Letter - (2022) Volume 13, Issue 8
Migraine with aura, a significant and independent risk factor for ischemic stroke
Léhleng Agba1,2*,
Donissongui Soro1,
Awissoba Awidina-Ama1,
Hugo Yaïche1 and
Olivier Heinzlef1
1Department of Neurology, Centre Hospitalier Intercommunal de Poissy/Saint-Germain-En-Laye, Poissy, France
2Department of Neurology, CHU-Kara, Université de Kara, Kara, Togo
*Correspondence:
Léhleng Agba, Department of Neurology, CHU-Kara, Université de Kara, Kara,
Togo,
Email:
Received: 11-Aug-2022, Manuscript No. ipjnn-22-12977;
Editor assigned: 12-Aug-2022, Pre QC No. P-12977;
Reviewed: 18-Aug-2022, QC No. Q-12977;
Revised: 24-Aug-2022, Manuscript No. R-12977;
Published:
31-Aug-2022
Abstract
Migraine is the most common type of headache in young adults
mainly in women. It has been reported by some observational
studies as an independent risk factor for ischemic stroke. We report
the case of a migrainous patient who presented an ischemic stroke
following a prolonged episode of visual aura. His only other risk
factor was smoking.
Keywords
Migraine; Visual aura; Migraine; Ischemic stroke
Introduction
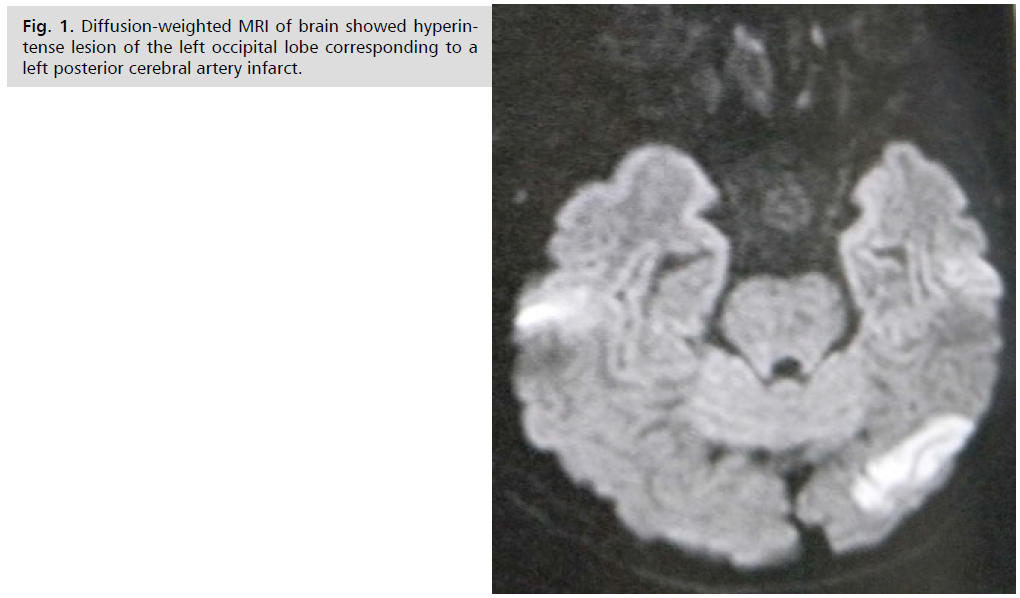
A 66-year-old right-handed man, a physician, presented at
the end of the day with a flickering scotoma of the right
eye, followed about ten minutes later by pulsating left
hemicranial headaches without nausea or vomiting. The
visual disturbances persisted until the next day. He therefore
performed on his own request, a brain magnetic resonance
imaging (MRI) which revealed an ischemic stroke in
the left posterior cerebral artery (Fig. 1). He arranges to
be hospitalized in the neurology ward. The patient had
been suffering from migraine with visual aura for over
15 years, treated with Aspegic 1g in case of crisis. He is
an active smoker with 10 pack-years. He denied another
cardiovascular risk factors. The patient had a BMI of 27
kg/m2, blood pressure of 128/80 mm Hg, pulse of 63/min,
and blood glucose of 0.94 g/L. Neurologically, he had good
consciousness and alertness, no motor or sensory deficits.
