Hamdi Louati*, Riadh Jouini, Awatef Charieg, Ines Chouchen, Yosra Ben Ahmed, Faouzi Nouira and Said Jlidi
Department of Pediatric Surgery, Children Hospital, Tunis, Tunisia
Corresponding Author:
Hamdi Louati
Department of Pediatric Surgery
Children Hospital, Tunis, Tunisia
Tel: 0021652225719
E-mail: drhamdilouati85@yahoo.com
Received Date: October 06, 2016; Accepted Date: November 15, 2016; Published Date: November 22, 2016
Citation: Louati H, Jouini R, Charieg A, Chouchen I, Ahmed YB, et al. Meckel’s Diverticulum Complications in Chirldren: Results of a 51 Cases Unicentric Series. Arch Med. 2016, 8:6. doi:10.21767/1989-5216.1000175
Copyright: © 2016 Louati H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Objective: The aim of this study is to investigate the diagnosis and the treatment options of complicated Meckel’s diverticulum and compare that with the literature.
Material and Methods: This study retrospectively evaluated 51 patients who had been operated on for complicated Meckel’s diverticulitis in our department of Pediatric Surgery, between January 1999 and February 2016. Clinical symptoms, signs, radiologic data and therapeutic management were retrieved.
Results: A total of 51 children with a diagnosis of complicated Meckel’s diverticulitis (MD) were retrospectively analysed. The reason for consultation was an occlusive syndrome in 28 patients (55%), rectal bleeding or melena in 18 patients (35%) and isolated abdominal pain in 5 patients (10%). Abdominal ultrasound was performed in 49 patients, it was normal in 37% and it has objectified an intussusception in 26.5% of cases. All patients were operated. The way was a McBurney incision 45%, a midline laparotomy 21.5% and laparoscopic 33.5% of cases. The intra-operative diagnoses of MD complications were diverticulum perforation in 13.5%, mechanical intestinal obstruction due to diverticulum in 6%, diverticulum invagination in 21.5%, diverticulitis in 31.5%, volvulus in 3%, one attached to the hernia sac in Littre’s hernia and 21.5% appeared macroscopically healthy in intraoperative. All patients had partial small bowel resection and end-to-end anastomosis. Histopathologic ectopic tissue revealed: 21 gastric mucosa (41%), 3 pancreatic tissues (6%), 12 jejunal tissues (23.5%) and no heterotopic focus in 5 patients (10%).
Conclusion: Meckel’s diverticulitis does not have specific clinical and radiological findings. Surgical intervention is the only treatment and laparoscopy is increasingly used.
Keywords
Meckel’s diverticulum; Children; Diagnosis; Treatment
Introduction
Meckel’s diverticulum is a true diverticulum containing all layers of bowel wall located in the ileum anti-mesenteric border. It results from non-closure of the omphalo-mesenteric canal, which is supposed to obliterate in the 5th-7th gestational weeks [1]. Complicated MD varies considerably in clinical presentation, including intussusception, volvulus, internal hernia, adhesion, Littre hernia, gastrointestinal bleeding, diverticulitis, and perforation [2]. This study aimed to investigate the diagnosis and the treatment options and compare that with the literature.
Material and Methods
This study retrospectively evaluated 51 patients who had been operated on for complicated Meckel’s diverticulitis in our department of Pediatric Surgery between January 1999 and February 2016. Clinical symptoms, signs, radiologic data and therapeutic management were retrieved.
Results
Over 18 years period, we diagnosed and managed 51 children with complicated MD. The average age of our patients was 3 years 7 months of age with extremes ranging from 12 days to 14 years. 24 patients (47%) were aged less than 2 years and 14 patients (27.5%) were older than 5 years. They were 43 males and 8 females (sex ratio of 5.4).
The reason for consultation was an occlusive syndrome in 28 patients (55%), rectal bleeding or melena in 18 patients (35%) and isolated abdominal pain in 5 patients (10%).
