Keywords
Multiple symmetric lipomatosis; Benign symmetric lipomatosis; Madelung's disease; Launois- Bensaude syndrome
Introduction
Madelung's disease also known as Launois-Bensaude syndrome, Multiple Symmetric Lipomatosis (MSL), cephalothoracic lipodystrophy, and benign symmetric lipomatosis - is a condition characterized by subcutaneous and deep non-encapsulated symmetric lipomas, mostly accompanied by polyneuropathy and metabolic disorders. The first description of the disease was made by Benjamin Brodie in 1846. Otto Wilhelm Madelung describes in 1888 the classic 'horse collar' pattern secondary to the head and neck distribution of the lipomas. Launois and Bensaude complete their description of this syndrome in 1898, giving it the name of multiple symmetric adenolipomatosis.
Case Report
A 45 year-old man was admitted to our hospital due to a 3- month evolution medical condition characterized by asthenia and lack of energy. A daily alcohol intake of 192 gr per day has to be mentioned as a significant background.
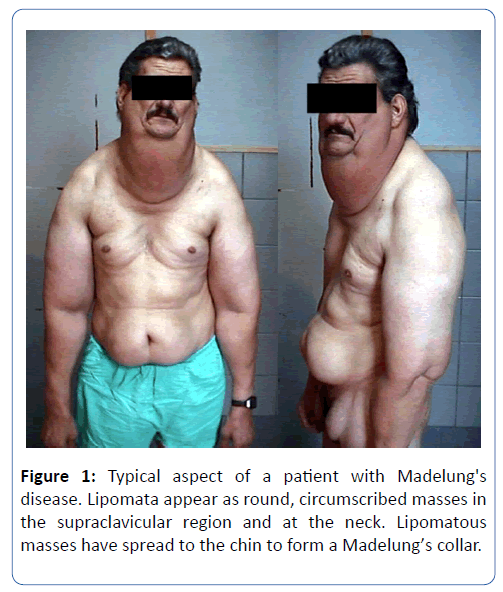
Physical examination revealed pale conjunctivas and jaundiced sclera. Painless symmetric soft tumors were verified in the cervical, thoracic, abdominal, inguinal, and upper limbs areas (Figure 1). The muscular bulk was hypotrophic and tendon reflexes were normal.
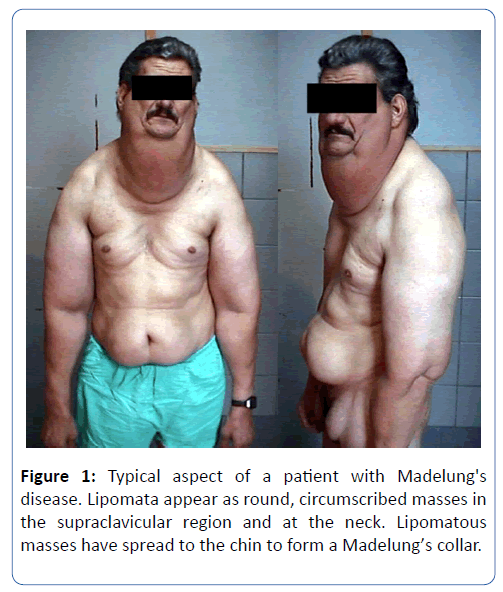
Figure 1: Typical aspect of a patient with Madelung's disease. Lipomata appear as round, circumscribed masses in the supraclavicular region and at the neck. Lipomatous masses have spread to the chin to form a Madelung’s collar.
Lab tests showed hematocrit 7%; mean corpuscular volume 115 fL; hemoglobin 2 g/dl; transferrin 392 μg/dl; hemoglobin saturation 21%; serum iron 81 μg/dl; corrected reticulocyte count 6.7%; platelets 22,000 mm3; GOT 151 UI/l; GPT 151 UI/l; GGT 151 UI/l; total bilirubin 4.5 mg/dl; lactic dehydrogenase 2300 UI/l; calcemia 7.9 mg/dl; phosphatemia 1.9 mg/dl; magnesemia 2 mg/dl; Prothrombin Time (PT) 18 seconds (reference: 12 seconds); Activated Partial Thromboplastin Time (APTT) 42 seconds (reference: 30 seconds); uric acid 9 mgdl; creatine phosphokinase 45 UI/l; aldolase 15 UI/l; total cholesterol 81 mg/dl; HDL cholesterol 16mg/dl; triglycerides 150 mg/dl; TSH of 1.83 μUI/ml; and the serology for HIV, HBV, and HCV was negative.