He had only a right homonymous hemianopsia. Laboratory
tests were normal. Echo-doppler of supra-aortic vessels and
the 48-hour ECG holter were all normal. The diagnosis of
migraine infarction was retained. He received Aspegic 160
mg/day, Amytryptiline 15 mg/day and Paracetamol 1 g/8h
in case of headache. He had a good outcome.
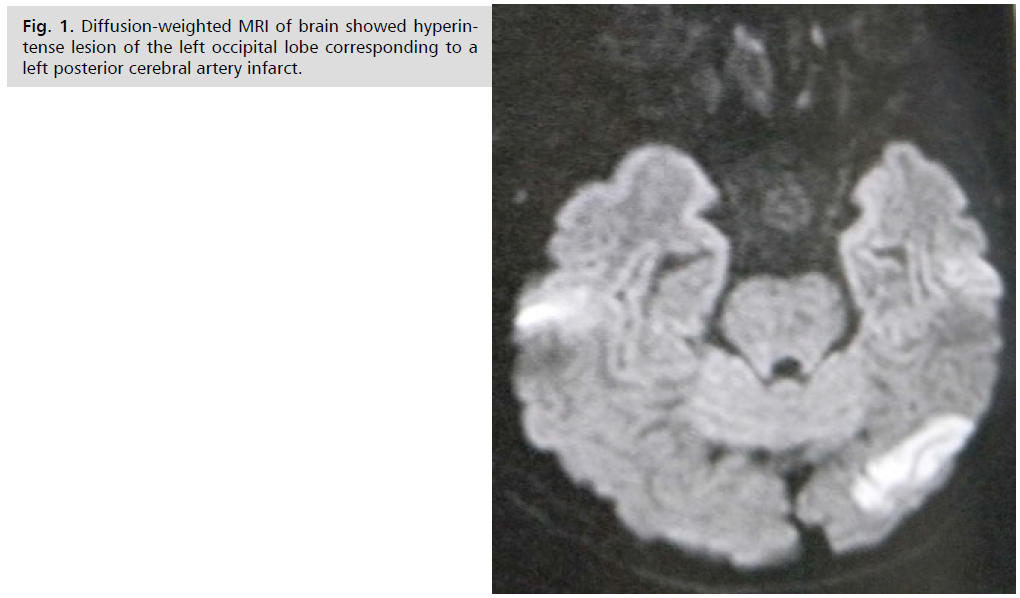
Fig 1:Diffusion-weighted MRI of brain showed hyperintense lesion of the left occipital lobe corresponding to a left posterior cerebral artery infarct.
Results and Discussion
Chronic, recurrent headaches, particularly migraines,
have become one of the leading causes of disabilities globally
[1]. Migraine is the most common type of headache in
young adults, with an estimated prevalence of 4% before
puberty and as high as 25% in women by their mid to
late 30s [2]. Some observational studies have shown an
increase in the risk of stroke among people with a history of
migraine, but others have failed to find this association [2].
Ischemic stroke in a migraine sufferer may be
categorised as cerebral infarction of other cause coexisting
with migraine, cerebral infarction of other cause presenting
with symptoms resembling migraine with aura (MA) or
cerebral infarction occurring during the course of a typical
migraine with aura attack. Only the last fulfils criteria
for migrainous infarction. Migrainous infarction mostly
occurs in the posterior circulation and in younger women
[3]. In 2004, Etminan et al. performed a systematic review
and meta-analysis of observational studies from 14 studies,
including 11 case-control studies and 3 cohorts, looking
for the risk of ischaemic stroke in people with migraine.
