheroids were found most commonly (>50%) included the anterior and dorsal upper and lower arms, ribcage, abdomen, pelvis, subscapular area on the back, flanks, buttocks, front and back of the thighs, the medial knee, popliteal, posterior leg, malleolar, and anterior foot (Figure 3). The sites in which patients had spheroids <50% of the time included the cranium, parotid, submandibular, posterior neck, dorsocervical area, upper chest, hand, and the dorsal foot (boxes, Figure 3); none of the women with stage 1 lipedema had spheroids in these areas. The cubital, anterior forearm, abdomen, thighs, medial knee, popliteal and posterior leg had spheroids 100% of the time in women with stage 1 lipedema. None of the patients with stage 2 lipedema had spheroids in the posterior neck or dorsocervical area; the cubital and medial knee areas contained spheroids in 100% of patients in all stages. There were no areas of examined fat that did not have spheroids in at least one (cranium), two (parotid, submandibular, posterior neck, dorsocervical, dorsal foot), or more patients with stage 3 lipedema. Patients with stage 3 lipedema had spheroids in the cubital, anterior and posterior forearms, abdomen, flanks, buttocks, thighs, medial knee, and posterior leg 100% of the time. Hands were affected in 21% of patients with stage 2 and 31% of patients with stage 3 lipedema. The anterior chest was affected in 40%, 36%, and 38% of patients with stage 1, 2, and 3 lipedema, respectively.
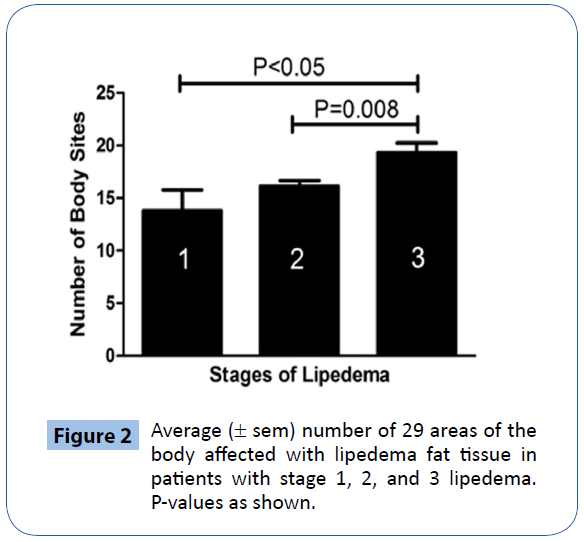
Figure 2: Average (± sem) number of 29 areas of the body affected with lipedema fat tissue in patients with stage 1, 2, and 3 lipedema. P-values as shown.
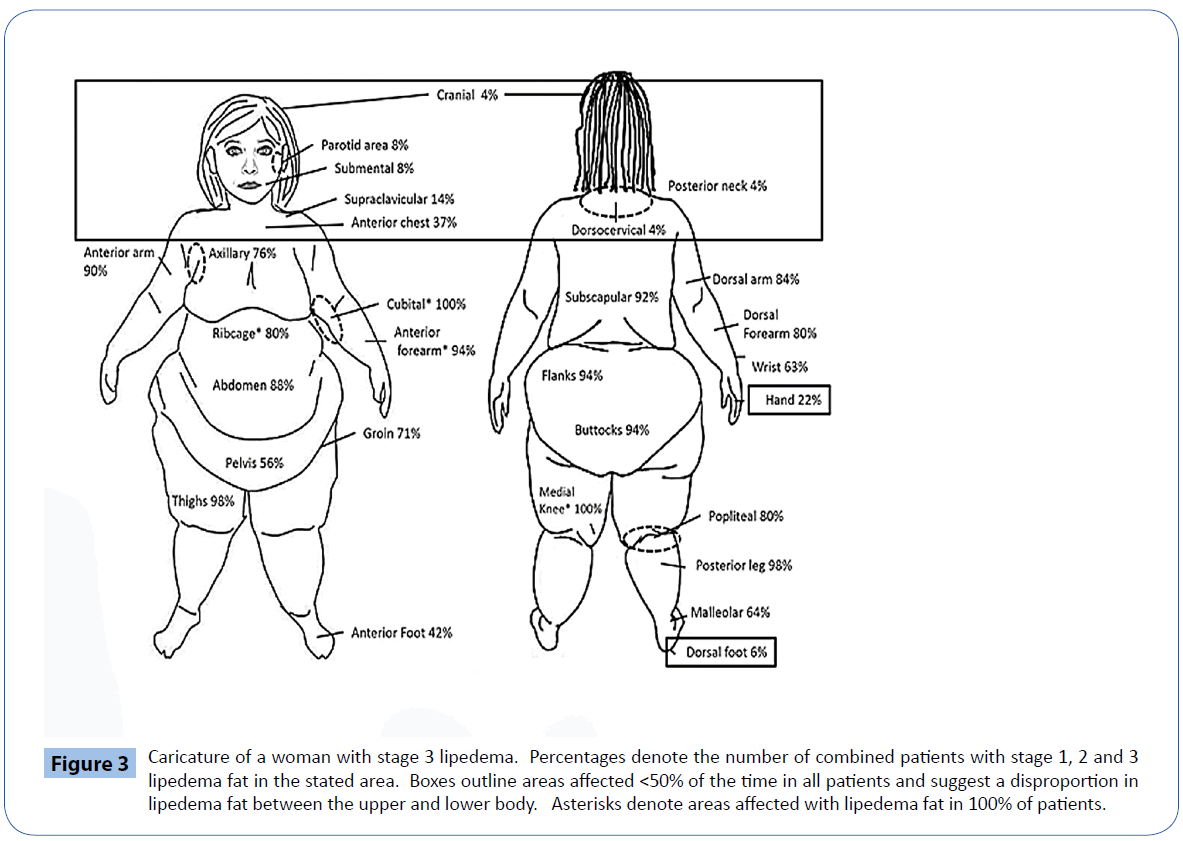
Figure 3: Caricature of a woman with stage 3 lipedema. Percentages denote the number of combined patients with stage 1, 2 and 3 lipedema fat in the stated area. Boxes outline areas affected <50% of the time in all patients and suggest a disproportion in lipedema fat between the upper and lower body. Asterisks denote areas affected with lipedema fat in 100% of patients.
