Keywords
Osteoporosis; Vitamin D; Osteomalacia; Calcium
Introduction
Bone
Bone is very important tissue, which formed commonly from collagen, which is a protein that responsible for softness of framework, and calcium phosphate, a mineral that responsible for strength and hardens of framework (Figure 1) [1].

Figure 1: Structure of bone
This interaction between protein and minerals donate the bone both flexible and strong. Main concentration of calcium present in bones and teeth.
During lifetime, old bone is removed and new bone is formed. Rate of bone formation is faster than the rates of bone remove during childhood. So, bones become more large, heavy, and dense. In women, rate of bone removed increase after post menopause. Bones need calcium and phosphorus to remain healthy and strong, but the body also needs vitamin D to be able to absorb these two minerals. Without this necessary vitamin, bones can become soft and flexible. The most common bone illnesses between populations are osteoporosis and osteomalacia. Osteoporosis is more well-known than osteomalacia [2].
Osteoporosis
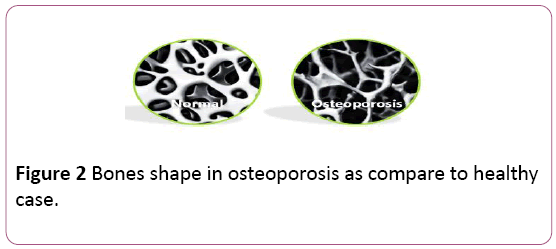
Definition of osteoporosis: Osteoporosis is a bone disease which characterized by low bone mass as result of body loses too much bone and makes too little bone. This leads to increased bone fragility so increased susceptibility to fracture, especially in the hip, spine, wrist and shoulder. Osteoporosis means “porous bone.” Healthy bone looks like a honeycomb. Once osteoporosis happens, the holes and spaces in the honeycomb are much larger than in healthy bone. Though bones in osteoporosis have lost density, weaken and are more expected to break (Figure 2) [3].
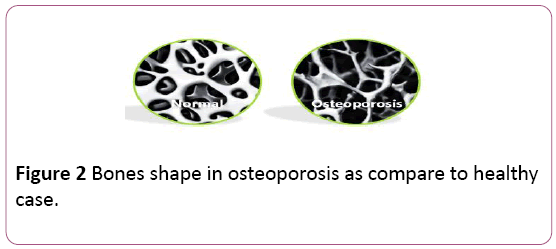
Figure 2: Bones shape in osteoporosis as compare to healthy case.
Epidemiology of osteoporosis: Osteoporosis is more common than heart attack, stroke and breast cancer combined as shown in Figure 3.

Figure 3: Incidence of common diseases.
200 million people have suffered from osteoporosis. Osteoporosis rate increases according to age. Also, osteoporosis depends on gender; it is more common in women than men at least one in three women and one in five men will suffer from osteoporosis. White and Asian people are at greater risk to osteoporosis as compared to African [4].
Sign and symptoms of osteoporosis: Osteoporosis is often recognized as “the silent thief” for the reason that bone loss happens without symptoms. Osteoporosis can be present without any symptoms until bone breaks. The symptom associated with osteoporotic fractures usually is pain; the position of the pain depends on the location of the fracture [5].
Causes of osteoporosis: Bones are in a constant state of regeneration where new bone is made, and old bone is broken down. During childhood, body makes new bone faster than it breaks down old bone, so bone mass increases. In old people, bone mass is lost faster than it's formed. The chief cause of osteoporosis is a deficiency of certain hormones, as androgen in men and estrogen in women. Menopause is a foremost factor that cause lower estrogen levels and increase women’s risk for osteoporosis. Risk factors for osteoporosis include genetics trouble, absence of exercise, deficiency of calcium and vitamin D, malabsorption, high-dose oral corticosteroids, low body mass, smoking, alcohol intake, rheumatoid arthritis, and family history of osteoporosis [6].
Diagnosis of osteoporosis: Diagnosis of osteoporosis can be suggested by X-rays and confirmed by tests to measure bone density. Detection of calcium and vitamin D levels, also help in early diagnosis of osteoporosis [7].
