Keywords
Lung cancer; Pneumonia; COVID-19
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARSCoV- 2) is a highly contagious virus, first appearing in Wuhan, China, December of 2019. This virus causes the multi-system organ disease Coronavirus Disease 2019 (COVID-19). Although symptoms and severity are varied, the most reported complication of COVID-19 is acute respiratory failure with hypoxia secondary to viral PNA, thus leading to ARDS.
Various groups are at higher risks for developing severe COVID-19 disease, including age greater than 50, cancer, chronic kidney disease, COPD, DM2, CHF, CAD, immunocompromised states from organ transplant, obesity with BMI >30, sickle cell disease, smoking, etc. [1]. Also, Hispanics, African Americans and Native Americans are 3-5 times more likely to be hospitalized with COVID-19 than whites [2,3].
Aside from the pandemic and the strain it has caused on our medical resources, reducing rates for admissions and readmissions is a continual goal of hospital medicine nationwide. Great effort has been put into determining groups at risk for both hospital admissions and readmissions. Patients with cancer contribute to the significant population at risk for high amounts of healthcare utilization [4,5]. Nearly 50% or more patient with cancer are admitted at least once with approximately 10% of this group at risk for readmission [6,7]. Other causes of admission seen as infection, pain, VTE [8]. Per prior report, over half of the admissions were related to failure to thrive and depression [9].
Lung cancer is the leading cause of cancer death in the US [10]. Lung cancer is the third most common cancer in the US, behind skin cancer (#1), breast cancer in women and prostate cancer in men [10]. The overall 5 year survival rate for lung cancer is only 21.7% [11]. Since lung cancer is a leading cause of death in the US, lung cancer patients are at high risk for hospitalization.
Recent reports state patients with lung cancer are at more risk of developing COVID-19, as well as severe symptoms, than the general population [11,12]. Due to this increased risk of patients with lung cancer being adversely at risk for COVID-19, several lung cancer advocacy groups have released joint statements advocating safety measures such as social distancing and education about the vaccine [13,14].
In this study, causes for admission and readmission for lung cancer patients admitted to the CUMC-B Hospital Internal Medicine Department will be determined in the year 2019. This group of patients from 2019 will be followed into 2020 to determine which patients contracted COVID-19. Furthermore, if the surviving group of patients from 2019 into 2020 developed COVID-19, the hospitalization and admission status will also be determined.
Materials and Methods
Study design
Patients were identified through chart review via the Electronic Medical Records System (EMR). Diagnosis of lung cancer was confirmed by chart review. The following information was obtained: patient’s age, race, sex, cancer type and stage, if receiving chemo, surgery and/or radiation, reason for admission, readmission in 30 days vs 365 day and if so, what was the cause for readmission. Patients who survived into 2020 were followed and then had their COVID-19 status determined, as documented in the EMR. Data and statistics were be complied using Microsoft Excel using a secure university-based network. Each unique diagnosis was counted once per patient. Only acute (not chronic) illnesses treated during admission were evaluated.
Participants
Patients included in the study had an established diagnosis of lung cancer receiving or pending treatment (chemotherapy, immunotherapy, surgery, and/or radiation). Admission criteria were exclusively at CUMC-B Internal Medicine (IM)/Hospitalist Department from January 1, 2019-December 31, 2019. Evaluation of COVID-19 in surviving patients from same cohort of patients from 2019 into 2020. Patients excluded from this study included new diagnosis of lung cancer received during the admission; otherwise, not under the care of an oncologist. Patient also excluded include those who declined further cancer care prior to admission (ie: hospice), admitted outside CUMC-B, admitted to another inpatient hospitalist group, such as private practitioners or another medical team (i.e., cardiothoracic surgery, family medicine), and those under the age of 19 or older than 89.
