Taha Yusuf Kuzan*, Ruslan Asadov, Rabia Ergelen and Davut Tuney
Marmara University School of Medicine, Istanbul, Turkey
Corresponding Author:
Taha Yusuf Kuzan
Department of Radiology
Marmara University Pendik Training and Research Hospital
Mimar Sinan Caddesi, No. 41, Ust Kaynarca
34899, Pendik, Istanbul, Turkey
Tel: +90-216-625-4545
Fax: +90-216-625-4639
E-mail: tykuzan@gmail.com
Received Date: October 22, 2016; Accepted Date: November 04, 2016; Published Date: November 11, 2016
Citation: Kuzan TY, Asadov R, Ergelen R, et al. Magnetic Resonance Imaging Findings of Isolated Hepatic Tuberculoma: A Diagnostic Dilemma. J Biomedical Sci. 2016, 6:1. doi:10.4172/2254-609X.100045
Copyright: © 2016 Kuzan TY. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Extrapulmonary tuberculosis; Liver tuberculosis; Hepatic tuberculoma; Hepatic mass; MRI
Introduction
Mycobacterium Tuberculosis (TB) is usually limited to the chest, but the disease might affect any organ system. Extrapulmonary tuberculosis constitutes 15.7-21% of all tuberculosis cases and less than 1% of all cases involving liver [1,2]. The most common form is the diffuse hepatic involvement seen along with pulmonary or miliary tuberculosis in 50-80% of patients dying of pulmonar tuberculosis. The second form is diffuse hepatic infiltration with small granulomas (less than 2 mm) without recognizable pulmonary involvement (granulomatous liver disease). The third much rarer form presents itself as a focal/local tuberculoma or abscess. Local hepatic tuberculosis, defined as tubercles>2 mm in diameter, usually occurs along with a tuberculous focus elsewhere. Isolated hepatic tuberculoma (synonyms nodular hepatic tuberculosis, macronodular hepatic tuberculosis) is the rarest form of local hepatic tuberculosis [3,4]. Isolated hepatic tuberculosis is granulomatous liver disease without pulmonary or bowel involvement. The imaging appearance of these lesions is considered to be nonspecific and can simulate metastases, abscess, and primary malignancy and thus, can mimic a number of other disease entities, and it is important to be familiar with the radiologic features to ensure early, accurate diagnosis [2-8]. Here we report a case of isolated hepatic tuberculoma mimicking solitary liver mass recovered with anti-TB treatment.
Case
A 40-year-old man patient with diagnosis of chronic renal failure presented with complaints of abdominal tenderness, fever, loss of appetite and weakness for a period of 4 months. Laboratory data revealed low Haemoglobin (Hb) level with normocytic normochromic red cells. The Erythrocyte Sedimentation Rate (ESR) was elevated. A normal white blood cell count, normal liver parenchyma function and normal coagulation tests were obtained. Creatinin (7.8 mg/dl) and Blood Urea Nitrogen (BUN) (46 mg/dl) were elevated. The patient was being treated by peritoneal dialysis for end stage renal disease.
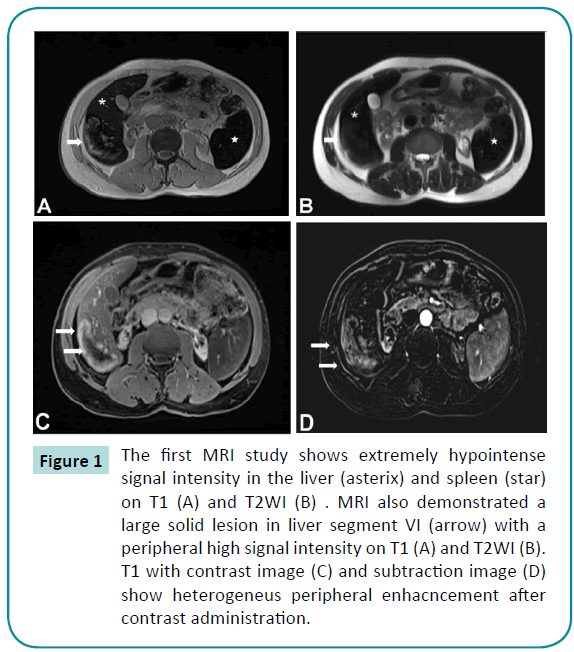
Ultrasound examination revealed that normal size liver with heterogeneous-hypoechoic mass affected focal lesion in segment 6, measuring 7×4 cm (not shown). The patient also had bilateral atrophic kidney and splenomegaly. After that, ?V contrastenhanced MRI was performed with a superconducting unit (Verio; Siemens, Germany) operating at a field strength of 3.0 T by using a body coil in order to characterize the lesion. MRI examination showed that 7×4 cm lession with centrally hypointense and peripherally hyperintes on both T1 and T2-weighted imaging in the segment 6 of liver (Figures 1A and 1B). The lesions had peripheral enhancement after contrast administration (Figures 1C and 1D). A diffuse signal reduction in the liver and spleen consistent with hemochromatosis and bilateral atrophic kidney were also seen on MRI.