There was no significant difference (P=0.4) in the average number of lipomas on the body in stage 1 (0.8 ± 0.5), stage 2 (0.9 ± 0.2) and stage 3 (0.5 ± 0.2). The number of lipomas in each patient in each stage varied between 0-3.
Signs and symptoms: Patients were asked to fill out a questionnaire listing 66 items as part of a review of systems prior to their clinical visit. Eighteen signs and symptoms from the questionnaire were positive in ≥ 50% of the patients with stage 1 lipedema (Table 2). Unexplained weight gain and muscle weakness were found in ≥ 50% of the patients with stage 2 and 3 lipedema, but not in any patient with stage 1 lipedema. Palpitations, hair loss, frequent urination, numbness, and shortness of breath were present exclusively in ≥ 50% of the patients with stage 3 lipedema (i.e., not in any patients with stage 1 or 2 lipedema). Cellulitis was experienced by 1 person with stage 1 (25 ± 0.5%), seven with stage 2 (22.6 ± 16%), and eleven with stage 3 lipedema (36.4 ± 25%). Other notable signs and symptoms that were more frequent in patients with stage 2 and 3 lipedema included obstructive sleep apnea, blood clot, nausea, constipation, higher body temperature, flu-like symptoms, and burning pain of the skin (Table 2). Signs and symptoms that occurred in <50% of all patients in this study included asymmetry of fat on the left or right side, unexplained weight loss, lumps in neck fat, difficulty swallowing, blurry vision, neck feels swollen, chest pain, burning pain, scalp or other lesions, thirsty all the time, tremors, vomiting, thrombophlebitis, visible veins on arms, tick bite, chronic sinusitis, warts, myoclonus, dry eyes, dry mouth, vertigo, hearing loss, frequent congestion, depression, and anxiety.