Results
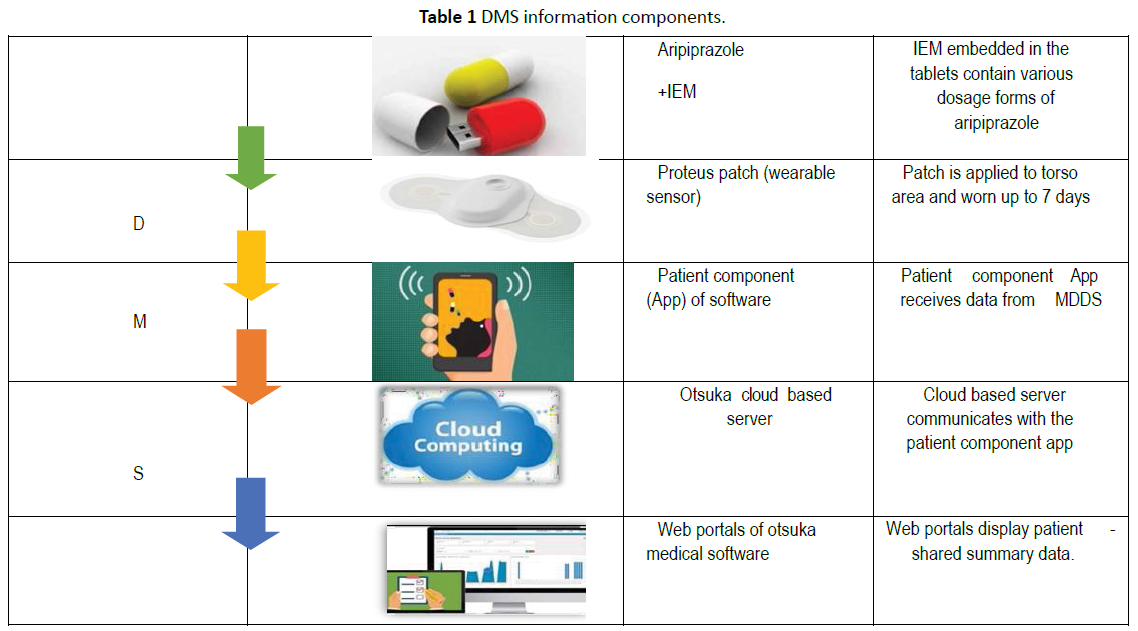
The number of patients eligible, based on inclusion criteria: 37 (selected from 311 candidates) (Table 1). There were a total 83 hospitalizations amongst these patients and 47 separate causes for admission in lung cancer patients in 2019 (admission and readmission data were combined) (Table 2). Of 47 separate causes for hospitalizations, there were an average of 3.3 causes for admission per each hospitalization, and average number of hospitalizations per patient was 2.24 (range 1-6). The top 14 causes for admission were responsible for 71.4% of the admissions of lung cancer patients in 2019 (Figure 1). Out of the 37 patients, 12 were readmitted within 30 days, 18 were readmitted within 2019. Seven patients out of 11 patients who died transitioned into hospice (Table 2).
| Characteristics |
Participants (n = 37) |
| Mean age, years, n |
66 (range 36-88) |
| Sex, n |
| Female |
21 |
| Male |
16 |
| Race, n |
| White, n |
31 |
| Black, n |
3 |
| Hispanic, n |
2 |
| Missing, n |
1 |
| Non-small cell lung cancer, n=23 |
| Stage 4, n |
19 |
| Stage 3b, n |
2 |
| Stage 2, n |
1 |
| Stage 1b, n |
1 |
| Small cell lung cancer, n=14 |
| Extensive, n |
11 |
| Limited, n |
3 |
Table 1 Characteristics of randomly assigned study participants.
| Characteristics |
Participants (n = 37) |
| Readmission within 30 days |
12 |
| Readmission within 365 days |
18 |
| Total number of hospitalizations |
83 (Average 2.24 hospitalizations per patient with range 1-6) |
Table 2 Admission and readmission data in 2019.