Abdominal ultrasound was performed in 49 patients. It was normal in 18 cases (37%) it has objectified an intussusception in 13 cases (26.5%), peritoneal effusion in 11 cases (22%), intestinal distention in 4 cases, a cannulated structure hypoechoic connects the umbilicus to the gastrointestinal tract in one case and an intestinal thickening with infiltration in 2 cases. 99mTc scan was performed in 17 cases and allowed to visualize a focus of increased uptake in the small intestine in 13 cases.
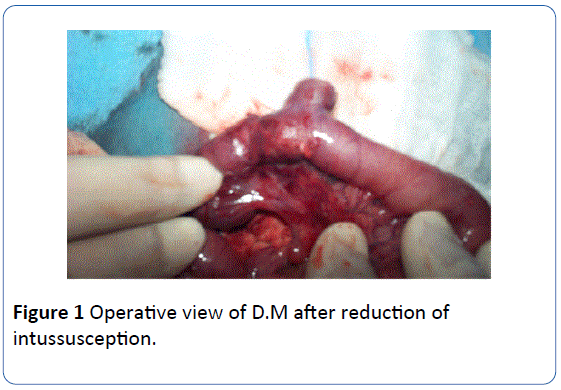
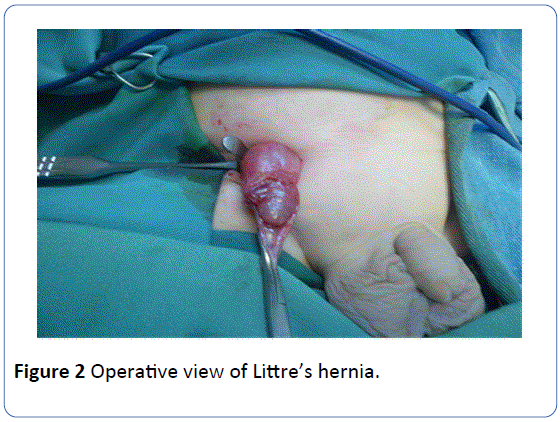
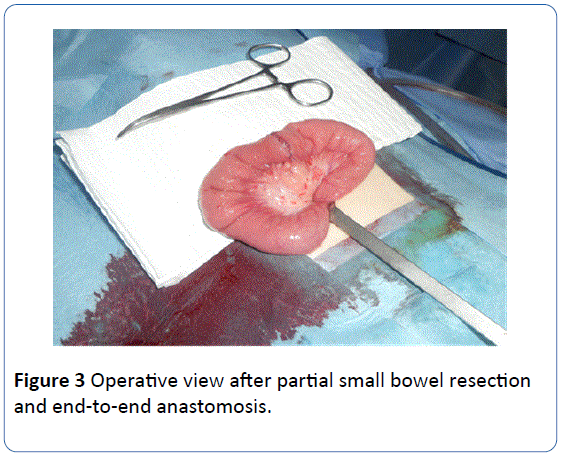
All patients were operated. The way was a McBurney incision in 23 cases (45%), a midline laparotomy in 11 cases (21.5%) and laparoscopic in 17 cases (33.5%). The intraoperative diagnoses of MD complications were diverticulum perforation in 7 patients (13.5%), mechanical intestinal obstruction due to diverticulum in 3 cases (6%), diverticulum invagination (Figure 1) in 11 patients (21.5%), diverticulitis in 17 cases (31.5%), volvulus in one case (3%), one attached to the hernia sac in Littre’s hernia (Figure 2) (3%) and 11 appeared macroscopically healthy in intraoperative (21.5%). All patients had partial small bowel resection and end-to-end anastomosis (Figure 3).