| Sign or Symptom |
Stage 1 |
Stage 2 |
Stage 3 |
| Signs, symptoms in 350% of patients with stage 1 lipedema |
| Abdominal pain |
50 ± 41 |
50 ± 13 |
22.2 ± 31 |
| Early satiety |
50 ± 41 |
36.7 ± 15 |
18.2 ± 27 |
| Edema |
50 ± 41 |
74 ± 10 |
100† |
| Headache |
50 ± 41 |
41.9 ± 14 |
36 ± 25 |
| Joint aches |
50 ± 41 |
75.9 ± 9 |
83 ± 12.3 |
| Nasal congestion |
50 ± 41 |
22.6 ± 16 |
25 ± 26 |
| Stress |
69 ± 11 |
83 ± 12 |
83 ± 12 |
| Easy bruising |
75 ± 29 |
68 ± 10.4 |
83 ± 12 |
| Itching |
75 ± 29 |
39 ± 14.3 |
58 ± 20 |
| Fatigue |
75 ± 29 |
77 ± 9 |
91.7 ± 8.7 |
| Low body temperature |
75 ± 29 |
41.4 ± 14 |
33.3 ± 25 |
| Bloating |
75 ± 29 |
58 ± 12 |
45.5 ± 23 |
| Nocturia |
75 ± 29 |
55 ± 12 |
66.7 ± 17 |
| Muscle aches |
75 ± 29 |
65.5 ± 11 |
66.7 ± 17 |
| Low back pain |
75 ± 29 |
71 ± 10 |
66.7 ± 17 |
| Difficulty sleeping |
80 ± 22 |
64.3 ± 12 |
45.5 ± 23 |
| Poor concentration |
100 |
52 ± 10 |
40 ± 26 |
| Visible veins on legs |
100 |
72 ± 10 |
27.3 ± 27* |
| Weigh more at night |
100 |
76 ± 10 |
100 |
| Signs, symptoms exclusively in 3 50% patients with stage 2 and 3 lipedema |
| Muscle weakness |
25 ± 50 |
54.8 ± 12 |
50 ± 24 |
| Unexplained weight gain |
40 ± 39 |
67.7 ± 10 |
58.3 ± 20 |
| Signs, symptoms exclusively in 3 50% patients with stage 3 lipedema |
| Palpitations |
0 |
35 ± 15 |
50 ± 21 |
| Shortness of breath |
0 |
39.3 ± 15 |
50 ± 21 |
| Frequent urination |
25 ± 50 |
41.9 ± 14 |
66.7 ± 17 |
| Hair loss |
0 |
48 ± 15 |
70 ± 18 |
| Numbness |
0 |
43 ± 14** |
82 ± 14** |
| Additional signs and symptoms that increased with stage |
| Blood clot |
0 |
0 |
16.7 ± 28† |
| Burning pain |
0 |
40 ± 14 |
25 ± 26 |
| Constipation |
25 ± 0.5 |
35 ± 10 |
45 ± 23 |
| Flu-like symptoms |
25 ± 0.5 |
29 ± 15 |
33 ± 24.6 |
| High body temperature |
0 |
20 ± 17 |
45 ± 23 |
| Nausea |
0 |
29 ± 15 |
33.3 ± 25 |
| Obstructive sleep apnea |
0 |
14.8 ± 18 |
40 ± 26 |
| *P<0.001 vs. stage 1, 2 |
| **P<0.05 vs. stage 1 |
| †P<0.05 vs. stage 1, 2 |
Table 2: Signs and symptoms in patients with lipedema (% ± se).
Discussion
Lipedema is a SAT disorder found primarily in women. The prevalence of lipedema has been estimated to affect up to 11% and possibly up to 39% of the female population [17,18]. Using the lower prevalence estimate, over 16 million women in the United States may be affected with lipedema. Lipedema developed in patients in our study around the age of 20 y. In the literature, the upper age limit for pubertal changes in the body is 17 y [19] therefore it is likely that lipedema develops during puberty in a majority of patients with lipedema. We were not able to address whether lipedema commenced or was affected by childbirth and/ or menopause.