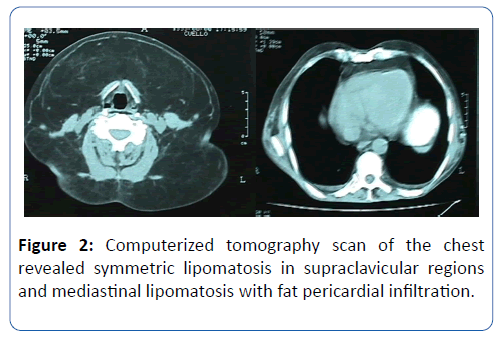
The neck ultrasound scan revealed a significant soft tissue thickening and the CT scan of neck and thorax showed a marked increase of subcutaneous cellular tissue in the neck, and growth of the pericardial fat (Figure 2).
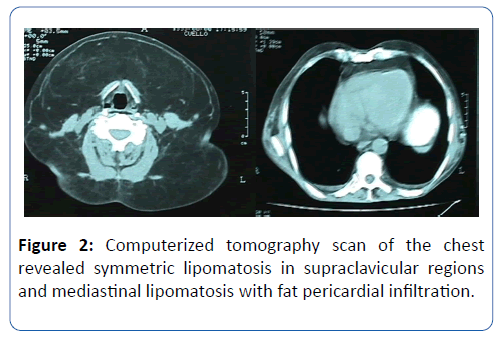
Figure 2: Computerized tomography scan of the chest revealed symmetric lipomatosis in supraclavicular regions and mediastinal lipomatosis with fat pericardial infiltration.
A biopsy of neck soft tissue was compatible with adipose tissue of normal characteristics. The electromyography (EMG) reveals a miopathic pattern.
The medical condition of the patient was interpreted as megaloblastic anemia in the context of Madelung's disease.
Patient was followed up over two years four times every year. In each consultation he was assessed with clinical examination and analytical variables commonly required. Medical control showed no changes of his illness. Patient was a homeless and after two years of follow up he didn´t attended at hospital anymore.
Discussion
Madelung's disease is a rare condition that occurs typically between 30 and 60 years of age with a male: female ratio of 15:1. It has a higher incidence in the Mediterranean region, with one case in every 25,000 males. Around 300 cases have been reported in Western literature up to date [1].
The disease has two clinical forms of presentation. The sporadic form of the disease begins in adults and it is related to alcoholism with a frequency between 60% to 90% [2]. The association with treatment with protease inhibitors, especially Indinavir, has been described [3]. The familial variant of the disease is transmitted in an autosomal recessive way, and it makes its appearance during childhood [4].
Based on phenotype there are two recognizable variables of this condition. Type 1 variable is reported in males with normal or low Body Mass Index (BMI). It manifests itself with symmetric non-encapsulated lipomas distributed in the upper part of the body and limbs affecting the adipose tissue in deep structures of the neck, thorax, and abdomen. The fatty tissue not affected by it shows progressive atrophy.
The first physiopathogenic theories stated the presence of a mitochondrial disorder due to an alteration of the respiratory chain caused by a decrease in the activity of C oxidase cytochrome (Complex IV), mitochondrial sarcolemic aggregates, and multiple suppressions in mitochondrial DNA [5-8]. These alterations cause a decrease in ATP formation with lipolysis blockage. This partly explains the resistance to the adrenergic lipolytic action. The distinctive distribution of lipomas around the neck and shoulders is the consequence of the prevailing presence of brown fat- rich in mitochondria - in the aforementioned places. The mitochondrial dysfunction results in progressive lipidic accumulation due to mitochondrial respiration and lipolysis are associated with brown fat [8]. A defect of mesenchymal stem cells is suggested among the latest aetiopathogenic theories [9].