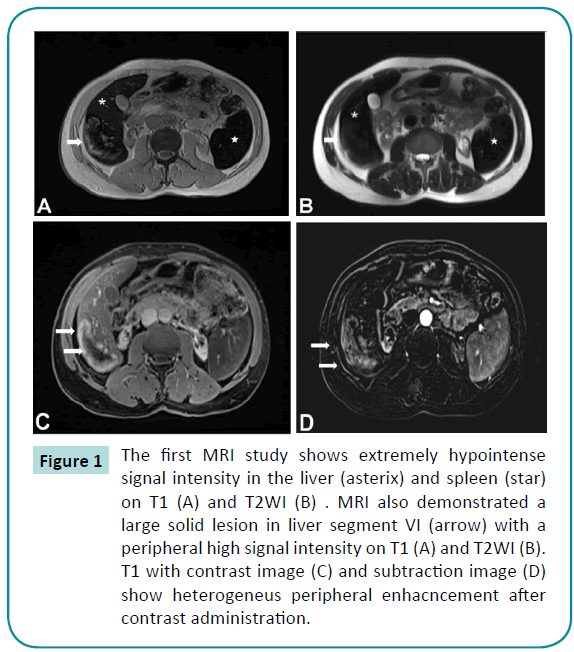
Figure 1: The first MRI study shows extremely hypointense signal intensity in the liver (asterix) and spleen (star) on T1 (A) and T2WI (B) . MRI also demonstrated a large solid lesion in liver segment VI (arrow) with a peripheral high signal intensity on T1 (A) and T2WI (B). T1 with contrast image (C) and subtraction image (D) show heterogeneus peripheral enhacncement after contrast administration.
Because of atypical MRI finding, ultrasound-guided biopsies were performed the liver lesion. Histopathological examination of the specimen showed multiple epithelioid cell granulomas without caseation necrosis and portal fibrosis. Acid-Fast Bacilli (AFB) could not be detected in smear examination, and Polymerase Chain Reaction (PCR) for Mycobacterium tuberculosis was negative in the biopsy specimen. A diagnosis of granulomatous hepatitis was made. Despite negative AFB and PCR, tuberculosis and sarcoidosis were considered in the differential diagnosis. The patient reported no history of tuberculosis or any contact with tuberculosis patient. Thorax Computed Tomography (CT) was within normal limits. The patient had no evidence of extrahepati tuberculosis or sarcoidosis at the time of diagnosis. The patient was clinically accepted to have localized hepatic TB.