This study suggested that the risk of stroke is increased
in people with migraine and was consistent in people
who had MA (RR 2.27) and migraine without aura (RR
1.83), as well as in those taking oral contraceptives (RR 8.72) [2]. Among the subtypes of auras, the visual aura is
that which has been most reported by studies as associated
with ischemic stroke. Indeed, the survey “Ischemic
stroke subtypes and migraine with visual aura in the
Atherosclerosis Risk in Communities (ARIC) study” also
made the high link between MA and high risk of ischemic
stroke [4]. The exact mechanisms for migraine-induced
stroke have been hypothesized equally heavily. One possible
mechanism is progressive hypoperfusion and reduction
in cerebral blood flow that occurs during migraine. The
mechanism by which this hypoperfusion occurs is called
“spreading depression” which is a marked reduction in
potential generating activity within neuronal membranes in the gray matter that advances across the cortex at a rate
similar to the one seen with the progression of symptoms in
migraines. Another possible mechanism of cerebrovascular
hypoperfusion is vasospasm. Several case reports have
established this link [1]. The association between migraines
and strokes is further supported by increased concentration
and activation of several intravascular procoagulant factors
in migraineurs. It seems that migraine with visual aura
may promote vasospasm, activate platelet aggregation,
and increased concentration of procoagulant factors [4].
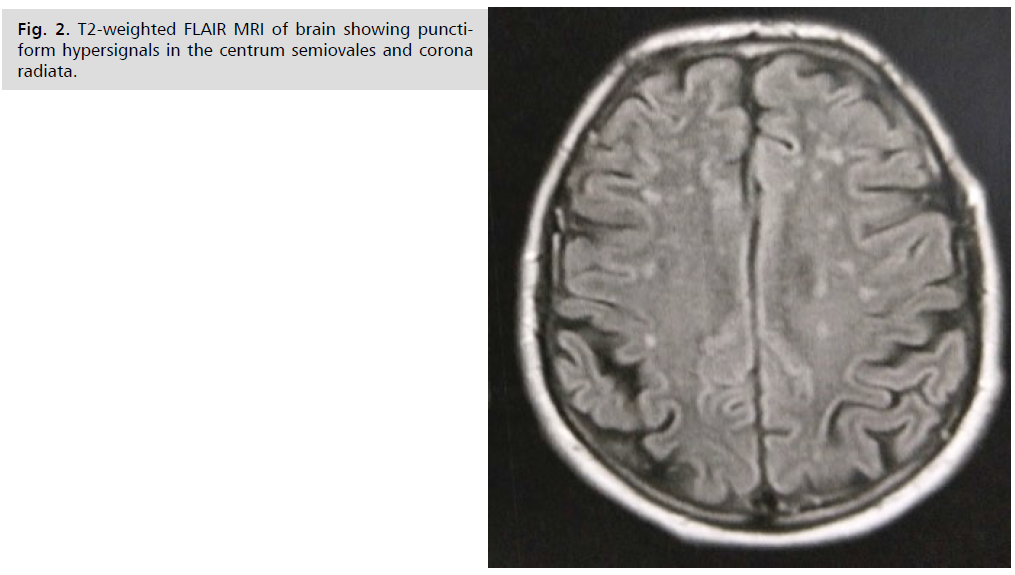
White matter lesions are a common finding in patients
with migraines. These lesions are visible as hyperintense
lesions on T2-weighted and fluid-attenuated inversion recovery images (Fig. 2). Some authors suggest that white
matter abnormalities are due to ischaemic insults [3].
Smoking is another risk factor that increases the likelihood
of migraineurs experiencing strokes at some point in their
life, particularly in the elderly. The prevalence of smoking
is 33% higher in migraineurs, with a positive relationship
between migraine attacks and the number of cigarettes
smoked [5]. Although currently there is no recommended
guideline for primary prevention of ischaemic stroke in
migraineurs, if clinically indicated, it would be appropriate
to select medications that reduce both migraine attacks
and vascular risks in migraineurs. Antihypertensive agents
including beta blockers, angiotensin II receptor blockers
and ACE inhibitors have shown a better effect than placebo
in reducing frequency, severity and disability of migraine.
