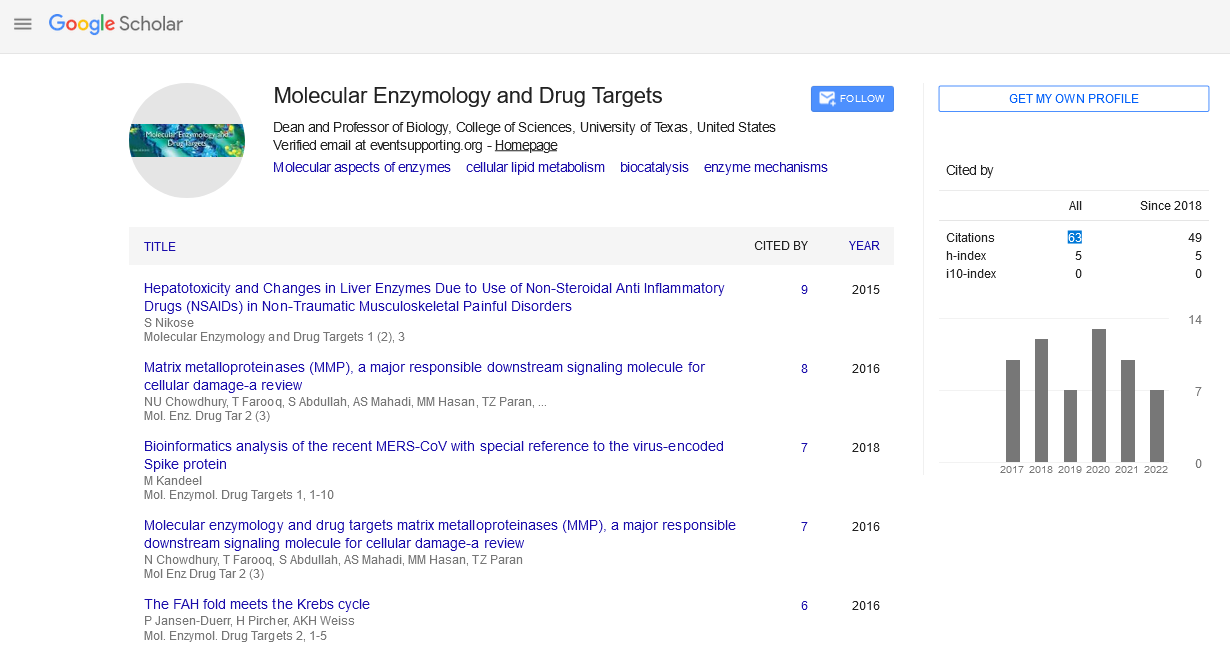
Perspective - (2022) Volume 8, Issue 3
Modulatinn intestinal uptake of Atenolol
1Department of Pharmaceutics, College of Pharmacy, King Saud University, P.O. Box 2457, Riyadh 1 1451, Kingdom of Saudi Arabia, Saudi Arabia
*Correspondence:
lbrahim A. lsarr, Department of Pharmaceutics, College of Pharmacy, King Saud University, P.O. Box 2457, Riyadh 1 1451, Kingdom of Saudi Arabia,
Saudi Arabia,
Tel: 641 10-2499,
Email:
Received: 02-May-2022, Manuscript No. Ipmedt-22-13013;
Editor assigned: 03-May-2022, Pre QC No. Ipmedt-22-13013 (PQ);
Reviewed: 16-May-2022, QC No. Ipmedt-22-13013;
Revised: 23-May-2022, Manuscript No. Ipmedt-22-13013 (R);
Published:
30-May-2022
Abstract
Drug permeation across membranes or targeting to specific tissues. Having a considerable ability to improve the permeability of drugs through lipoid membranes, niosomes have been utilized as carriers to enhance atenolol absorption from the gastrointestinal tract. Two methods have been adopted to prepare niosomes, the proniosome-derived method and the conventional film hydration method. The products from the two methods were compared in terms of their morphology, vesicle size, drug encapsulation efficiency, in vitro drug release and enhancement effect on drug permeation across the intestinal membrane using an averted sac technique. Proniosome-derived niosomes were smoother and exhibited a smaller (5 pm) vesicle size compared to those prepared by conventional methods (1 2 pm). High encapsulation efficiencies of 98.6% and 93.4% were achieved by methods A and B, respectively. In vitro drug release has been significantly retarded from both types of niosomes. Comparing to pure drug, which dissolved completely in 15 min, only 8.9% and 9.9% of the entrapped drug was released in the same time period. However, the difference between the two types of niosomes was not significant.
