Case Report
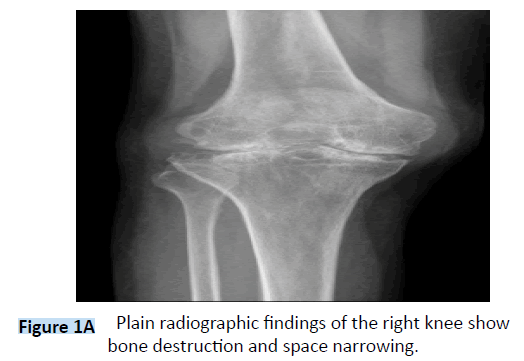
A 50-year-old man was evaluated because of 10 years of recurrent swelling and pain of knees and ankles. The patient was reported well until right knee pain occurred approximately 10 years before presentation [1]. He was treated by arthroscopic debridement 10 years ago and pain relieved after surgery. The pathological report showed PVNS. The right knee reported pain again 5 years before presentation and arthroscopic debridement was done plus radiation therapy after surgery [2,3]. Symptoms relieved one year before presentation, the patient reported right knee pain again, and left knee, bilateral ankles pain occurred this time, which would aggregate by exercise and relieve by rest (Figure 1A).
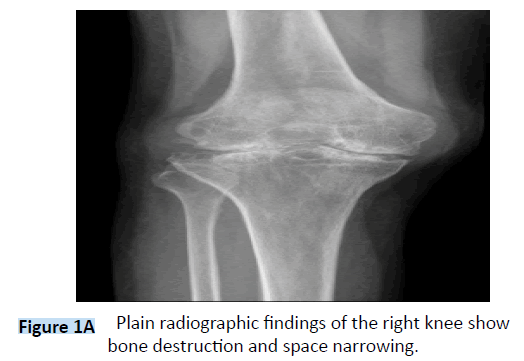
Figure 1A: Plain radiographic findings of the right knee show bone destruction and space narrowing.
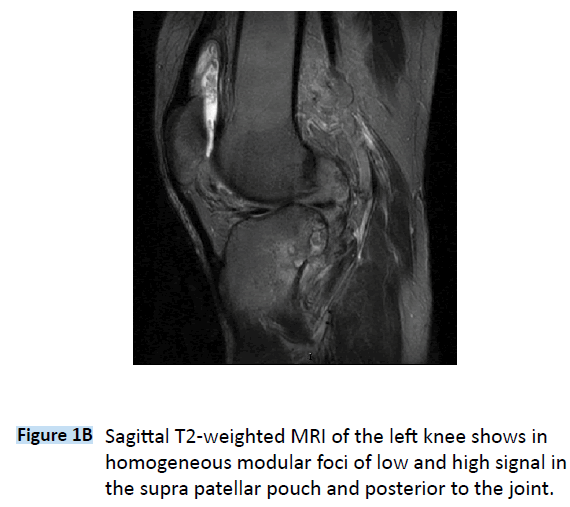
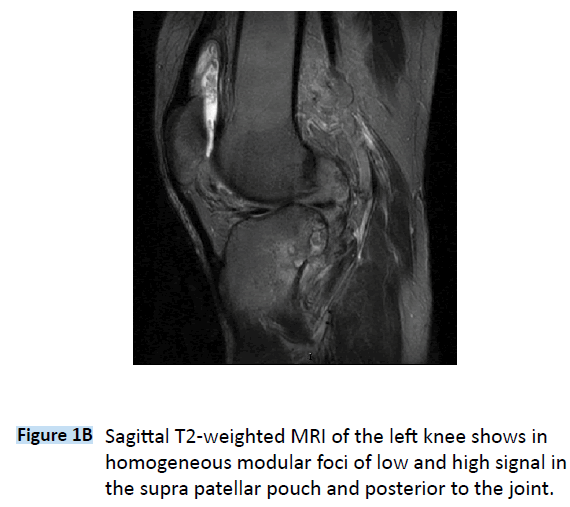
Figure 1B: Sagittal T2-weighted MRI of the left knee shows in homogeneous modular foci of low and high signal in the supra patellar pouch and posterior to the joint.
On examination, the patient showed claudication. The right knee showed mild varus deformity. The right knee range of motion was 10 to 110 degrees. The dermal temperature of left knee is higher than the right. The floating patella tests were positive in both sides. Tenderness were showed when the knee were palpated. The ankles showed mild swelling and normal range of motion. The blood parameters of creatine kinase, aspartate aminotransferase, lactate dehydrogenase and CRP were within normal limits. X-ray showed right knee space narrowing and joint destruction. Enhanced-MRI showed thicken synovial lining, nodular mass with blurred boundary, articular cartilage lesion and soft tissue swelling of bilateral knee joints, talonavicular joints, calcaneonavicular joints and calcaneocuboid joints. The dark-red bloody fluid was draw from right knee, which showed negative in bacterial and fungal culture. Positron emission tomography (PET) imaging was non-significant.