The diagnosis is mainly clinical. Imaging tests help assessing process scope. Histopathology reveals similar characteristics than normal adipose tissue, with smaller multivacuolated adipocytes associated with interstitial fibrosis and proteoglycans [10].
Their growth is frequently slow, the first consequence being purely aesthetic. Nevertheless, they can lead to internal organ compression in advanced stages of the disease [11].
The association between MSL and PN is frequent. The latter is evident several years after the occurrence of lipomas. Even though PN aetiology has been ascribed to alcohol for years, it’s very presence in non-alcoholic patients, the demyelinating pattern, and the absence of regression of the PN with the suppression of alcohol, have ruled out such association [12].
Weather there is a relation between polyneuropathy and precise genetic defects or not it is something yet to be confirmed. Neurologic manifestations generally appear in more than half the cases during middle-age (30 to 40) and they have a tendency to be progressive. Their most common forms involve thermoalgesic, proprioceptive, vibratory, and autonomic sensibility, with variable levels of intensity. Within the latter, sexual impotence and perspiration are the most frequent signs. Other less usual neurologic disorders are pyramidalism, cerebellar signs, and seizures [13].
Typical electromyographic patterns are characterized by presenting a decrease in the range of the sensitive action potential, reduced conduction velocity of motor evoked potential, and fibrillation potential [12].
Miopathy is not frequent, and muscle biopsy reveals fiber atrophy, intramitochondrial subsarcolemic deposits, fiber tear, and diffuse muscle denervation-reinnervation [13]. Lab abnormalities include anemia, macrocytosis, oral glucose intolerance, peripheral insulin resistance, hepatogram alterations, hyperuricemia, dyslipidemia, renal tubular acidosis, hyperthyroidism, and hypothyroidism. Due to the fact that some of these disorders are very often associated with alcoholism it cannot be inferred that such abnormalities are a characteristic of MSL [12].
A differential diagnosis must be made with other clinical entities. Dercum's disease is characterized by multiple fatty deposits distinctively painful, with a similar distribution to that of MSL; affecting mainly women with overweight and potential spontaneous reversal. Lipomas are composed of variable-sized slow-growing movable soft adipose tissue.
The existence of diverse sized generally painless adenomegaly in cervical, axillary, and inguinal regions makes it necessary to rule out lymphoma. MSL, in its early stages, is sometimes misdiagnosed as sialoadenitis.
Surgical treatment-lipectomy or liposuction - is among the possible therapeutically resources, for aesthetical purposes and, eventually, because neighboring structures are compromised. MSL might recur after 3 to 5 years after surgery [10].
The oral administration of salbutamol could prevent the increase of the size of lipomas and a rapid mass growth [14]. Treatment with corticoids has been reported in cases of severe polyneuropathy [15].
In recent years, ultrasound waves have been described as a possible treatment due to its activation of the cellular metabolism with a reduction in mass size. Intra-lesional injection of enoxaparin and hypolipemiant has also been proposed as treatment, with controversial results [16,17]. Abstinence from alcohol has not showed an effect in lesion reduction, but it does have an effect on recurrence after treatment.
Conclusion
Benign symmetric lipomatosis is considered a rare disease characterized by the symmetric growth of fatty tumors distributed throughout the body. According to its distribution, two different classification systems can be established. The disease is frequently present in patients aged 30 to 60 with a 15:1 male: female ratio. Although the physiopathogenic pathways remain unknown until now, two different theories have been proposed: mitochondrial disorder due to an alteration of the respiratory chain, and a defect of mesenchymal stem cells. Diagnosis can be made by anamnesis and a physical examination, although imaging tests help in the assessment of the process scope. Based on phenotype, there are two different clinical classifications. Clinical findings are related to the neurological system and disorders of analytical variables, such as anemia and thrombocytopenia or myopathy, are not often observed. A condition that should be considered as a differential diagnosis is Dercum's disease. There is not a curative treatment. The non-curative treatment aims to improve severe polyneuropathy with corticosteroids, prevent the increase of the size of lipomas and a rapid mass growth with salbutamol, surgical treatment for aesthetical purposes and intra-lesional injection of enoxaparin and hypolipemiants with controversial results. The patient we report consulted a doctor about asthenia and lack of energy, he showed a typical Madelung´s collar and severe anemia. Anemia was treated with ferrous sulphate and folic acid with an acceptable improvement of hematocrit. Patient was followed-up for two years until he stopped going to the hospital.