A review of the literature on lipedema suggests: 1) that lipedema SAT is generally accepted to be located from the ankle up to the lower abdomen and on the upper arms; and 2) that there is a disproportion between the greater size of the body below the waist compared to above the waist, unless obesity is present, and the disproportion is lost [15]. This study of fifty women and a man who presented to a single clinic in an academic setting demonstrates that lipedema fat can be found on the body from the cranium (top of the head) down to the underside (dorsal side) of the foot with the majority of lipedema fat between the axillary region and the ankle; the head and foot were affected in only a small percent of patients with stage 2 and 3 lipedema. In agreement with Cornely [13], in this study, the dorsal forearm had lipedema fat in 80% of patients, and up to 90% of patients had lipedema fat on the anterior arm. The number of areas affected by lipedema fat increased with a higher lipedema stage. In this study, the level of disproportion of lipedema fat was higher on the body (up to the axillary area) than previously described (up to the waist). If we set a limit that at least 75% of patients must have lipedema fat in an area of the body to be considered as “generally affected”, then lipedema fat can extend from the posterior leg up and including to the superior aspect of the axillary crease.
Data from this study suggests that the disproportion of fat on lower compared to upper body presented in the literature primarily refers to women with stage 1 and 2 lipedema, in which lipedema fat is not present on the upper body in the majority. Women with lipedema are under-diagnosed by healthcare providers who do not compare upper body to lower body fat. It is likely that women with stage 3 lipedema are confused more often as having lifestyleinduced obesity [20] as the lipedema fat develops globally and the disproportion diminishes. In stage 3 lipedema, lipedema SAT continues to progress to include more areas of the body, and in this stage there may be greater areas of lipedema fat induced by the development of lipedema secondarily through retention of lymph, as it is well-known that lymph makes fat grow [21]. This area deserves additional research to help patients with lipedema and to shed light on changes in fat in lifestyle-induced obesity. Body composition by dual X-ray absorptiometry scans would have been helpful in this study to examine the disproportion of fat in the different stages of lipedema with greater accuracy as has been published previously [15]. A larger group of patients with stage 1 lipedema would have also improved comparisons amongst the groups.
Lipedema fat can be distinguished from lifestyle-induced fat by palpating spheroids in the fat and in the majority, by pain in the SAT and/or tenderness on palpation of SAT in areas of spheroids. Most healthcare providers have limited time with patients therefore if lipedema is suspected, a focused examination of the cubital and medial knee SAT areas should reveal the presence of lipedema fat as these areas contained spheroids in 100% of the patients in our study. Healthcare providers that diagnose patients with lipedema can use International Classification of Diseases (ICD) codes specific for “Other lymphedema”, ICD-9 457.1, or 272.8 for “other disorders of lipoid metabolism” until lipedema is recognized by our healthcare system.
The stages of lipedema are primarily described in the literature with reference to the skin with smooth skin and an enlarged hypodermis in stage 1, indentations in the skin in stage 2, and lobulations of the skin in stage 3. Data from this study suggest that the stages of lipedema should refer not only to the quality of the skin and lipedema tissue, but also that a greater quantity of the body SAT area is affected as the lipedema stage increases; stating a percent of the body that is affected may be helpful. The presence of lipolymphedema also increases with progression from stage 1 to 2 and 3.
Lipomas were not found in a large number of women with lipedema but they were present in patients with every stage. Better imaging of lipomas by magnetic resonance imaging using proton-density fat saturated sequences [22] would provide a much better assessment of lipomas in lipedema.
