Introduction
Ultimate health and maximal life span requires metabolic harmony and nutrient abundance.[1] In order for the body’s cellular machinery to function properly, an adequate amount of bioavailable nutrients plus a myriad of other essential substrates must always be available. Recommended Daily Allowance (RDA) amounts of vitamins and minerals do little to prevent the epidemic of chronic degenerative diseases. RDA’s were first introduced in the 1930’s for the purpose of reducing scurvy, rickets, and pellagra. Today, however, RDA’s are a confusing and misleading standard, causing many people to think that if they consume the RDA amounts of vitamins and minerals, they’re doing all that’s necessary to be healthy. This is clearly false and damaging to a misguided and suffering population.[2] Air pollution, contaminated sources of water, radiation, over-processed foods, depleted soils, toxic chemicals, and prescriptive drugs effect nutrient needs making RDA suggestions and nutritionist’s meal plans woefully inadequate.
Macronutrient and micronutrient deficiencies are very common in the general population – it is estimated that over 1 billion people worldwide are vitamin D deficient, or at least insufficient.[3] Overall it has been established by the scientific community that approximately 70 percent of the U.S. population is at risk for long-term vitamin and mineral deficiencies.[4] Some individual nutrient levels will predictably low in patients who are fighting active disease due to increased demand, but coupled with genetic predisposition issues and a myriad of other issues, levels can easily become pathological. Micronutrient deficiencies are insidious usually, and recommendations for vitamin and mineral supplementation for the apparently healthy are often disregarded as superfluous. It is unlikely that anyone ever has sufficient levels of essential micronutrients at all times to meet the unpredictable demands of the body defense systems. Intuitively, it might seem that a low single nutrient level would make little difference in the whole scheme of life. However, when just one cellular request goes unfilled repercussions are felt throughout the entire body and can lead to a myriad of acute and chronic disease states.
Unfortunately, body reserves of vitamins and minerals do not have to be even “out of the reference range” or “significantly low” in order to cause problems.[5] “Evidence suggests that metabolic damage occurs at intake amounts between the level causing micronutrient deficiency diseases and the recommended dietary allowances (RDA). This may result in an increase in DNA damage, neuronal or mitochondrial decay that could lead to accelerated aging, cancers, and degenerative diseases.[6] Dr. Bruce Ames, a respected biochemist from the University of California, Berkeley, showed that low levels of micronutrients (vitamins and minerals) at the cellular level may actively promote DNA and protein damage and cause disease to a larger extent than is generally realized. The optimum amount of vitamins and minerals that are truly required is the amount that minimizes DNA damage and maximizes a healthy life span, which is higher than the amount to prevent acute disease.[7] Dr. Ames suggests that vitamins and minerals play a critical role as cofactors in enzyme reactions that protect genes from mutations and repair gene damage. Thus, certain micronutrients can act prophylactically, and also therapeutically.
Numerous clinical trials have evaluated the use of nutritional supplements such as beta-carotene, selenium, vitamin C and vitamin E in the prevention of coronary heart disease and stroke yielding conflicting results (positive, neutral and negative). In many of these clinical trials there were enormous clinical design problems, methodological flaws, varied patient populations, variable doses and type of vitamin use, improper selection of vitamins used and many other issues that make the studies difficult to interpret.[8] The MOST study is the first to run the methodological gauntlet, solving the clinical design and therapeutic challenges that others haven’t. This pilot study produced encouraging and exciting results, and established the viability, and capabilities of this revolutionary research tool. The MOST methodology should be utilized to modernize recommended daily allowances, improve tolerance and safety data, promote new focus into micronutrient research studies, and become a formidable foe of chronic and acute disease.