Pathogenesis of osteoporosis: Osteoporosis result due to imbalance between bone resorption and bone formation. This process takes place in bone multicellular units. Osteoclasts are aided by transcription factor PU.1 to destroy the bone matrix, while osteoblasts reconstruct the bone matrix. Low bone mass density occurs if osteoclasts are degrading the bone matrix faster than the osteoblasts are rebuilding the bone. There are three main mechanisms by which osteoporosis develops; an insufficient peak bone mass, excessive bone resorption, and insufficient formation of new bone. Hormonal factors strongly control on the rate of bone resorption; lack of estrogen increases bone resorption, also decreasing the deposition of new bone [8]. In addition to calcium metabolism plays a significant role in bone turnover, and deficiency of calcium and vitamin D leads to diminished bone deposition; moreover, the parathyroid glands react to low calcium levels by secreting parathyroid hormone, which increases bone resorption to safeguard enough calcium in the blood. Calcitonin, a hormone produced by the thyroid that increases bone deposition, is less effective as compared to PTH [9].
Treatment of osteoporosis: The aim of treatment of osteoporosis is the avoidance of bone fractures by overcoming bone loss or by increasing bone density. Drugs which are used in treatment of osteoporosis include:
• Bisphosphonates drugs which responsible for decrease bone loss hence reduce risk of fracture.
• Estrogen antagonists which act as inhibitor for spine fractures.
• Calcitonin which responsible for prevention spinal fracture in postmenopausal women.
• Parathyroid hormone which stimulates formation of bones.
• Calcium supplements.
• Vitamin D supplements [10].
As well as, prevention of osteoporosis is most important than treatment. Osteoporosis can be prevented by:
Lifestyle changes, including take off smoking, excessive alcohol intake, take sufficient calcium and vitamin D.
• Take drugs that stop bone loss and increase bone strength, alendronate, risedronate, calcitonin.
• Take medications which increase bone formation such as teriparatide [11].
Osteomalacia
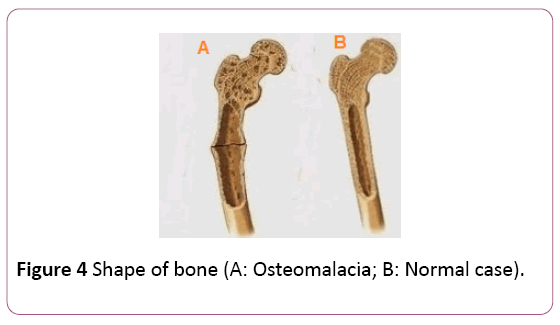
Definition of osteomalacia: It is the softening of the bones due to impaired bone metabolism as result of insufficient levels of phosphate, calcium, and vitamin D, or because of resorption of calcium. All of this leads to inadequate bone mineralization. Osteomalacia in children is known as rickets (Figure 4) [12].
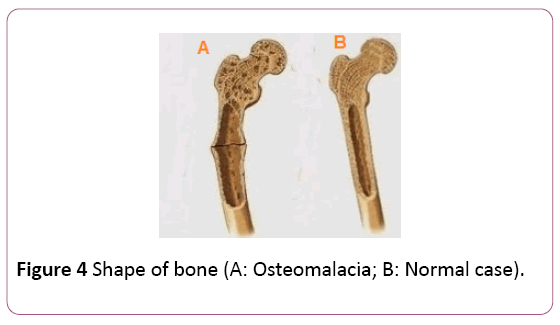
Figure 4: Shape of bone (A: Osteomalacia; B: Normal case).
Epidemiology of osteomalacia: Osteomalacia is rare in the United States and Western Europe. In attendance is a developing in occurrence of vitamin D deficiency in various countries, which responsible for suffer from hypocalcaemia, secondary hyperparathyroidism, secondary hypophosphatemia, and osteomalacia. People at risk include:
• The people who have slight exposure to the sun and take inadequate amount from dietary calcium and vitamin D.
• Patients with malabsorption as in gastrointestinal bypass surgery, or celiac disease.
• Vegetarian diets without vitamin D supplementation.
• Take anticonvulsant therapy include phenytoin and phenobarbital for long time [13].
Sign and symptoms of osteomalacia: Osteomalacia might not have any symptoms in early stage, even though signs of osteomalacia may be apparent on an X-ray or additional diagnostic tests. For instance osteomalacia progresses, development of bone pain and muscle weakness occur [14].