Statin and statin with vitamin D have been reported to be
efficacious for migraine prophylaxis in case reports [3].
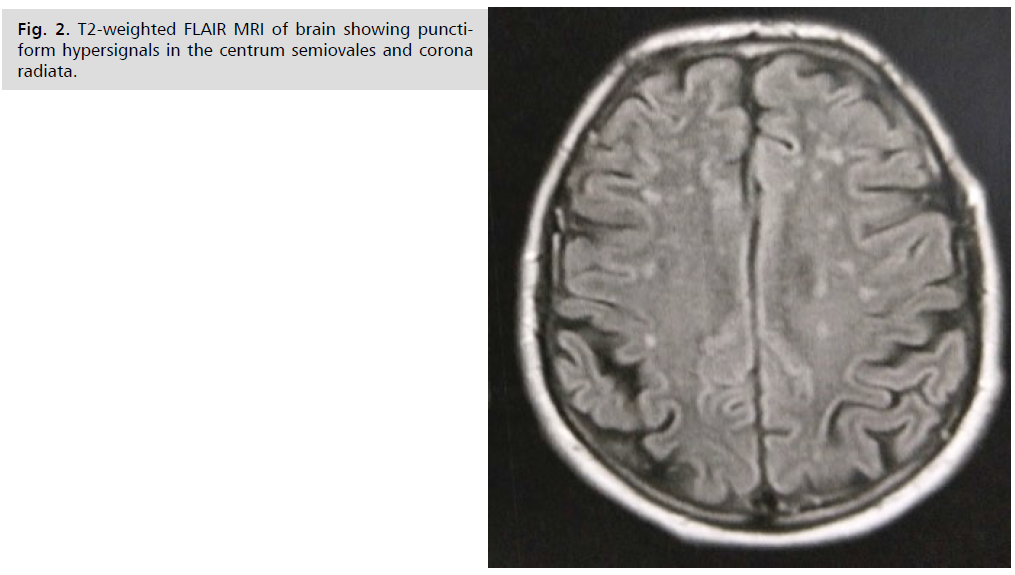
Fig 2:T2-weighted FLAIR MRI of brain showing punctiform hypersignals in the centrum semiovales and corona radiata.
Conclusion
Based on previous observational studies, it is clear that
migraine, especially migraine with aura, is an independent
risk factor for cardiovascular disease, including ischemic
stroke. Focal neurological signs associated with migraine
episodes, regardless of type, require brain imaging to avoid
complications that can be treated early and effectively.
Acknowledgement
We do not receive any fund for this work. Patient
consent has been received as well as approval from the
National Ethics Committee.
Conflict of Interest
The authors declare that there is no conflict of interest.
REFERENCES
- Hassan M, Belavadi R, Gudigopuram SVR, et al. Migraine and stroke: In search of shared pathways, mechanisms, and risk factors. Cureus. 2021;13(12):e20202.
Google Scholar, Crossref, Indexed at
- Etminan M, Takkouche B, Isorna FC, et al. Risk of ischaemic stroke in people with migraine: systematic review and meta-analysis of observational studies. BMJ. 2005; 330(7482):63.
Google Scholar, Crossref, Indexed at
- Zhang Y, Parikh A, Qian S. Stroke and vascular. Stroke Vasc Neurol. 2017;2(3):160-167.
Crossref, Indexed at
- Androulakis XM, Kodumuri N, Giamberardino LD, et al. Ischemic stroke subtypes and migraine with visual aura in the ARIC study. Neurology. 2016;87(24):2527-2532.
Google Scholar, Crossref, Indexed at
- López-Mesonero L, Márquez S, Parra P, et al. Smoking as a precipitating factor for migraine: a survey in medical students. J Headache Pain. 2009;10(2):101-103.
Google Scholar, Crossref, Indexed at