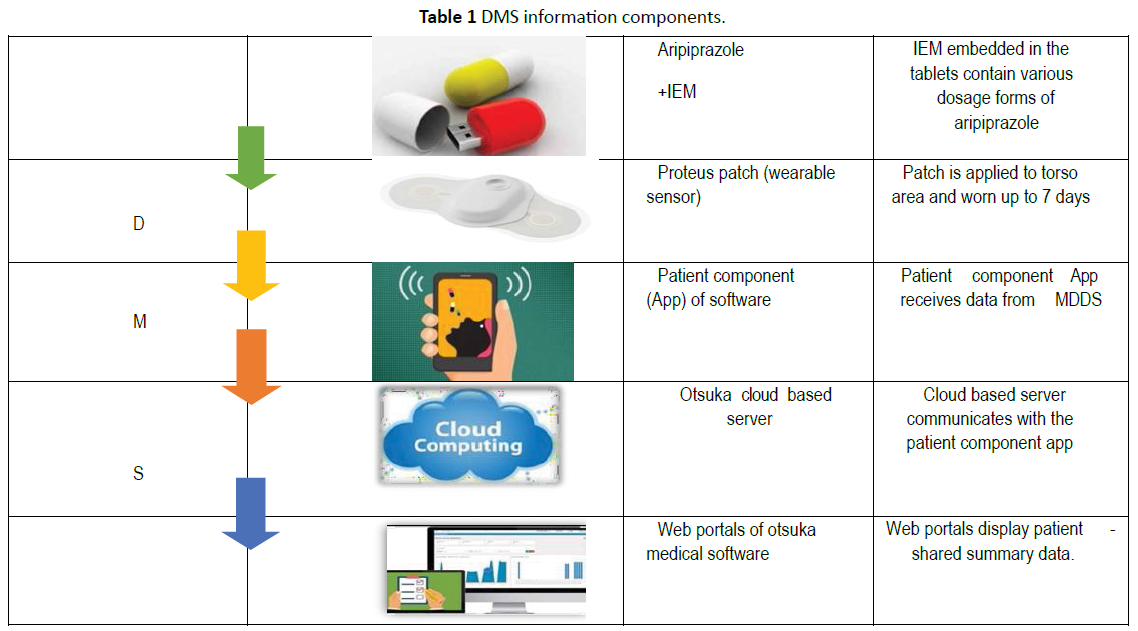
Figure 1: Top 14 causes for admission and readmission for lung cancer patients in 2019 at CUMC-B.
Of the 26 patients who remained after March 2020 into Dec 31, 2020, an additional 10 patient died (15 remained alive or unknown at end of 2020). Thirteen patients have died after March 1, 2020. Of these patients who survived after March 1, 2020, one had a confirmed positive COVID-19. Nine additional patients were tested COVID-19, and found to be negative. None of the 13 patients who died in 2020 had known COVID-19 or died from it (Table 4).
| Diagnosis |
Number of admissions |
| Pneumonia |
26 |
| Acute Respiratory Failure With Hypoxia |
17 |
| Anemia Requiring Transfusion |
10 |
| Cancer Associated Pain |
8 |
| COPD Exacerbation |
8 |
| Non Cardiac Chest Pain |
7 |
| VTE |
5 |
| FTT |
5 |
| Hyponatremia |
4 |
| CHF Exacerbation |
5 |
| GI Bleed |
4 |
| Non-Specific Abdominal Pain |
4 |
| Malignant Pleural Effusion |
4 |
| Chemotherapy Induced Neutropenia |
3 |
| SVT |
2 |
| Collapse Of Lung |
2 |
| Hypotension |
2 |
| Thrombocytopenia Requiring Transfusion |
2 |
| AKI |
2 |
| Hip Fracture Requiring Surgery |
2 |
| NSTEMI |
2 |
| Pericardial Effusion |
2 |
| Septic Shock |
2 |
| Non Malignant Pleural Effusion |
2 |
| Transfusion-Associated Reaction |
2 |
| Unspecified Back Pain |
1 |
| Unspecified Pelvic Pain |
1 |
| Hemoptysis |
1 |
| UTI |
1 |
| BPH |
1 |
| Headache |
1 |
| Dysphagia |
1 |
| Sepsis, Unknown Source |
1 |
| Pneumonitis, Chemo Induced |
1 |
| Acute Ischemic CVA |
1 |
| Critical Limb Ischemia |
1 |
| Nausea And Vomiting 2/2 Brain Mets |
1 |
| Nausea And Vomiting 2/2 Pneumatosis |
1 |
| Gastroenteritis |
1 |
| AFIB With RVR |
1 |
| Acute Cholecystitis |
1 |
| Ground Level Fall |
1 |
| Opioid OD |
1 |
| Osteomyelitis |
1 |
| Syncope |
1 |
| Cellulitis |
1 |
| Immune Therapy Induced Enterocolitis |
1 |
| Abbreviations: COPD: Chronic Obstructive Pulmonary Disease; VTE: Venous Thromboembolism; FTT: failure to thrive; CHF: Congestive Heart Failure; GI: Gastrointestinal; SVT: Supraventricular Tachycardia; AKI: Acute Kidney Injury; NSTEMI: Non ST Elevation Myocardial Infarction; UTI: Urinary Tract Infection; BPH: Benign Prostatic Hyperplasia; CVA: Cerebrovascular Accident; 2/2: secondary to; AFIB with RVR: Atrial Fibrillation with Rapid Ventricular Response; OD: Overdose. |
Table 3 Causes for admission for lung cancer patients in 2019.