The foremost symptom of osteomalacia is pain in bones, especially in lower back, hips, and legs at night. Muscle cramps, numbness and tingling in legs may be occurring in osteomalacia due to deficiency of vitamin D and calcium. Waddling of gait due to weakness in the legs and lack of proper muscle tone is addition to frequency of fracture [15].
Causes of osteomalacia: Osteomalacia happens from a defect in bone modulation process. In metabolic process the body required some minerals as calcium and phosphate in synthesis process of bones. So develop osteomalacia occur as result of deficiency of these minerals. These problems may be caused by as follows [16]:
• Vitamin D Deficiency: Vitamin D deficiency is the furthermost common cause of osteomalacia. People who live far from exposure to sunlight or take inadequate amount of vitamin D can develop osteomalacia [13].
• Certain surgeries: Surgery bypass your small intestine can lead to vitamin D and calcium deficiency.
• Celiac disease. It is autoimmune disease which responsible for malabsorption of calcium and vitamin D [17].
• Kidney or liver disorders: Any problems kidneys or liver can inhibit the ability of body to synthesis active vitamin D.
• Drugs: Some drugs as phenobarbital can cause severe vitamin D deficiency.
Diagnosis of osteomalacia: Biochemical feature of osteomalacia is similar to rickets. Biochemical findings in osteomalacia included as follows [18]:
• Low serum and urinary calcium.
• Low serum phosphate.
• Elevated serum alkaline phosphatase.
• Elevated parathyroid hormone.
• Bone X-rays and a bone density test can help detect bone softening so, help in diagnosis of osteomalacia.
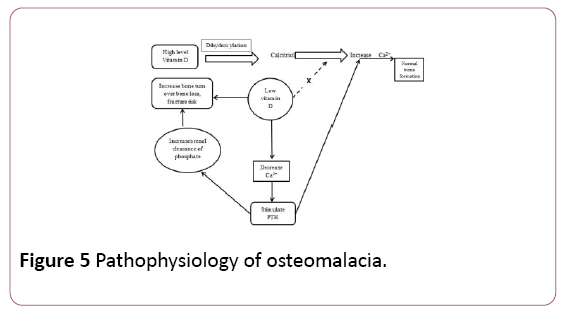
Pathogenesis of osteomalacia: Bone synthesis is required sufficient amount from ionized calcium and phosphate. Calcium concentration influence by Vitamin D after its dihydroxylation into calcitriol. When level of vitamin D decrease impaired in metabolic process occurs as result of drop in concentration of calcium [19]. Low calcium levels stimulate secretion of parathyroid hormone (PTH) from parathyroid gland. PTH raises calcium concentration but also increases renal clearance of phosphate. Once phosphate decreases lower than a critical level, mineralization cannot proceed normally as in Figure 5 [20].
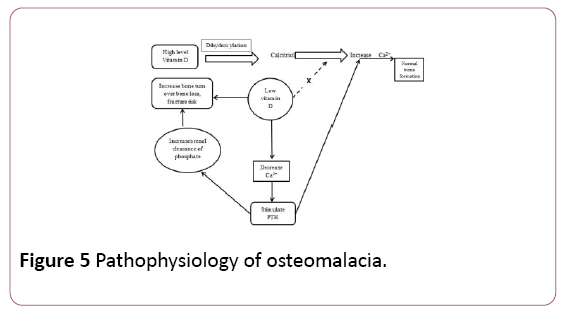
Figure 5: Pathophysiology of osteomalacia.
Treatment of osteomalacia: Treatment of osteomalacia can be occur by administration of 10,000 IU weekly of vitamin D for four to six weeks. While Osteomalacia due to malabsorption require treatment daily by injection or oral significant amounts of vitamin D. Treatment may include vitamin D, calcium, and phosphorus supplements [21].
Differentiation between osteoporosis and osteomalacia
Although both osteoporosis and osteomalacia are bone diseases, there are various differences between them. The differences between osteoporosis and osteomalacia are summarized in Table 1.
| Osteomalacia |
Osteoporosis |
Differences |
| Demineralization of the bones |
Reduction of the bone mineral density |
Definition |
| Adults |
≥ 65 years women |
Presence |
| Weakness of the muscles and fragile bones |
Curving of the back and risk for fractures |
signs and symptoms |
| Deficiency in Vitamin D |
Deficiency in calcium and phosphorous, drugs, inherited, endocrine disorders, alcohol drinking. |
Causes |
| Injections of Vitamin D |
Healthy lifestyle, calcium supplements and naturally calcium-diet |
Treatment |
Table 1: Differences between osteoporosis and osteomalacia.