Methods
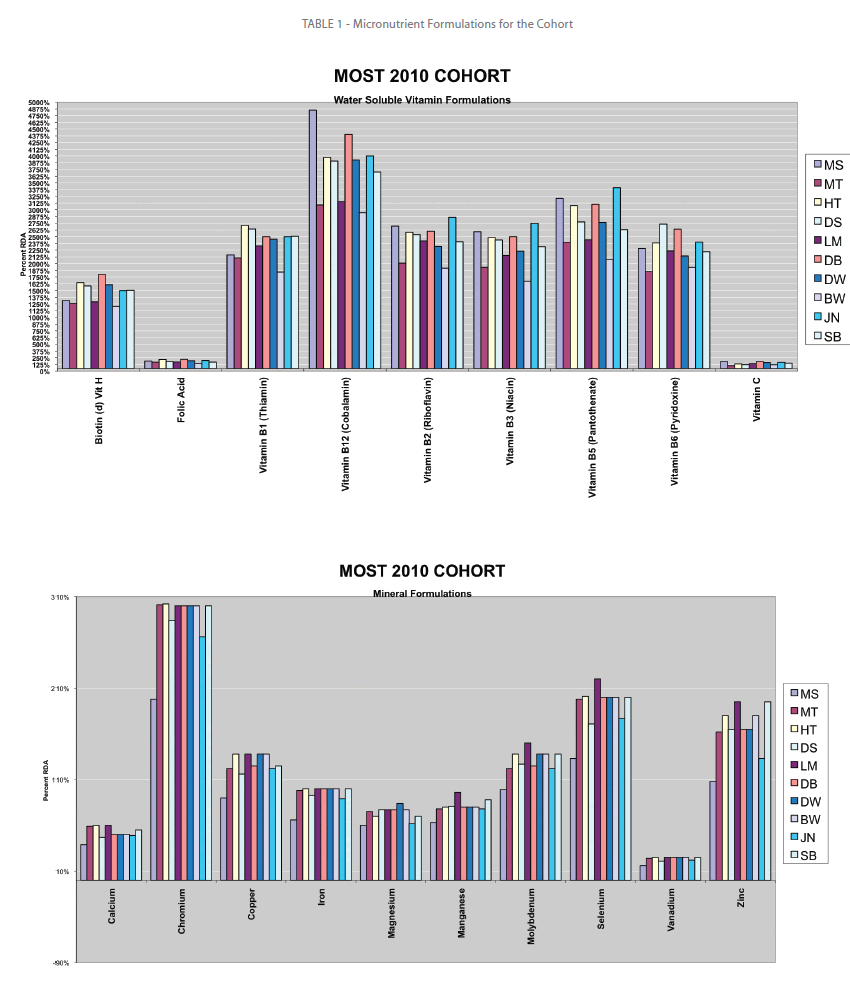
We examined prospectively a cohort of active adults aged 34 to 73 years (median 53.5) who were seen at a preventive medicine center late 2009 through early 2010. This pilot study group was selected merely as the first group of ten available for analysis. The group of adults, 6 men and 4 women were given a proprietary IVitaminScience (IVS) comprehensive health history questionnaire and then had their initial phlebotomy. Once their cellular laboratory results were completed, the data was entered, along with the nutrient history findings into the IVS’s proprietary algorithm that created individual, custom, therapeutic formulas for each participant. (See Table 1.)
