Fernando A Herrera1,2*, Brennan RBS2, Karen M Horton2, Charles K Lee2, Rudolph Buntic2 and Gregory M Buncke2
1Department of Surgery, University of California, San Diego, California, USA
2The Buncke Clinic and Division of Microsurgery, California Pacific Medical Center, San Francisco, California, USA
Corresponding Author:
Fernando A Herrera
Department of Surgery
University of California
San Diego, California, USA
Tel: 6175042292
E-mail: fherrera@ucsd.edu
Received Date: November 03, 2016; Accepted Date: November 08, 2016; Published Date: November 15, 2016
Citation: Herrera FA, Brennan RBS, Horton KM, Lee CK, Buntic R, et al. Management of Hand and Digit Soft Tissue Injuries Using Free Fascia and Fasciocutaneous Flaps with Neo-Syndactylization. Arch Med. 2016, 8:6. doi:10.21767/1989-5216.1000172
Copyright: © 2016 Herrera FA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Trauma; Upper extremity; Syndactyly; Free flap
Introduction
Traumatic hand and digit injuries resulting in soft tissue loss can be a difficult and challenging problem for the reconstructive surgeon. These injuries may result in composite tissue loss to digits and require soft tissue coverage as well as bone, tendons, and nerves grafts. Coverage of exposed structures such as tendons, bones, vessels, or nerves at the dorsal and palmar surface of the hand requires thin, supple tissue to provide adequate range of motion and a satisfying aesthetic result. The use of local and regional flaps when possible to treat these injuries is a popular choice [1-5].
However due to the limited amount of expendable tissue in the hand this may result in a functional limitation at the donor site or simply may not be possible in due to the surrounding zone of injury. Free muscle flaps have been shown to be effective not only in covering these wounds but also at providing a well vascularized tissue that would decrease the risk of chronic infection of these vital structures [6,7]. Therefore muscle and musculocutaneous flaps in microsurgical reconstruction have been widely used to cover such upper extremity defects in the past [8-12].
However, with the advancement in microsurgical techniques the use of free fasciocutaneous and fascial flaps allow for more appropriate replacement of similar tissues allowing for improved range of motion and a more aesthetically pleasing appearance of the traumatized upper extremity [13-16].
When multiple adjacent fingers require soft tissue coverage these flaps can be placed over the entire defect creating artificially syndactylized digits. This allows for complete coverage of all defects using one free flap. However this would require a staged procedure for flap division after adequate neovascularization has occurred. We discuss our experience with free fascia and fascio-cutaneous flaps for soft tissue coverage of traumatic hand and digit injuries with neo-syndactylization and the timing of flap division.
Patients and Methods
The authors retrospectively reviewed 13 consecutive free fascia and fasciocutaneous flaps to the hand and digits with neosyndactylization of adjacent digits for traumatic soft tissue loss from 1991 to 2005. Patient charts and operative reports were reviewed.
The indications for free tissue transfer, anatomical site of injury, type of flap performed, patient age, time to flap division, and early postoperative complications were analyzed. Outcomes assessed were flap failure, partial flap necrosis, wound infection, donor site complications, need for further surgeries after flap division, and length of hospital stay after initial free tissue transfer.
Results
Thirteen microvascular free flaps were performed in 13 patients. Twelve patients were male, one female with a mean age of 36.2 years (range 19 to 79 years). The soft tissue defects were located on the dorsal surface in 9 patients, and volar surface in 4 patients. How many digits where on the hand/ fingers were the injuries? Microsurgical free tissue transfers included 10 fascio-cutaneous flaps and three fascial flaps (Table 1).
| Patient |
Age |
Sex |
Type of injury |
Type of flap |
Time from injury to initial flap (days) |
Time to division(s) |
Early complications |
| 1 |
41 |
F |
Crush/Burn |
RFFC |
10 |
20 days |
no |
| 2 |
20 |
M |
Crush |
DTF |
7 |
56 days |
yes |
| 3 |
35 |
M |
Crush/Burn |
RFFC |
|
90d/150d |
no |
| 4 |
41 |
M |
Crush/Burn |
RFFC |
3 |
23d/57d |
yes |
| 5 |
79 |
M |
Degloving |
ALT |
5 |
69 days |
no |
| 6 |
19 |
M |
Degloving |
RFF |
2 |
89days |
no |
| 7 |
44 |
M |
Crush |
RFFC |
|
61days |
no |
| 8 |
18 |
M |
Crush |
RFFC |
7 |
24days |
no |
| 9 |
41 |
M |
Crush |
RFFC |
10 |
24d/42d |
no |
| 10 |
35 |
M |
Crush/Burn |
DTF |
|
49days |
no |
| 11 |
44 |
M |
Degloving |
RFFC |
|
78 days |
no |
| 12 |
23 |
M |
Crush |
RFFC |
4 |
122 days |
no |
| 13 |
30 |
M |
Degloving |
RFFC |
26 |
86d/202d |
yes |
Table 1: Microsurgical free tissue transfers.