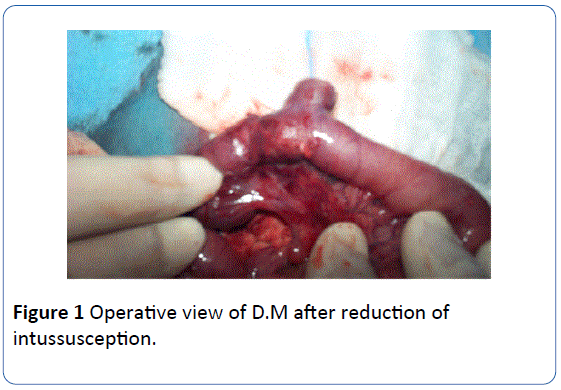
Figure 1: Operative view of D.M after reduction of intussusception.
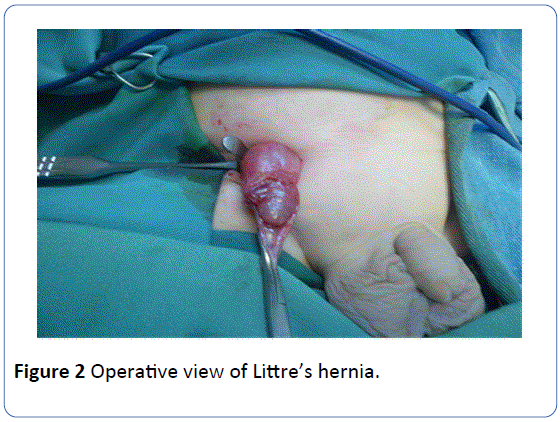
Figure 2: Operative view of Littre’s hernia.
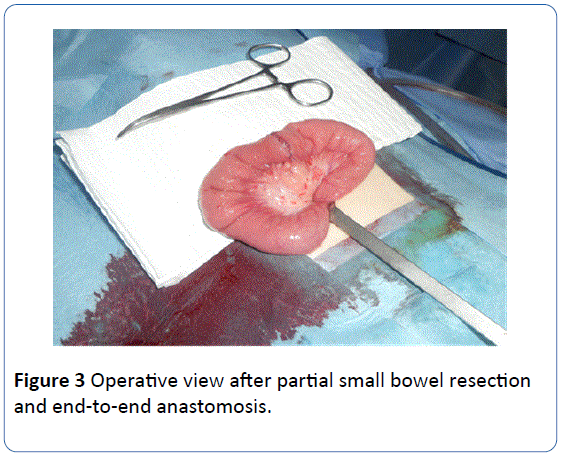
Figure 3: Operative view after partial small bowel resection and end-to-end anastomosis.
The histopathologic mean diverticular size was 4.3 cm (1.5-8 cm). The distance DM ileocecal valve has been proposed in 42 patients. It varied between 10 cm and 100 cm with an average of 49.8 cm. Histopathologic ectopic tissue revealed: 21 gastric mucosa (41%), 3 pancreatic tissues (6%), 12 jejunal tissues (23.5%) and no heterotopic focus in 5 patients (10%). In 10 patients (19.5%), the diverticulum mucosa could not be assessed due to necrosis and intense inflammation.
45 patients were discharged after an uneventful progress and 6 were discharged after management of postoperative complications (fever in 4 patients and occlusive syndrome in 2 patients). Long term outcome was favourable with a variable back from 2 months to 13 years 4 months.
Discussion
MD is the most common congenital abnormality of the gastrointestinal system [3]. First described by Hildanus [4], the German anatomist Johann Friedrich Meckel’s defined this pathology embryological and named it in 1809. It had a prevalence rate of 2% in the general population [5]
The incidence of symptomatic presentation has been more difficult to elucidate, several single institution series and retrospective reviews have studied the natural course of MD and determined that the incidence of symptomatic presentation ranges between 17%-54% [6,7]. In our series, we identified 51 cases of complicated DM over a period of 18 years or 2.83 cases per year. There is a male predominance. The male/female ratio was reported to be 3/1 in a study from Mayo including 1476 patients [8]. Our series show similar male preponderance.