There was no past history that clearly appeared to be associated with lipedema. What was striking in this population was the very low incidence of type 2 diabetes (2%). This low prevalence suggests that lipedema fat is not insulin resistant fat, or that the patients were protected from diabetes in some other manner. As lipedema fat in earlier stages is in a purely gynoid distribution (hips, buttocks and thighs), and gynoid fat confers lower cardiovascular risk [23], lipedema fat may also confer less cardiovascular risk in stage 1 and 2 and possibly also in stage 3. A major concern resulting from the review of systems in this study was the increase in shortness of breath, palpitations, urination, and numbness in patients with stage 3 lipedema. We hypothesize that these symptoms suggest excess fluid accumulation in the body as pre-lymph or lymph fluid. Indeed, edema and cellulitis increased with stage of lipedema in this study consistent with this hypothesis. Women with stage 3 lipedema were also more likely to have obstructive sleep apnea, nausea, constipation and flulike symptoms. These data suggest that the metabolic protection of the lipedema fat wanes in stage 3 lipedema as the lipedema fat spreads globally on the body and patients develop signs of systemic illness. The only known treatment to reduce lipedema fat at this time is excision by lymph-sparing liposuction, a treatment for lipedema established in Germany for over 20 years [24-26]. Furthering our understanding of the pathophysiology of lipedema and medical treatments for reducing lipedema fat are needed so we are not relying solely on surgical management of lipedema fat.
Hypermobility is not a condition reported in association with lipedema but in this report,~50% of women with lipedema had a positive Beighton score ( ≥ 5) suggesting that they may also have the common disorder known as Ehlers Danlos syndrome hypermobility type (EDS-HT) formerly type III) [27]. Pain is a common component of EDS-HT and females are functionally affected to a greater extent than males and therefore this association should be further investigated.
Venous disease is known to occur in women with lipedema [28]. The data in this study demonstrated that as the stage of lipedema increased, visible veins decreased. Interestingly, venous blood clots were only present in women with stage 3 lipedema. These data suggest a masking of underlying venous disease by excess lipedema fat. The development of lymphedema in a patient with lipedema should prompt not only a reassessment by a manual lymphatic drainage therapist, but also evaluation for venous disease by a vascular surgeon, consideration for a sleep study for evaluation of obstructive sleep apnea, and an echocardiogram to assess for heart failure.
The single man was included in our study to serve as a reminder that men can also develop lipedema [6]. Men who develop lipedema tend to be hypogonadal as our patient, have a history of hypogonadal symptoms and signs such as gynecomastia, or have liver disease [29] resulting in elevated estrogen levels. In the hypogonadal state in a man, the ratio of testosterone to estradiol (an estrogen) is altered, and estradiol plays a greater role in tissues that have sex hormone receptors such as SAT. Lipedema occurs primarily in women suggesting that estrogen plays a pivotal role in the development of lipedema SAT. Men with higher effective levels of estrogen may be at greater risk for developing lipedema fat.
This study was performed at a tertiary referral center that was available to people living in the local area and to those who can travel. Patients with lipedema who were too ill to travel or who were financially unable to travel would be under-represented in this study.
In conclusion, lipedema is a common disorder likely present in millions of women all over the world. Lipedema fat can affect any area of SAT, but is found more often in SAT at or below the axillary area and above the ankle. Obesity increases with stage of lipedema but overall, lipedema SAT confers a disproportionately larger lower body. The presence or absence of lipedema fat can be quickly assessed around the cubit nodes or the medial knee, areas affected in 100% of patients in this study. Women with stage 3 lipedema develop signs and symptoms associated with increased cardiovascular risk suggesting the need to evaluate for underlying conditions such as venous disease or obstructive sleep apnea in patients with lipedema prior to but especially after diagnosis of stage 3. Studying lipedema and lipolymphedema can help millions of women, and provide a better understanding of lymphedema that develops secondary to obesity [30].
6744
References
- Allen EV, Hines EAJ (1940) Lipedema of the legs: A syndrome characterised by fat legs and orthostatic edema. Proc Staff Meet Mayo Clin 15: 184-187.
- Spiller WG (1898) Clinical Memoranda: Report of three cases of adiposis dolorosa. Medical News 268-270.
- Cornely ME (2006) Lipedema and Lymphatic Edema. In Liposuction. Springer.
- (2001) Lipoedema. Guidelines of the German Society of Phlebology (DGP). Dusseldorf Association of the Scientific Medical Societies.