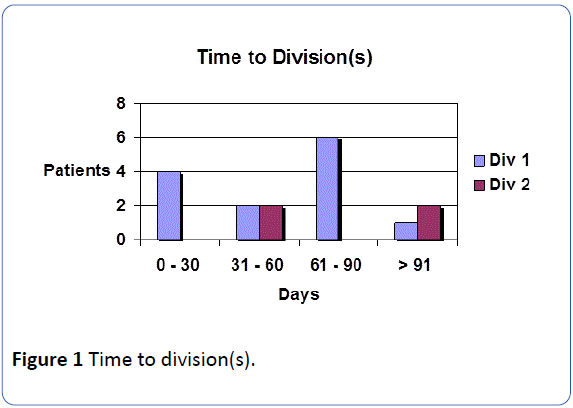
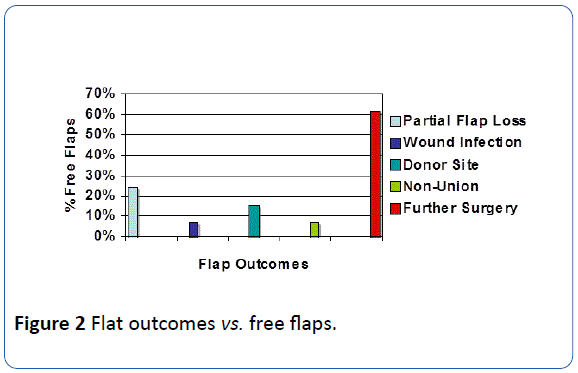
Of these nine were radial forearm fascio-cutaneous flaps (69.2%), one anterolateral thigh fascio-cutaneous flap (7.7%), two dorsal thoracic fascial flaps (15.4%), and one radial forearm fascial flap (7.7%). The mean time from injury to flap coverage was 8.2 days (2 to 26 days) and the average length of hospital stay was 7.6 days (6 to 10 days). Outcomes included partial flap necrosis in 3 patients, one superficial wound infection, and 2 donor site complications. Of the patients that developed partial flap necrosis, 2 occurred prior to flap division and one after flap division. One patient required a second flap for coverage while the other 2 were treated with debridement and flap advancement. The one patient who developed superficial wound infection was treated with debridement and oral antibiotics. The donor site complications included one early partial loss of split thickness skin graft of the donor site which healed and one late contracture at the donor site requiring scar revision, tenolysis, and flap advancement. Nine patients underwent a single stage desyndactylization procedure while the remaining four patients underwent a two-stage flap division (Table 2). The mean time to primary flap division was 61 days (range 20-122 days). The mean time to secondary flap division was 113 days (42 to 202 days). Four patients underwent primary de-syndactylization with the first 30 days post microsurgical transfer. Of these, one developed partial flap necrosis at the division site requiring further debridement and flap advancement for wound closure. The remaining 10 patients underwent flap division at more than 30 days, none of which developed flap loss (Figure 1). Timing of flap division was determined by surgeon preference and not based on flap size or type. Two patients required debulking procedures and 6 required tenolysis for improved range of motion.
| Location of injury |
Radial forearm fasciocutaneous |
Dorsal thoracic fascial flap |
Anterior lateral thigh flap |
Radial forearm fascia flap |
| Volar Injuries |
3 |
- |
- |
1 |
| Dorsal Injuries |
6 |
2 |
1 |
- |
Table 2: Location of injury and type of flap performed.
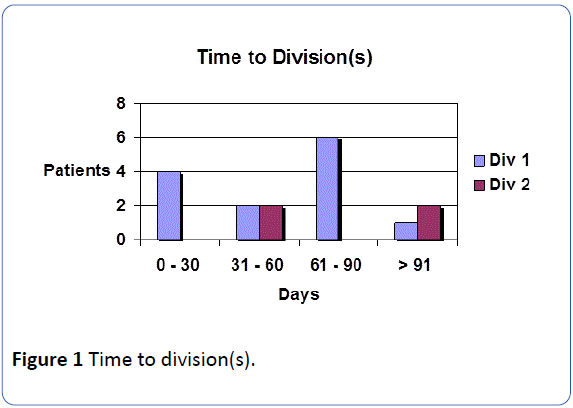
Figure 1: Time to division(s).