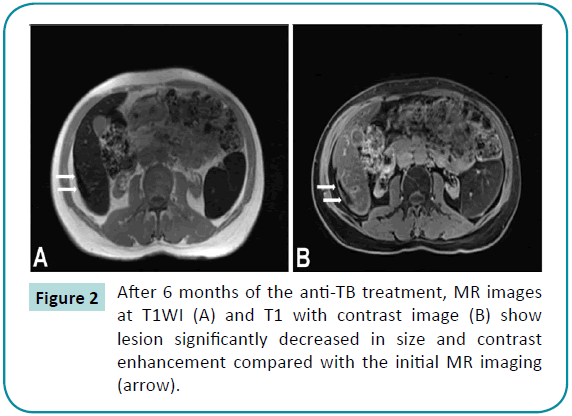
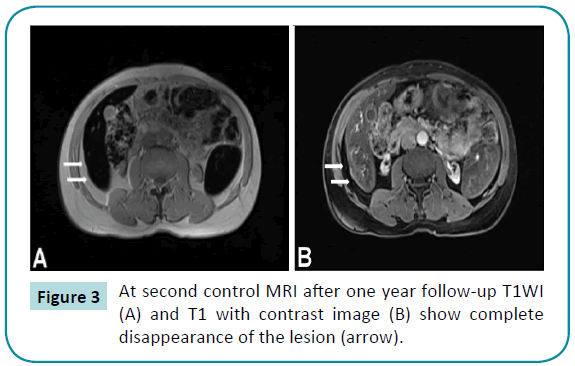
The patient was treated with a combination of rifampicin, isoniazid, ethambutol, and pyrazinamide for 6 months, It was observed that the patient recovered clinically and lesion regressed markedly (Figure 2) and after 6 of months anti-TB treatment, the lesion disappeared completely on the second control MRI (Figure 3).
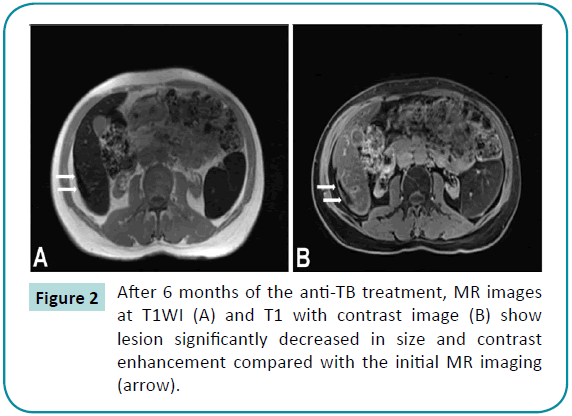
Figure 2: After 6 months of the anti-TB treatment, MR images at T1WI (A) and T1 with contrast image (B) show lesion significantly decreased in size and contrast enhancement compared with the initial MR imaging (arrow).
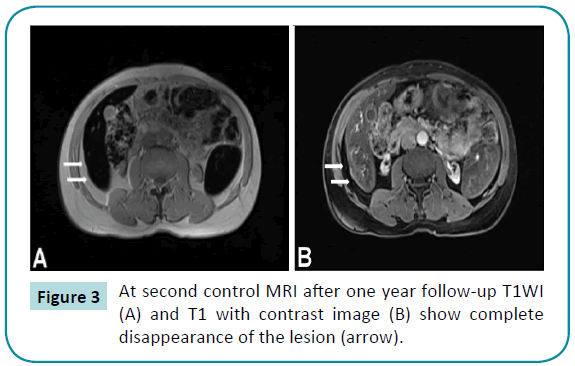
Figure 3: At second control MRI after one year follow-up T1WI (A) and T1 with contrast image (B) show complete disappearance of the lesion (arrow).
Discussion
Tuberculosis demonstrates a variety of clinical and radiologic features depending on the organ site involved. Liver involvement in tuberculosis is rare and classified into three categories: miliary, granulomatous and localized hepatic form. A few cases of reported isolated hepatic tuberculoma with ultrasonography, CT, and MRI findings were confirmed by biopsy [4-6,9-11].
The most common presenting symptoms of hepatic tuberculosis are right upper abdominal pain, upper abdominal tenderness, low-grade fever, weight loss, loss of appetite, and jaundice [5]. Similarly, our case presented abdominal tenderness, fever, loss of appetite and weakness.
The radiologic features of hepatic tuberculoma can mimic liver tumors, cholangiocarcinomas, liver abscess and hydatid cyst, or may present with various forms of systemic diseases like as collagen vascular disorders and hepatic involvement in systemic infections including viral infection, fungal infection, enteric fever [7-12].