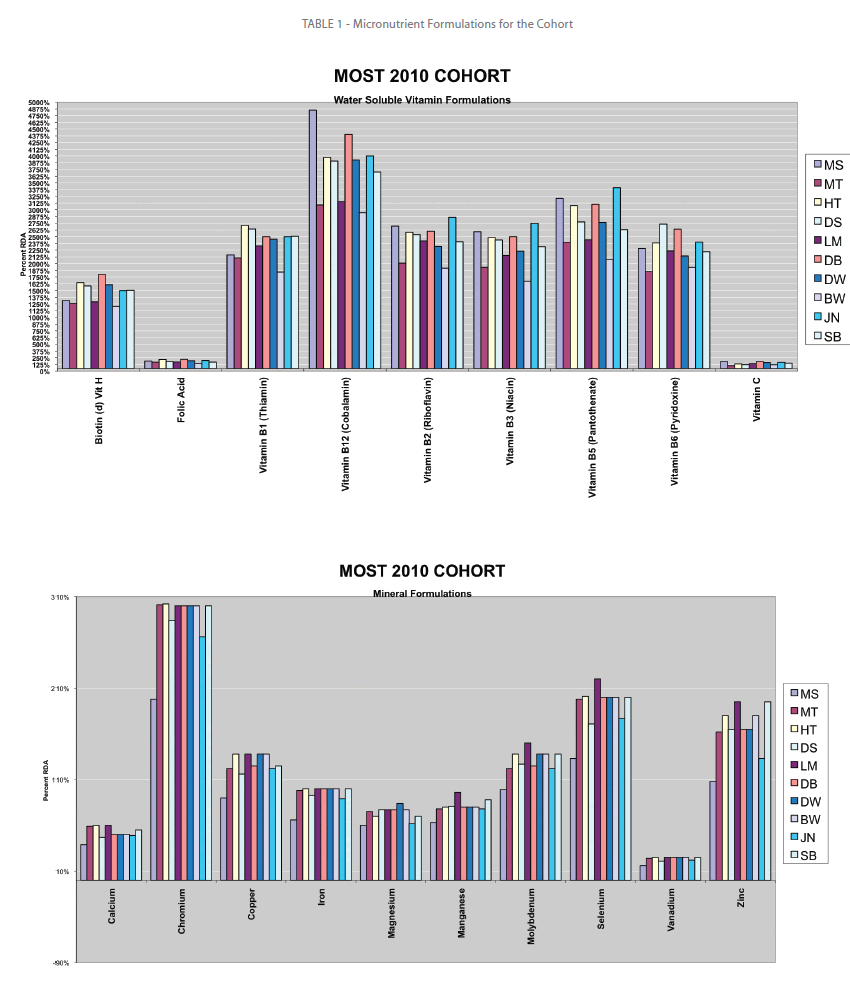
Table 1: Micronutrient Formulations for the Cohort
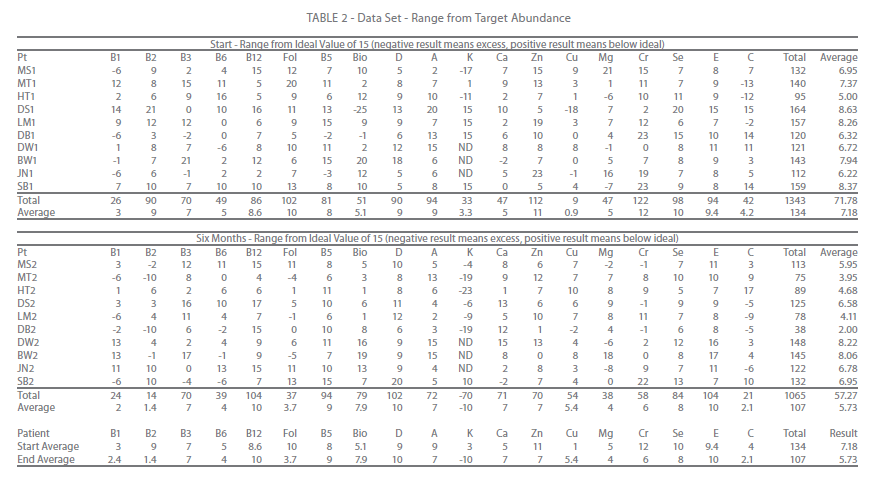
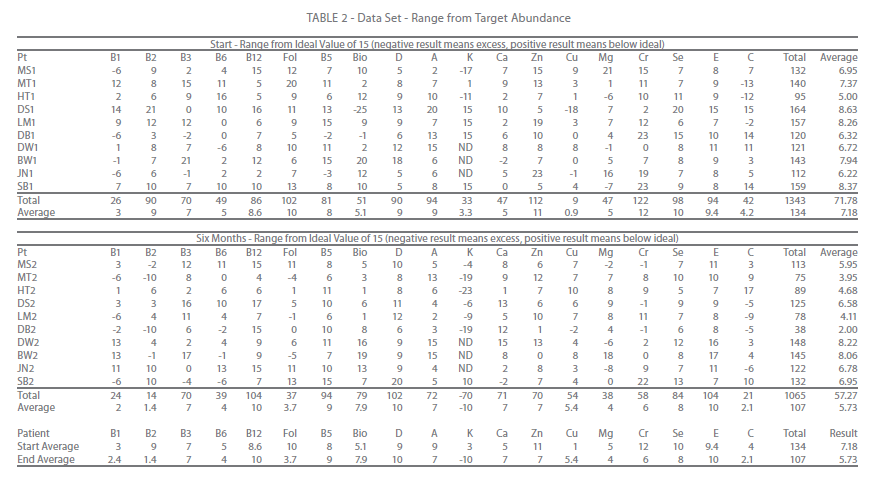
Table 2: Data Set - Range from Target Abundance
Thirteen individual vitamin and ten mineral components that were supplemented, each patient had at least 4 capsules per day of micronutrients and were asked to take their vitamins in the AM and their minerals in the PM. Each patient was also asked to refrain from any other micronutrient supplement for the duration of the study. At the end of 6 months, a second phlebotomy was performed and the results were compared against their baseline.
Blood samples were collected in two 10 ml heparinized tubes and shipped overnight to the testing facility. Upon receipt, peripheral blood mononuclear cells (over 90% lymphocytes) were isolated by Ficoll density gradient