Case Presentations
Case 1
A 18-year right hand dominant male suffered an automobile accident resulting in complex degloving injury of the volar surface of his left middle and ring finger with open fracture of the distal phalanx of the middle finger (Figure 2). He underwent immediate irrigation and open reduction internal fixation of the phalanx fracture and placement of a vacuum closure device to temporarily cover the soft tissue defect. The patient was taken back to the operating theatre several days later. A free radial fascial flap with split thickness skin graft to the ipsilateral hand was performed with neo-syndactylization of the affected digits. The flap survived without complications and the patient underwent division of the neo-syndactylized digits at 89 days from the original procedure without further complications or secondary procedures needed.
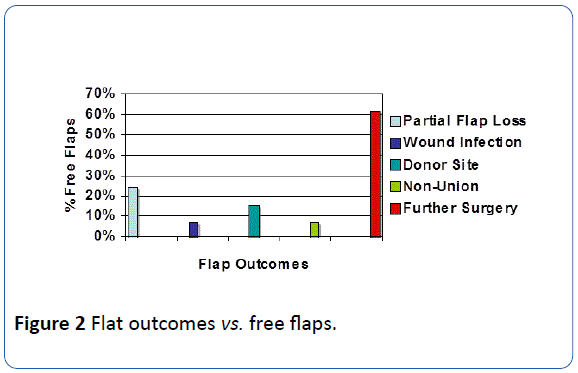
Figure 2: Flat outcomes vs. free flaps.
Case 2
A 79-year-old male right hand dominant male suffered a lawn mower accident resulting in severe mutilating injury to the dorsal surface of his right hand and index through small fingers. He underwent immediate irrigation and debridement with skeletal stabilization and application of vacuum assisted closure. Definitive soft tissue coverage was completed using an anterior lateral thigh flap with neo-syndactylization of the affected digits. Postoperatively the flap survived without complications. Flap division was completed at 69 days from the original flap procedure without complications or need for further surgeries.
Discussion
Reconstruction of hand and digit injuries after traumatic soft tissue loss resulting in exposed vital structures posses a challenge to the reconstructive surgeon. Many flaps have been described to cover such defects and allow for proper management of these devastating injuries [1-5]. Local flaps can be used to provide coverage for small defects; however the limited arc of rotation and extensive zone of injury produced by these injuries limits their use. Many authors recommend coverage with well vascularized tissue, such as musculocutaneous flaps when infection, scarring, or previous radiation compromises the wound bed [6,7]. With the advancement in technology and microsurgical training we have improved our ability to care for such injuries and provide adequate soft tissue coverage by replacing like with like tissue. The use of free fascia and fasciocutaneous flaps has allowed for a more contoured and supple soft tissue coverage in upper extremity trauma. These flaps allow for improved range of motion and improved aesthetic appearance [13-16]. In our series we performed 9 radial forearm fascio-cutaneous flaps from the contralateral arm, one anterior-lateral thigh flap, two dorsal thoracic fascia, and one radial forearm fascia flap with split thickness skin graft. All of our patients required further procedures for division of neo-syndactylization and reshaping of individual digits covered by these flaps. The timing and staging of flap divisions were based on surgeon preference and patient availability.
Although many papers have been written on the subject, the exact timing at which free flaps become independent of their vascular pedicle remains unclear. Oswald et al. [17] showed that occlusion of the vascular pedicle in micro vascular free flaps performed in rats, on the 5th day resulted in survival of the flap. With the exception of anecdotal reports, most of the published literature suggests that free flaps in humans are dependent on their pedicle for at least 15 to 17 days [18-22]. The condition and quality of the recipient site plays a large role in survival of these flaps. Ischemic, irradiated, and scarred beds are inadequate in providing late flap neovascularization, compared to healthy recipient sites and therefore would be dependent on the vascular pedicle for longer periods of time [23,24]. In our series all wounds were secondary to acute trauma. The average time to free flap coverage from initial injury was 8.2 days. Early coverage of these wounds is associated with a decreased incidence of infection and early neovascularization of the newly transferred tissue. The average time to primary flap division in our series was 61 days. Four patients underwent primary flap division within 30 days of the original microvascular transfer. Of these only one patient developed partial flap necrosis early after flap division. No other complications followed primary or secondary flap division [25,26]. Although several studies suggest that flaps become independent of their vascular pedicle at 15 days after tissue transfer, several factors affect the proper timing of flap division. We feel that the appropriate timing depends on overall clinical assessment including flap edema, evidence of superficial wound infection and overall wound healing status.