| Characteristics |
Participants (n = 37) |
| Number of patients who died before March 1, 2020 |
10 |
| Number of patients who died after March 1, 2020 |
13 |
| Number of patients alive or unknown as of December 31, 2020 |
14 |
| COVID-19 Negative |
9 |
| COVID-19 Positive |
1 |
| COVID-19 hospitalizations or deaths in 2020 |
0 |
| Unable to confirm COVID-19 status |
14 |
Table 4 Characteristics of randomly assigned study participants, COVID-19 status, and survival.
Discussion
Patients with lung cancer, who were admitted to CUMC-B in 2019 and 2020, tended to have stage 4 or extensive disease. Of the 37 patient charts reviewed, 12 were readmitted within 30 days and 18 readmitted within 365 days in 2019. Average number of hospitalizations per patient in year 2019 was approximately 2. There are 14 top diagnoses that are responsible for over 70% of the admissions. The two most common diagnoses codes found in this study are acute respiratory failure with hypoxia and pneumonia. Seven of the 37 patients were transitioned to hospice while admitted within that 365 days in 2019. Other notable causes for admission were cancer associated pain and anemia requiring transfusion. Further investigation into causes for hospitalization for lung cancer patients, as findings novel strategies to reduce readmissions in this high risk group, is warranted in future directions.
Of the surviving patients from 2019 into 2020, only one had confirmed COVID-19, although it was not a cause for hospitalization. It is unclear why this population of patients at CUMC-B did not suffer from the effects of COVID-19, including hospitalization. Although the reason for lack of COVID-19 admissions at CUMC-B is unclear, the most likely is non pharmaceutical interventions, such as wearing masks and social. Observational data suggests masks mitigate spread of SARS-CoV-2 [15,16].
Mask wearing is not a new practice, introduced in 1910 during the Manchurian Plague [15]. Face coverings have been recommended for protection from respiratory pathogens since the 14th century, even during the Spanish Flu in the early 20th century. Mask wearing became prominent again during this pandemic. Although there are currently no known randomized control trials that support use of mask wearing for any respiratory pathogen on community transmission, there are observational data that support use of masks [15]. Evidence for wearing masks is stronger in healthcare than community settings. Evidence for SARS-CoV-2 limited to 2 observational studies, limited reliability [16]. There is some evidence for reduced community viral transmission with other viral illnesses [16].
Social distancing/quarantining, another non-pharmaceutical practice, also not a new practice in prevention of infectious disease, as these means to control infection (social distancing, border control, contract tracing) have been used for centuries - from Black Plague to 1918 flu. School closures also evidence of social distancing reducing influenza pandemics.
The findings in this study, regarding causes for hospitalization in lung cancer patients, correspond to some recent reports. In a recent study, pulmonary disease was reported to be the most common reason for admission with lung cancer patients, followed by cardiovascular and gastrointestinal disease [17]. With our report, CHF exacerbation and GI bleeds are also leading causes for lung cancer admission. This report did not mention cancer associated pain as leading cause for hospitalization, however, and the relevance of this is unclear. This study does differ from ours, mainly due to larger sample size, and that the cohort included patient who had survived at least 5 years after diagnosis. In another study, most common symptoms for admission were dyspnea, fever, hemoptysis, respiratory infections and neutropenia [18]. Cancer associated pain was not mentioned as a leading cause for admission in this study, as well.
Based on this study, and prior reports, it is evident that lung cancer patients are at high risk for admission due to respiratory failure and pneumonia, making the COVID-19 a particularly difficult prospect for this vulnerable group of patients. One report stated that 52.3% of their lung cancer patients who developed COVID-19 died versus 10% total COVID-19 patient mortality at their center [19]. In a recent systemic review and meta-analysis, patients with cancer had an overall high mortality rate, and this study referenced many studies that included lung cancer [20].