centrifugation and washed to remove platelets. Lymphocytes (150,000 cells/ml) were added to wells of microtiter plates with a series of over 60 different modifications of CFBI 1000 proprietary media, stimulated to grow by addition of phytohemagglutinin (PHA), and incubated for four days. Tritiated thymidine was then added, and incubation continued for another day. Cells were then harvested to retain DNA on filters, and a direct-read beta counter counted radioactivity. Results were expressed as a percentage of control (optimal) growth.[9]
Results
This trial was not only a supplemental challenge study, but also an efficiency study. The goals of the program were to replace all nutrients to a reasonable abundance, without creating large excesses. Target abundance was determined to a cellular numerical value of 15 when compared against the arithmetic difference from control to observed values, while deficiencies were defined as levels below 7. (See Table 1)
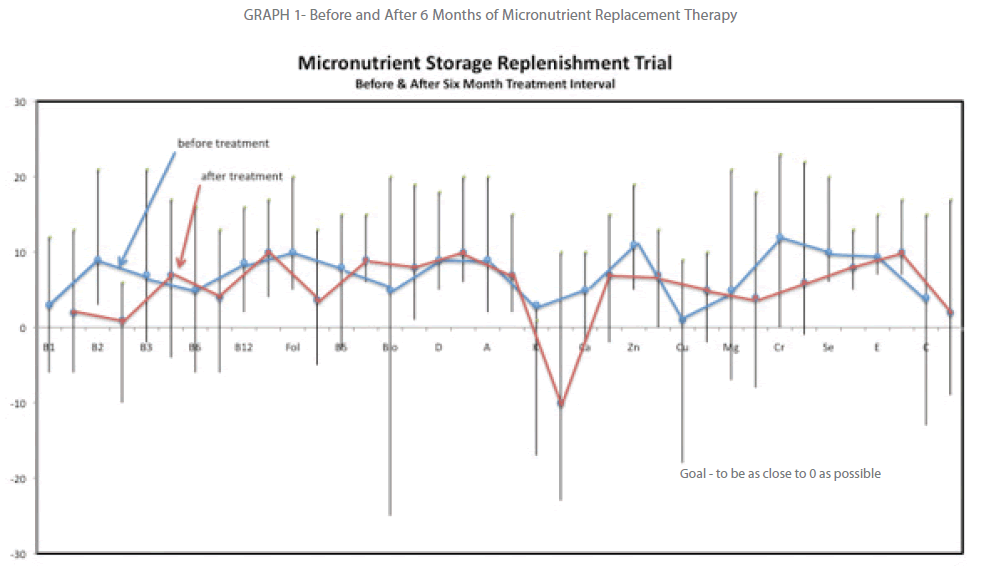
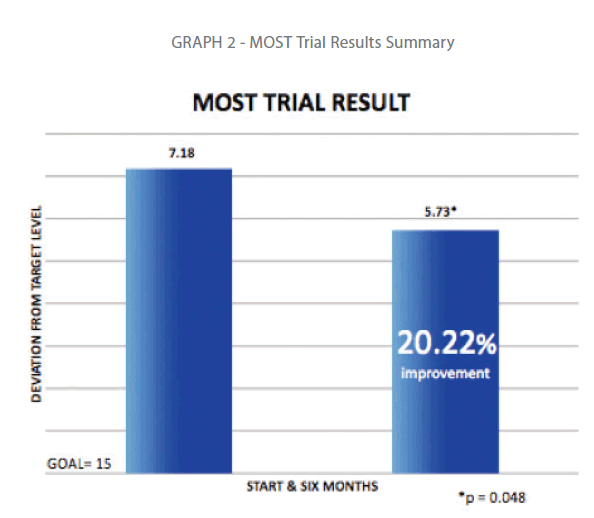
Ten vitamin and thirteen minerals were studied in this trial over the six months. Since lymphocytes tend to live anywhere from 3 months to 9 months, clinical experience suggests a biannual testing cycle that was followed. The individual nutrient levels were subtracted from the mean the ranges were summed and averaged. The ranges were thus compared against baseline. Over the time interval the average range from goal went from 7.18 to 5.73, which was a 20.22% improvement. (See Graph 2.) Paired T-test showed the small study reached statistical significance with a P value of 0.48. (See Appendix 1)
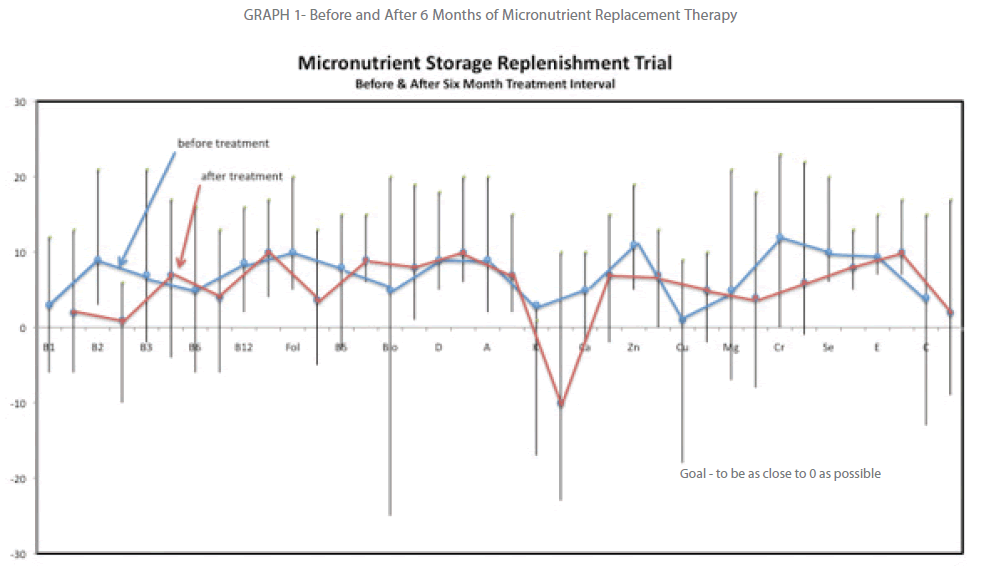
Graph 1: Before and After 6 Months of Micronutrient Replacement Therapy.