Keywords
Atenolol; Niosomes; Averted sac; Intestinal absorption; Permeation enhancer
INTRODUCTION
Pharmaceutical modification by inclusion complication has been extensively developed to improve drug absorption and bioavailability. Non-ionic surfactant vesicles known as niosomes are microscopic lamellar structures formed on admixture of a non-ionic surfactant, cholesterol and lecithin with subsequent hydration in aqueous media [1]. Niosomes are biodegradable, biocompatible, non-toxic and capable of encapsulating large quantities of material in relatively small volumes of vesicles. However, little research related to the effect of niosomes on drug permeation through the intestinal membrane could be identified, although promising results have been reported. Atenolol is a P-adrenergic receptor blocking agent used for treatment of hypertension, either alone or with other antihypertensive such as thiazide diuretics. It is reported that the bioavailability of 50 mg atenolol tablets is only about 63 % [2]. The aim of this present work was to investigate the suitability of liposomal preparation as a drug carrier for the antihypertensive drug, atenolol, which could be used as an aid to enhance the intestinal absorption of the drug using the averted sac technique.
Description
The open-end of the glass tube was covered with a lid and the tube was warmed in a water bath at 65 + 3 "C for 5 min [3]. Then 1.6 ml of phosphate buffer (pH 7.4) was added and the mixture was further warmed in the water bath for about 2 min so that a clear solution was obtained. The mixture was allowed to cool to room temperature until the dispersion was converted to proniosomal gel. The proniosomal gel was then hydrated with 10 ml phosphate buffer (pH 7.4), and the formed niosomes were separated by centrifugation at 25000 rpm at 20 "C for 30 min. The resulting niosomes were dried in an oven at 40 "C. The mixture was transferred to a 500 ml round bottom flask and attached to a rotary evaporator (Buchi Rotavapor RE 120). The organic solvents were removed under reduced pressure at 60 "C to form a thin dry film on the wall of the flask. The film was then hydrated with 20 ml of phosphate buffer (pH 7.4) at 60 "C at a rotation speed of 150 rpm for 1 hour. The dispersion was sonicated for 3 min. The dispersion of the formed niosomes was then centrifuged at 25000 rpm at 20 "C for 30 min, the supernatant decanted, and the separated niosomes were dried in an oven at 40 "C. Briefly, the mobile phase consisted of acetonitrilelmethanoIlO.01 M phosphate buffer with a pH adjusted to 6.0 with NaOH, containing 0.01% dodecyl sulphate sodium salt delivered at a flow rate of 1.2 mllmin at ambient temperature through a Lichrosorb analytical column, 250 x 4.6 mm ID, 10 pm RP18 (Merck), protected by a guard column (Security-guard; Phenomenex, CA, USA) [4]. To 500 pI of each sample, 100 p1 of metoprolol of 5 pg/ml in methanol water (1: 1) and 200 pl of NaOH (0.25 M) were added. The tubes were then centrifuged (14000 rpm at 25 "C for 10 minutes), the organic layer was discarded, and the aqueous phase was transferred to a clean tube to be evaporated to dryness at 40 "C, under a N2 stream. The residue was dissolved with 100 p1 of the mobile phase, transferred to the injection vials, and a 20 pl aliquot was injected into the chromatographic system. . The aqueous suspension was sonicated in a sonicator bath (Transonic T460/H, Elma, Germany) for 5 min. The atenolol-containing niosomes were separated from untrapped drug by centrifugation at 25000 rpm at 20 "C for 30 min [5]. The supernatant was recovered and assayed by HPLC method for atenolol content. A 0.2 g sample of dried niosomes prepared by method A or B was spread on a circular glass disk (5.04 cm2 diameter), then covered by cellophane dialyzing membrane (with molecular weight cut-off 8000, Spectrum Medical Inc., Los Angeles, USA) which was securely mounted on the disk by a rubber band. The disk was placed on the bottom of a glass tube fitting the disk diameter. Fifty ml of phosphate buffer (pH 7.4) was poured on the membrane surface.
Acknowledgement
None
Conflict of interest
No conflict of interest
REFERENCES
- Rowland RN, Woodley JF (1981). The uptake of distearoylphosphatidylcholin/cholesterol liposomes by rat intestinal sac in vitro. Biochim. Biophys. Acta, 673:217-223.
Indexed at, Google Scholar
- Chengjiu H,David G. Proniosomes(1999).A novel drug carrier preparation. Int. J. Pharm.185:23-35.
Indexed at, Google Scholar, Crossref
- de Abreu LR, de Castro SA , Pedrauoli J(2003). Atenolol quantification in human plasma by high performance liquid chromatography: application to bioequivalence study. AAPS Pharm. Sci. 5: 1-7.
Indexed at, Google Scholar, Crossref
- Korsmeyer RW, Gurny R, Doelker E, Buri P, Peppas NA(1983). Mechanisms of solute release from porous hydrophilic polymers. Int. J. Pharm.15:25-35.
Indexed at, Google Scholar, Crossref
- Barry BW(2001). Novel mechanisms and devices to enable successful transdermal drug delivery. Eur. J. Pharm.Sci.14:101-14.
Indexed at, Google Scholar, Crossref
Citation: lsarr IA (2021) Modulatinn
intestinal uptake of Atenolol . Mol Enzy Drug
Targ, Vol.8 No. 3: 104.