- Fife CE, Maus EA, Carter MJ (2010) Lipedema: a frequently misdiagnosed and misunderstood fatty deposition syndrome. Adv Skin Wound Care 23: 81-92.
- Meier-Vollrath I, Schmeller W (2004) [Lipoedema--current status, new perspectives]. J DtschDermatolGes 2: 181-186.
- Pascucci A, Lynch PJ (2010) Lipedema with multiple lipomas. Dermatol Online J 16: 4.
- Fife CE, Maus EA, Carter MJ (2010) Lipedema: a frequently misdiagnosed and misunderstood fatty deposition syndrome. Adv Skin Wound Care 23: 81-92.
- Inamadar AC, Palit A (2004) Cutaneous signs in heritable disorders of the connective tissue. Indian J DermatolVenereolLeprol 70: 253-255.
- Beighton P, Horan F (1969) Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br 51: 444-453.
- Reich-Schupke S, Altmeyer P, Stucker M (2013) Thick legs - not always lipedema. J DtschDermatolGes. 11: 225-233.
- Cornely M (2011) Lipoedema of arms and legs. Conservative and surgical therapy of the lipoedema, Lipohyper- plasia dolorosa.
- Beninson J, Edelglass JW (1984) Lipedema--the non-lymphatic masquerader. Angiology 35: 506-510.
- Dietzel R, Reisshauer A, Jahr S, Calafiore D, et al. (2015) Body composition in lipoedema of the legs using dual-energy X-ray absorptiometry: a case-control study. Br J Dermatol .
- Malfait F, Wenstrup R, De Paepe A (2013) Ehlers-Danlos Syndrome, Classic Type: Synonym: Ehlers-Danlos Syndrome, Classical Type. Ehlers-Danlos Syndrome Type I, Ehlers-Danlos Syndrome Type II.
- Beninson J, Edelglass JW (1984) Lipedema--the non-lymphatic masquerader. Angiology 35: 506-510.
- Marshall WA, Tanner JM (1969) Variations in pattern of pubertal changes in girls. Arch Dis Child 44: 291-303.
- Herbst KL (2012) Rare adipose disorders (RADs) masquerading as obesity. ActaPharmacol Sin 33: 155-172.
- Schneider M, Conway EM, Carmeliet P (2005) Lymph makes you fat. Nat Genet 37: 1023-1024.
- Tins BJ, Matthews C, Haddaway M, Cassar-Pullicino VN, Lalam R, et al. (2013) Adiposis dolorosa (Dercum's disease): MRI and ultrasound appearances. ClinRadiol 68: 1047-1053.
- Wiklund P, Toss F, Weinehall L, Hallmans G, Franks PW, et al. (2008) Abdominal and gynoid fat mass are associated with cardiovascular risk factors in men and women. J ClinEndocrinolMetab 93: 4360-4366.
- Warren AG, Janz BA, Borud LJ, Slavin SA (2007) Evaluation and management of the fat leg syndrome. PlastReconstrSurg 119: 9e-15e.
- Stutz JJ, Krahl D (2009) Water jet-assisted liposuction for patients with lipoedema: histologic and immunohistologic analysis of the aspirates of 30 lipoedema patients. Aesthetic PlastSurg 33: 153-162.
- Rapprich S, Dingler A, Podda M (2011) Liposuction is an effective treatment for lipedema-results of a study with 25 patients. J DtschDermatolGes 9: 33-40.
- De Wandele I, Rombaut L, Malfait F, De Backer T, De Paepe A, et al. (2013) Clinical heterogeneity in patients with the hypermobility type of Ehlers-Danlos syndrome. Res DevDisabil 34: 873-881.
- Wold LE, Hines EA Jr, Allen EV (1951) Lipedema of the legs; a syndrome characterized by fat legs and edema. Ann Intern Med 34: 1243-1250.
- Weissleder H, Schuchhardt C (1994) Erkrankungen des Lymphgefa systems. KargererKommunikation.
- Helyer LK, Varnic M, Le LW, Leong W, McCready D (2010) Obesity is a risk factor for developing postoperative lymphedema in breast cancer patients. Breast J 16: 48-54.