Keywords
- Giessler GA, Erdmann D, Germann G (2003) Soft tissue coverage in devastating hand injuries. Hand Clin 19: 63-67.
- Neumeister MW, Brown RE (2003) Mutilating hand injuries: principles and management. Hand Clin 19: 1-15.
- Weinzweig N, Chen L, Chen ZW (1994) The distally based radial forearm fasciosubcutaneous flap with preservation of the radial artery: an anatomic and clinical approach. PlastReconstrSurg 94: 675-684.
- Meland NB, Lincenberg SM, Cooney WP, Wood MB, Hentz VR (1989) Experience with the island radial forearm flap in local hand coverage. J Trauma 29: 489-493.
- Mandrekas AD, Zambacos GJ (1994) Reverse-flow radial forearm flap for reconstruction of the hand. Ann PlastSurg 33: 536-543.
- Calderon W, Chang N, Mathes SJ (1986) Comparison of the effect of bacterial inoculation in musculocutaneous and fasciocutaneous flaps. PlastReconstrSurg 77: 785-794.
- Anthony JP, Mathes SJ, Alpert BS (1991) The muscle flap in the treatment of chronic lower extremity osteomyelitis: results in patients over 5 years after treatment. PlastReconstrSurg 88: 311-318.
- Hing DN, Buncke HJ, Alpert BS, Gordon L (1985) Free flap coverage of the hand. Hand Clin 1: 741-758.
- Kerrigan CL, Daniel RK (1986) Free tissue transfers to the upper extremity. OrthopClin North Am 17: 383-394.
- Breidenbach WC (1989) Emergency free tissue transfer for reconstruction of acute upper extremity wounds. ClinPlastSurg 16: 505-514.
- Rao VK, Baertsch A (1994) Microvascular reconstruction of the upper extremity with the rectus abdominis muscle. Microsurgery 15: 746-750.
- Press BH, Chiu DT, Cunningham BL (1990) The rectus abdominis muscle in difficult problems of hand soft tissue reconstruction. Br J PlastSurg 4: 419-425.
- Reyes FA, Burkhalter WE (1988) The fascial radial flap. J Hand Surg Am 13: 432-437.
- Chen HC, el-Gammal TA (1997) The lateral arm fascial free flap for resurfacing of the hand and fingers. PlastReconstrSurg 99: 454-459.
- Wong SS, Wang ML, Su MS, Wei FC (1999) Free medialispedis flap as a coverage and flow-through flap in hand and digit reconstruction. J Trauma 47: 738-743.
- Flugel A, Kehrer A, Heitmann C, Germann G, Sauerbier M (2005) Coverage of soft-tissue defects of the hand with free fascial flaps. Microsur 25: 47-53.
- Oswald P, Tilgner A, Schumann D (1988) The influence of postoperative vessel occlusion on the viability of free microvascular skin-fat flaps and island flaps in rats. J ReconstrMicrosurg 4: 403-407.
- Gatti JE, LaRossa D, Brousseau DA, Silverman DG (1984) Assessment of neovascularization and timing of flap division. PlastReconstrSurg 73: 396-402.
- Chen HC, Tan BK, Cheng MH, Chang CH, Tang YB (2002) Behavior of free jejunal flaps after early disruption of blood supply. Ann ThoracSurg 73: 987-989.
- Millican PG, Poole MD (1985) Peripheral neovascularisation of muscle and musculocutaneous flaps. Br J PlastSurg 38: 369-374.
- Tsur H, Daniller A, Strauch B (1980) Neovascularization of skin flaps: route and timing. PlastReconstrSurg 66: 85-90.
- Clarke HM, Chen GZ (1992) Peripheral neovascularization of muscle and musculocutaneous flaps in the pig. PlastReconstrSurg 89: 109-113.
- Morris SF, Yang D (1999) Effect of vascular delay on viability, vasculature, and perfusion of muscle flaps in the rabbit. PlastReconstrSurg 104: 1041-1047.
- Gonzalez MH, Weinzweig N (2005) Muscle flaps in the treatment of osteomyelitis of the lower extremity. J Trauma 58: 1019-1023.
- Salgado CJ, Smith A, Kim S, Higgins J, Behnam A, et al. (2002) Effects of late loss of arterial inflow on free flap survival. J ReconstrMicrosurg 18: 579-584.
- Ceulemans P, Van Landuyt K, Hamdi M, Blondeel P, Matton G, et al. (2001) Complete survival of a free flap after early pseudoaneurysm formation and pedicle thrombosis. Ann PlastSurg 47: 332-335.
17448