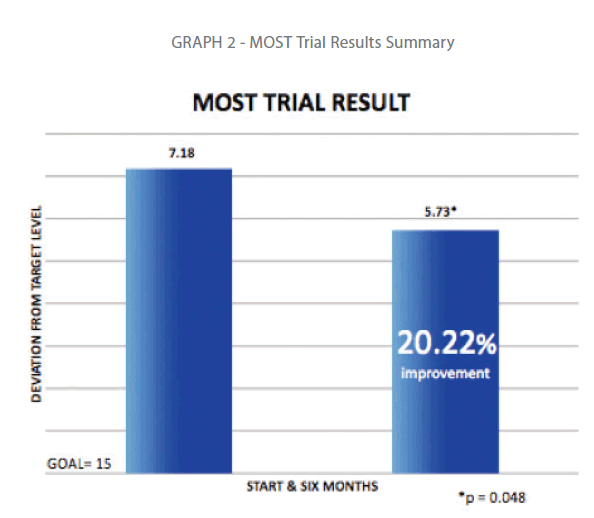
Graph 2: MOST Trial Results Summary
Discussion
The seductiveness of the possibility of personalized prevention and cures for disease has engulfed almost everyone; subsequently tremendous resources have been pushed towards nutrient and genomic research. This tidal wave of interest in vitamins and minerals has been bolstered by patient demands for a reverting back to a more time honored, personal approach to healthcare needs. Patients, providers, and policy makers rely on published data to shape lives, treat diseases, and legislate. The Recommended Dietary Allowances (RDAs), first published by the U.S. National Academy of Sciences in 1941 and revised every few years until 1989 when the Dietary Reference Intake (DRI) values superseded them, has been a time honored, highly respected tool.[10] The RDA provides the backbone and core of most supplements, and support preventive medicine and public health professionals in their duties. Unfortunately, these well-respected values are based on faulty methodology, and numbers are skewed, biased, and irreversibly flawed. They grossly underestimate the need for aggressive supplementation and have had significantly delayed progress in fighting preventive disease battles.
Scientists must avoid at least three major potential flaws in micronutrient experimental designs while attempting to determine the amount of micronutrients required by the body. If a study does not meet these standards, results should be dismissed as invalid. The MOST trial is the first, and only study that meets and exceeds this imperative threshold.
The first compulsory is to acknowledge the absoluteness of individuality. No two individuals share precise phenotypical expression despite their commonalities in genotype. Despite much research, genetic susceptibility to complex diseases such as heart disease, cancer and obesity has proved difficult to identify, with many poorly reproducible results. Except in a small percentage of cases, genes are poor predictors of future health.[11] Since classical nutrition research essentially treats everyone as genetically identical, their estimations, and conclusions lack objectivity. What is really difficult for most public health specialists to acknowledge is the fact that population research and metaanalysis studies, by designation, always fails the first imperative of respecting the unique requirements of individuals. When scientists attempt to measure the effect of a consistent dose of nutrient on disease mitigation, meta-analysis should and often does result in a null effect - a type II error. Moreover, any conclusions on RDA, DRI, or maximal tolerated dose (MTD) must therefore have to be challenged.
The second compulsory issue is that micronutrient testing has to be accurate - not only to dictate therapy, but also measure results. The peripheral blood lymphocyte is an ideal system for metabolic studies because it is easily obtained, is a primary resting cell that can be activated to proliferate, and presumably reflects both the genetic makeup and biochemical environmental history of the individual at the time the cells were formed.[12] Any study not using functional cellular testing is not using the gold standard, and places their results and recommendations in peril. There are a myriad of absurd tests being utilized by some researchers, such as urine, saliva, skin reflectivity, and hair sampling, and these studies should be summarily dismissed. Blood serum testing is still regarded highly by most physicians and scientists but serum does not provide accurate estimation of cellular status, and therapeutic suggestions and measure based on them simply extends the fiction. Serum testing only measures from 24 to 48 hours of nutrient intake, and results do not correlate well with cellular storage findings. While Genomicists are now able to peer into the nucleus of cells and read genetic coding, they only are able to predict where potential nutritional problems might occur. At this point genomics is an expensive and fancy term for educated guessing when it comes to nutrient needs, and provides nothing to gauge replacement therapies.