Discussion
Future trends
Although calcium and vitamin D play important role in bone synthesis, although Mg has important bio vital effect on maintaining skeletal health. Alternative warm area of research relates to the use of mesenchymal stem cells (MSC) for regenerative medicine in treatment of bone diseases including osteoporosis, and osteomalacia [22].
Conclusion
Osteoporosis is reduction of mass of the bones. On the other hand osteomalacia is the softening of the bones. Osteoporosis can be cause due to deficiency of vitamin D, while osteomalacia is caused by a deficiency in calcium and phosphorus. Treatment of these diseases can be significant by using calcium, vitamin D with high does naturally or in the form of supplements.
Conflict of Interest
The authors declare that they have no conflict of interest.
21384
References
- Rinaldo F, Gisela R, Estela S, Manuel J (2015) Biology of bone tissue: Structure, function, and factors that influence bone cells. Biomed Res Int 1: 17.
- Golob A, Laya M (2015) Osteoporosis: Screening, prevention, and management. Med Clin North Am 99: 587-606.
- Svedbom A, Hernlund E, Ivergård M (2013) Osteoporosis in the European Union: A compendium of country-specific reports. Arch Osteoporos8: 137.
- Wade S, Strader C, Fitzpatrick L (2014) Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Osteoporos 9: 182.
- Kim D, Vaccaro A (2006) Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J 6: 479-487.
- Malay S, Rajeev B, Irappa M (2015) Osteoporosis in chronic obstructive pulmonary disease. Clin Med Insights Circ Respir Pulm Med9: 5-21.
- Guglielmi G, Scalzo G (2010) Imaging tools transform diagnosis of osteoporosis. Diagnos Imag Eur 26: 7-11.
- Maria H, Pedro G (2016) Bone cells dynamics during peri-implantitis: Atheoretical analysis. J Oral Maxillofac Res7: e6.
- Jacqueline G (2015) Parathyroid hormone, calcitonin and vitamin D testing in calcium and bone metabolic disorders. Medlab Magazine 26:28.
- Moyer V (2013) Vitamin D and calcium supplementation to prevent fractures in adults: U.S. preventive services task force recommendation statement. Ann Intern Med 158: 691-696.
- Adler A, El-Hajj F, Ghada B (2016) Managing osteoporosis in patients on long-term bisphosphonate treatment: Report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 31: 16-35.
- Salmon B, Bardet C, Coyac B (2016) Abnormal osteopontin and matrix extracellular phosphoglycoprotein localization, and odontoblast differentiation, in X-linked hypophosphatemic teeth. Connect Tissue Res 55: 79-82.
- Cesur Y, Yuca SA, Kaya A (2013) Vitamin D deficiency rickets in infants presenting with hypocalcaemic convulsions. West Indian Med J62:201-204.
- Anish A, Rohit R, Joshua K (2015) Imaging findings and evaluation of metabolic bone disease. Adv Radiol2015:1-21.
- Ritu G, Ajay G (2014) Vitamin D deficiency in india: prevalence, causalities and interventions. Nutrients 6: 729-775.
- Holick, Michael F (2007) Vitamin D deficiency. N Engl J Med 357: 266-281.
- Joao F, Larry A, Patricia A (2013) Calcitriol, calcidiol, parathyroid hormone, and fibroblast growth factor-23 interactions in chronic kidney disease. J Vet Emerg Crit Care 23:134-162.
- Blaine J, Chonchol M, Levi M (2015) Renal control of calcium, phosphate, and magnesium homeostasis. Clin J Am Soc Nephrol 10: 1257-1272.
- Fikry E (2017) Effect of coeliac disease on gastrointestinal tract and immunity. J Steroids Horm Sci 8:185
- Manisha S, Rakesh S (2012) Rickets-vitamin D deficiency and dependency. Indian J Endocrinol Metab 16: 164-176.
- Sara C, Alessandra C, Walter A (2013) Magnesium and osteoporosis: Current state of knowledge and future research directions. Nutrients 5: 3022-3033.