Symptomatic patients although complicated, are usually diagnosed “on-table.” Although without an objective piece of evidence, the complications are said to be more frequent in males than females, with the lifetime risk of 6.4% [9,10]. Some have reported that younger patients in the pediatric population with symptomatic MD are more prone to present with obstructive symptoms [8,11]. In secondary intussusception, MD is the most common lead point [12]. In our series the frequency of complications during the first two years of estimated life 47% how is almost consistent with the literature data. In this study 21.5% of cases associate MDintussusception
Radiological diagnosis of MD can be difficult, particularly when the diagnosis is not initially suspected. Ultrasound is often used in the setting of non-specific abdominal pain; however, it is of limited value for diagnosing MD except in the case of intussusception [13]. In our study ultrasound objectified an intussusception in 13 cases. CT was considered of little interest in diagnosing Meckel’s diverticulum because of its suspected incapacity to differentiate the diverticulum from a loop of small bowel [14]. The CT pattern associated with the presence of Meckel’s diverticulum is that of an outpouching blind-ended digestive structure arising from the antimesenteric side of the terminal ileum; this structure is found in the right lower quadrant or lower abdomen and is connected to the small bowel by a neck of varying caliber [15,16]. The 99mTc scan, or Meckel’s scan, is generally regarded as the most accurate, non-invasive diagnostic technique searching for gastric ectopic tissue. However, falsenegative rates are higher in patients without bleeding [17]. Scintigraphy with Tc-99 m-labelled red blood cells is the most sensitive imaging method to detect active gastrointestinal haemorrhage with bleeding rates as low as 0.1 ml/min [18].
Complicated MD should be treated by surgical resection. The choice of surgical techniques depends on the external appearance of MD [17,19]. Resection is recommended for treatment of complicated MD, whereas this issue is controversial for patients with incidental findings. In their epidemiologic study Cullen et al. suggest routine resection to all incidental MD’s under the age of 80 years. Herein, early laparoscopy can pinpoint the diagnosis and drastically reduce the access trauma, allowing these patients to enjoy a markedly reduced postoperative morbidity, without compromising on cosmetic appearance [20]. In our study in the last years laparoscopy had become most used because it permits the easy diagnosis and identification of the diverticulum and reduces postoperative complications and hospitalization period.
The diverticulum usually occurs within 100 cm of the ileocecal valve in the anti-mesenteric border of ileum. The diverticulum has various sizes up to 15 cm in length [21]. Patients with diverticular length greater than 2 cm were more prone to develop symptoms according to the Mayo Clinic survey [8]. Some studies have also documented that a long or thin based MD is more likely to develop symptoms than a short or broad-based one [22,23].
Ectopic tissues have been detected in 31% to 85% of symptomatic MD in previous pediatric series [8,11,24]. Diverticula containing gastric mucosa are more responsible for symptoms. The remaining ectopic tissue can be seen in the following rates; pancreatic tissue in 6%, combination of pancreatic tissue and gastric mucosa 5%, jejunal mucosa 2%, Brunner gland 2% and combination of gastric and duodenal mucosa 2% [24]. In our study the most ectopic tissue was gastric mucosa.
Conclusion
Complicated MD in child is usually present with bleeding, intestinal obstruction, abdominal pain, diverticulum perforation or intussusception. It remains a challenge in diagnosis before operation. The surgical treatment is partial small bowel resection and end-to-end and laparoscopy must be considered as the technique of choice in the management of complicated MD.
17526
References
- Peoples JB, Lichtenberger EJ, Dunn MM (1995) Incidental Meckel'sdiverticulectomy in adults.Surgery 118: 649-652.
- Rosai J (2004) Gastrointestinal Tract. In: Surgical Pathology.( 9th edtn), Elsevier publishing, New York, USA.