28389
References
- Orasmo CR, Ocanha JP, Barraviera SR, Miot HA (2014) Syndrome in question. An Bras Dermatol 89: 525-526.
- Debén Sánchez M, Veloso Rosendo M, Pérez Álvarez C, Pita Caaveiro (2003) Multiple simmetric lipomatosis: Report of two different clinical types and review of the literature. An Med Interna 20: 243-246.
- Vassallo GA, Mirijello A, Tarli C, Rando MM, Antonelli M, et al. (2019) Madelung’s disease and acute alcoholic hepatitis: case report and review of literature. Eur Rev Med Pharmacol Sci 23: 6272-6276.
- Szwec M, Sitarz R, Moroz N, Maciejewski R, Wierzbicki R (2018) Madelung’s disease-progressive, excessive, and symmetrical deposition of adipose tissue in the subcutaneous layer: A case report and literature review. Diabetes Metab Syndr Obes 11: 819-825.
- Chen K, He H, Xie Y, Zhao L, Zhao S, et al. (2015) miR-125a-3p and miR-483-5p promote adipogenesis via suppressing the RhoA/ROCK1/ERK1/2 pathway in multiple symmetric lipomatosis. Scientific Reports 5: 1-15.
- Ozderya A, Temizkan S, Aydin Tezcan K, Ozturk FY, Altuntas Y (2015) A case of Madelung's disease accompanied by Klinefelter's syndrome. Endocrinol Diabetes Metab Case Rep 2015.
- Berkovic SF, Andermann F, Shoubridge EA (1991) Mitochondrial dysfunction in multiple symmetrical lipomatosis. Ann Neurol 29: 566-569.
- Prantl L, Schreml J, Gehmert S, Klein S, Bai X, et al. (2016) Transcription profile in sporadic multiple symmetric lipomatosis reveals differential expression at the level of adipose tissue-derived stem cells. Plast Reconstr Surg 137: 1181-90.
- Ardeleanu V, Chicos S, Georgescu C, Tutunaru D (2013) Multiple benign symmetric lipomatosis - A differential diagnosis of obesity. Chirurgia 108: 580-583.
- Gao H, Xin ZY, Yin X, Zhang Y, Jin QL et al. (2019) Madelung disease: A case report. Medicine (Baltimore) 98: 3.
- Mimica M, Pravdic D, Nakas-Icindic E, Karin M, Babic E, et al. (2013) Multiple symmetric lipomatosis: A diagnostic dilemma. Case Rep Med 2013.
- Ouahabi HE, Doubi S, Lahlou K, Boujraf S, Ajdi F (2017) Launois-bensaude syndrome: A benign symmetric lipomatosis without alcohol association. Ann Afr Med 16: 33-34.
- Leung NWY, Gaer J (1978) Multiple symmetric lipomatosis: Effect of oral salbutamol. Clin Endocrinol 7: 601-606.
- Teplitsky V, Huminer D (1995) Multiple symmetric lipomatosis presenting with polyneuropathy. Isr J Med Sci 31: 693-695.
- Chun YC, Qing-Qing F, Xiao FW, Min-Xia Z, Wan-Yi Z, et al. (2018) Madelung’s disease: Lipectomy or liposuction?. Hindawi BioMed Research International 2018.
- Enzi G, Busetto L, Ceschin E, Coin A, Digito M, et al. (2002) Multiple symmetric lipomatosis: Clinical aspects and outcome in a long-term longitudinal study. Int J Obes Relat Metab Disord 26: 253-261.