The third compulsory issue, for those who have advanced past the first two rather obvious challenges, is to treat indicated deficiencies therapeutically. Few have the experience and ability to provide custom, multi-component, therapeutic dosing of pharmaceutical grade, prescriptive multivitamins and minerals. Those who base therapy using dietary suggestion or multipliers of RDA underwhelm the body and provide little chance of significant improvement. This is why we have such conflicting data in regards to the value and impact vitamins and minerals have on disease mitigation.
The roles of the vitamins and minerals are diverse, with many of these nutrients doing double and triple duty. Some act like hormones, others are a part of enzymes, most are vital compounds that control metabolic reactions in the body. While many still feel that micronutrient supplementation is unnecessary, ineffective, wasteful, or even harmful - we only have our flawed studies to blame for their ignorance. Nutrient reference values have significant public health and policy implications.[13] Given the importance of defining reliable nutrient reference values, there is a need for an explicit, objective, and transparent process to set these values. We should utilize the MOST methodology to update the RDA, DRI and MTD values based on individuality, accurate testing, and therapeutic treatment and tolerances.
Advances in research and discovery, illuminating our understanding of disease at the molecular level, have enabled a new individualized approach to health and the treatment of disease. A generation of medicine and technologies based on an individual’s specific genetic make up is now empowering scientists, health care providers, and patients to develop new strategies for maintaining health, managing illness, and fighting disease. Micronutrient researchers must respect the greater effect of nurture over nature, and not rely on predictive medicine over objective medicine. Once we can accurately determine nutrient resources required to fend off environmental challenges, then, and only then will we be equipped to incorporate the power of genomics into future formulations.
2571
References
- “Nutritional Status and Health” SpectraCell Jan 2009 https://www.spectracell.com.
- “RDA’s vs. Optimal Nutrition” https://www.mreassociates.org June 2002
- Wellness International Network “Personal Vitamin Analysis” https://web.winltd.com/Article.aspx?PageURL=/Pages/English/ healthnews/spectracell. 1999
- Fairfield KM, Fletcher RH. Vitamins for chronic disease prevention in adults: scientific review. JAMA 2002; 287:3116-3126.
- Ames, B. N., “The metabolic tune-up: metabolic harmony and disease prevention,” J Nutr, vol. 133, no. 5 Suppl 1, pp. 1544S-1548S, May 2003.
- Ames, B. N., “Delaying the mitochondrial decay of aging-a metabolic tune-up,” Alzheimer Dis.Assoc.Disord., vol. 17 Suppl 2 pp. S54-S57, Apr. 2003.
- Houston, M. C. “The role of cellular micronutrient analysis, nutraceuticals, vitamins, antioxidants and minerals in the prevention and treatment of hypertension and cardiovascular disease” Ther Adv Cardiovasc Dis June 2010 vol. 4 no. 3 165-183
- Bucci L.R. “A functional analytical technique for monitoring nutrient status and repletion” Am Clin Lab. 1993 Jun;12(6):8, 10.
- Penland, J. “RDA and DRI, Not Just Acronyms” Grand Forks Human Research Service Oct 2006.
- Holtzman, N.A, Marteau, T. M (2000), Will Genetics Revolutionize Medicine? New England Journal of Medicine, 343,141-144.
- Pinkerton, S. W. et all. “ Development of a Chemically Defined Serum and Protein Free Medium for Growth of Human Peripheral Lymphocytes.” Proc Natl Acad Sci USA 1986 Jan;83(1):9-13.
- Russell Robert, MD et al. “Issues and Challenges in Conducting Systematic Reviews to Support Development of Nutrient Reference Values: Workshop Summary” Nutrition Research Series March 2009 Vol. 2.