Hepatic tuberculoma appears well-defined hypodense lesions with slight peripheral enhancement or no enhancement after IV contrast administration on CT [5,6,11]. At the early and medium stages of granuloma, the lesion may show a low signal intensity on T1-weighted imagings and a high signal intensity on T2-weighted MR imagings. Similar lesions with hypointense on T1-weighted imaging and hypo- and isointense on T2-weighted imagings were corresponding to fibrous stage of tuberculosis and may have slightly or no peripheral enhancement [5].
In our case, MRI examination showed a lession with centrally hypointense and peripherally hyperintes on both T1 and T2- weighted imaging and peripheral enhancement after contrast administration. In our patient, hemochromatosis may explain peripheral hyperintesity on both T1 and T2-weighted imaging which is incompatible with the literature cases [5].
Our patient had a tumor-like mass lesion of the liver on the abdominal US and MRI. To make a correct diagnosis, ultrasonography-guided percutaneous liver biopsy was performed, and histopathological examination revealed granulomatous hepatitis without caseation, suggestive of sarcoidosis and tuberculosis. Clinical and imaging findings of the patient were not consistent with sarcoidosis. Despite negative AFB and PCR, a diagnosis of isolated hepatic tuberculosis was made based on the presence of the granuloma and anti-TB treatment was started. After 6 months of treatment, the patient was asymptomatic and the lesion regressed markedly at MRI. On the follow-up after 6 months of the treatment, the lesion disappeared completely at the second MRI control.
Conclusion
The physical findings and imaging appearance of hepatic tuberculoma are considered to be nonspecific at US, CT and MRI that may cause diagnostic problems. Although US, CT and MRI can detect hepatic tuberculom, differential diagnosis with other masses (cystic, necrotic or infected metastases, fungal abscesses, lymphoma) may be difficult [2,5]. Because of that hepatic tuberculom is often misdiagnosed as liver cancer, liver abscess, benign tumor of liver, liver cysts, liver hydatid and so on [7]. For the accurate diagnosis of atypical liver lesions mimicing mass at radiologic imaging, a histopathological or bacteriological confirmation is often required.
17461
References
- Peto HM, Pratt RH, Harrington TA (2009) Epidemiology of extrapulmonary tuberculosis in the United States, 1993–2006. Clin Infect Dis 49:1350-1357.
- Mert A, Ozaras R, Tabak F (2003) Localized hepatic tuberculosis. Eur J Intern Med 14:511-12.
- Islam MR, Maksud M, Baral P (2015) Case Report of Isolated Hepatic Tuberculosis. Bangladesh Journal of Medicine 26:43-45.
- Yu RS, Zhang SZ, Wu JJ (2004) Imaging diagnosis of 12 patients with hepatic tuberculosis. World J Gastroenterol 10:1639-1642.
- Sheikh ASF, Qureshi IH, Saba K (2013) Primary isolated hepatic tuberculosis. J Coll Physicians Surg Pak 23:359-361.
- Ciftci A, TiryakiC, YaziciogluMB, CelaletinM, Haksal, et al. (2015)Macronodular hepatic tuberculosis mimicking hydatid cyst: A case report. IAIM 2: 203-206.
- Parsak CK, Hanta I, Aslan A (2008) Isolated hepatic tuberculosis presenting as cystic-like andtumour-like mass lesions. Case Rep Gastroenterol 2:18-21.
- Küçükmetin NT, ?nce Ü, Çiçek B (2014) Isolated hepatic tuberculosis: a rare cause of hepatic mass lesions. Turk J Gastroenterol25:110-112.
- Arora R, Sharma A, Bhowate P (2008) Hepatic tuberculosis mimicking Klatskintumor: a diagnostic dilemma. Indian J PatholMicrobiol 51:382.
- Senturk H, Kocer N, Papila C (1995) Primary macronodularhepatosplenic tuberculosis: two cases with US, CT, and MR findings. European Radiology 5:451-455.
- Mortelé KJ, Segatto E, Ros PR (2004) The Infected Liver: Radiologic-Pathologic Correlation 1. Radiographics 24:937-955.