Although lung cancer patients in CUMC-B did not appear to require hospitalization for COVID-19, there appears to be an increased overall death rate. From Jan 1, 2019 into March 1, 2020, there were 11 deaths out of 37 patients. From March up until the present, there were 13 deaths out of 26 patients. Based on low sample size, it is unclear if any real conclusion can be drawn. That aside, it is plausible that patients could have also resisted medical care, based on fear of contracting COVID-19. According to the CDC, by June 30, 2020, because of concerns about COVID-19, an estimated 41% of US adults had delayed or avoided medical careboth emergency and routine care [21].
Limitations
Limitations of this study include small sample size, possibility for selection bias (since patients were manually selected to meet study criteria), inability to know COVID-19 status of 14 patients, inability to know if these patients died in other hospital systems outside of the EMR used (Epic) vs home/hospice.
Conclusion
Despite these limitations, the conclusions of this study are as followed. Patients with lung cancer are at high risk for being admitted with pneumonia, being the number one cause for admission for lung cancer patients, in 2019, and second main cause being acute respiratory failure with hypoxia. However, in 2020, there were no lung cancer patients admitted because of COVID-19 at CUMC-B, despite significant literature stating patients with lung cancer have a higher rate of morbidity and mortality if infected with this novel virus. Although the cause for this is unknown, the protection of lung cancer patients from COVID-19 is likely a result of non-pharmaceutical interventions. One cannot deny that overall death rates did increase amongst this cohort of patients past March 1, 2020. The cause is unclear, and small sample size is a limitation, but it is possible that medical care was delayed or avoided for fear of contracting COVID-19.
38467
References
- https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
- https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/increased-risk-illness.html
- Albright HW, Moreno M, Feely TW (2011) The implications of the 2010 Patient Protection and Affordable Care Act and the Health Care and Education Reconciliation Act of cancer care deliver. Cancer 117: 1564-1574.
- Zuckerman RC, Sheingold SH, Orav EJ, Ruhter J, Epstein AM (2016) Readmissions, observation, and the Hospital Readmissions Reduction Program. N Egl J Med 374: 1543-1551
- Bekelman JE, Halpern SD, Blankart CR (2016) Comparison of site of death, healthcare utilization, and hospital expenditures for patient dying with cancer in 7 developed countries. JAMA 315: 272-283
- Earle CC, Neville BA, Landrum MB (2004) Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol 22:315-321
- Oniell B, Atoria CL, O’Reilly EM (2016) Hospitalization in Older Adults with advanced cancer: the role of chemotherapy. J Onc Prac 12: e138-148
- Nipp RD, El-Jawahri A, Moran SM (2017) The relationship between physical and psychological symptoms and the health care utilization in hospitalized patients with advanced cancer. Cancer 4720-4727.
- Jing Y, MD Wen O, Melvin LK, Conghua X (2020) SARS-CoV-2 Transmission in Patients With Cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol 6: 1108-1110
- Luo J, Rivzi H, Preeshagul S (2020) COVID19 in patients with lung cancer. Ann Oncol 31: P1386-1396
- https://www.lungcancerresearchfoundation.org/lung-cancer-groups-issue-statement-on-coronavirus/
- Howard J, Huang A, Li Z (2021) An evidence review of face masks against COVID19. PNAS 118: 1-12.
- Chou R, Tracy D, Jungbaurer R (2020) Masks for the prevention of Respiratory Virus Infections, Including SARS-CoV-2, in healthcare and community settings, a living rapid review. Ann Intern Med 173: 542- 556.
- Geena X, Ituarte Phillip HG, Ferrell B, Sun V, Erhunmwunsee L, et al. (2020) Causes of Death and Hospitalization in Long-term Lung cancer survivors: A population-based appraisal. Clin Lung Cancer 21: 204-213.
- Kiapikou A, Petras P (2017) Causes for hospitalization in patients with lung cancer. Eur Clin Respir J 50 pp: 1-61.
- Rogado J, Pangua C (2020) COVID19 and lung cancer – a greater fatality rate? Lung Cancer 146: 19-22
- Venkatesulu B, Chandrasekar V (2021) A systemic review and meta-analysis of cancer patients affected by a Novel Coronavirus. JNCI Cancer Spectrum 5: 1-11