- Uppal K, Tubbs RS, Matusz P, Shaffer K, Loukas M (2011) Meckel's diverticulum: a review.ClinAnat 24: 416-422.
- Opitz JM, Schultka R, Göbbel L (2006) Meckel on developmental pathology.Am J Med Genet A 140: 115-128.
- Moore TC (1996) Omphalomesenteric duct malformations.SeminPediatrSurg 5: 116-123.
- Soltero MJ, Bill AH (1976) The natural history of Meckel's diverticulum and its relation to incidental removal. A study of 20 cases of diseased Meckel's diverticulum found in King County, Washington, over a fifteen year period.Am J Surg 132: 168-173.
- Mackey WC, Dineen P (1983) A fifty year experience with Meckel's diverticulum.SurgGynecolObstet 156: 56-64.
- Park JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR (2005) Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002).Ann Surg 241: 529-533.
- Arnold JF, Pellicane JV (1997) Meckel's diverticulum: a ten-year experience.Am Surg 63: 354-355.
- Cullen JJ, Kelly KA, Moir CR, Hodge DO, Zinsmeister AR, et al. (1994) Surgical management of Meckel's diverticulum. An epidemiologic, population-based study.Ann Surg 220: 564-568.
- Tseng YY, Yang YJ (2009) Clinical and diagnostic relevance of Meckel's diverticulum in children.Eur J Pediatr 168: 1519-1523.
- Lehnert T, Sorge I, Till H, Rolle U (2009) Intussusception in children--clinical presentation, diagnosis and management.Int J Colorectal Dis 24: 1187-1192.
- Thurley PD, Halliday KE, Somers JM, Al-Daraji WI, Ilyas M, et al. (2009) Radiological features of Meckel's diverticulum and its complications.ClinRadiol 64: 109-118.
- Rossi P, Gourtsoyiannis N, Bezzi M, Raptopoulos V, Massa R, et al. (1996) Meckel's diverticulum: imaging diagnosis.AJR Am J Roentgenol 166: 567-573.
- Bennett GL, Birnbaum BA, Balthazar EJ (2004) CT of Meckel's diverticulitis in 1 patients.AJR Am J Roentgenol 182: 625-629.
- Elsayes KM, Menias CO, Harvin HJ, Francis IR (2007) Imaging manifestations of Meckel's diverticulum.AJR Am J Roentgenol 189: 81-88.
- Robijn J, Sebrechts E, Miserez M (2006) Management of incidentally found Meckel's diverticulum a new approach: resection based on a Risk Score.ActaChirBelg 106: 467-470.
- Graça BM, Freire PA, Brito JB, Ilharco JM, Carvalheiro VM, et al. (2010) Gastroenterologic and radiologic approach to obscure gastrointestinal bleeding: how, why, and when? Radiographics 30:235–252.
- Varcoe RL, Wong SW, Taylor CF, Newstead GL (2004) Diverticulectomy is inadequate treatment for short Meckel's diverticulum with heterotopic mucosa.ANZ J Surg 74: 869-872.
- Rangarajan M, Palanivelu C, Senthilkumar R, Madankumar MV (2007) Laparoscopic surgery for perforation of Meckel's diverticulum.Singapore Med J 48: e102-e105.
- Lüdtke FE, Mende V, Köhler H, Lepsien G (1989) Incidence and frequency or complications and management of Meckel's diverticulum.SurgGynecolObstet 169: 537-542.
- DiGiacomo JC, Cottone FJ (1993) Surgical treatment of Meckel's diverticulum.South Med J 86: 671-675.
- Feller AA, Movson J, Shah SA (2003)Meckel diverticulum: a geriatric disease masquerading as common gastrointestinal tract disorders. Arch Intern Med 163:2093-2096.
- Durakbasa CU, Okur H, Mutus HM, Bas A, Ozen MA, et al. (2010) Symptomatic omphalomesenteric duct remnants in children.PediatrInt 52: 480-484.