Above all, the clinical diagnosis was multifocal PVNS. Because the right knee lesion had progressed to end-stage osteoarthritis, total knee replacement was planned and done. And the left knee underwent arthroscopic debridement and open-up synovial resection through posterior approach. III degree articular injury was seen during right total knee replacement. The synovial membrane proliferated diffusely in left knee joint cavity, especially in suprapatellar bursa and lateral recess. Resected synovial membrane through arthroscopy and extra articular lesion through posterior approach. Pathological diagnosis was PVNS. The patient received low molecular weight heparin subcutaneously daily for 2 weeks for DVT prophylaxis. A continuous passive motion machine and sequential compressive devices were utilized. A standardized physical therapy protocol began on postoperative day one, and patients were encouraged to walk three times daily with supervision from nursing staff or their family. Two weeks after surgery, radiotherapy were done through knee and ankle. 6MV-X line radiated anteriorly and posteriorly. The total radiation dosage was 3000cGy (200cGy per time * 5 times per week). The radiation range was limited to 2cm outside of the joint cavity. His condition improved progressively and return to normal at the end
Discussion
PVNS is an uncommon disease. The prevalence is approximately 1.8 cases per 1 million population. And it is more common between ages from 20 to 50 years old, which has nearly equal incidence in male and female patients. PVNS could erosive cartilage and the surrounding bone, result in significant morbidity if left untreated. Pain, loss of function and eventual joint destruction may occur [4]. PVNS affects predominantly large joints, with the knee being the most common (80%) [5]. Other joints that may be affected by PVNS, in decreasing order of frequency, include the hips, ankles, small joints of the hands and feet, shoulders and elbows . It is typically a unifocal disease; however, a rare multifocal or multifocal involvement has been reported. This article reports a case of multifocal diffuse form of PVNS.
The etiology of PVNS still remains uncertain. Numerous mechanism, including chronic inflammation and neoplasia have been proposed [6]. The signs and symptoms of PVNS were mostly joint swelling and pain, sometimes palpable limited mass, joint dysfunction. The fluid drawn from PVNS joint was always dark red fluid. The MRI manifestations of PVNS were joint effusion, nodular proliferation of synovial membrane, bone marrow edema and articular cartilage destruction. Imaging, especially MRI, plays an important role in the diagnosis of PVNS. And this report is a typical case of PVNS.
The primary treatment option is synovectomy. Recurrence is reduced with complete resection, and it is achieved more often with localize form. Arthroscopic synovectomy now is becoming the standard surgical pattern [6]. While diffuse form of PVNS is more invasive and involves more joint, which makes it more difficulty to treat and more likely to recur. As Kotwal et al. [7] found, there are several factors that lead to relapse, including un-complete resection, mitotic activity and bone involvement. Diffuse PVNS has a tendency to invasive to the adjacent tissue. The lesion may invasive to tissue lower than the gastrocnemius or higher than the femoral condyle, which makes arthroscopy couldn’t find and resect, and relapse easily. Ogilvie-Harris et al. [8] reported that the recurrence rate of partial synovectomy through arthroscopy may up to 56%. Total synovectomy through open surgery is still the standard surgical approach [9]. Anterior and posterior approach through open surgery are also used by some surgeons [10]. Recurrence rate of open surgery is high in early report, and the recurrence rate is between 8-17% in recent reports [9,11]. A retrospective analyze done by Sharma et al. [12] showed the least recurrence rate of total synovectomy through anterior and posterior open surgery. Due to the large involvement of left knee, total synovectomy was done through arthroscopy and posterior open surgery.
Because the high recurrence rate after simple synovial resection, now radiation therapy may be used in concert with surgical excision to reduce the recurrence rate. Heyd et al. [13] reported that radiotherapy after surgery can make 82.9% of patients restore the joint function back to “well”. The study sum up 19 relevant studies, which include 140 cases, follow-up time up to 250 months, total radiation dose of 16-50Gy, 84.5% regional control rate. Griffin et al. [14] reviewed 50 patients treated with surgery and radiation, whose mean total radiation dose of 39.8Gy and men follow-up time of 94 months, only 6% of the patients had PVNS recurrence. This case had multi-joint involvement, which means high recur possibility and high difficulty in ankle synovectomy, radiotherapy of involve joints was added to avoid recurrence.
For PVNS involved with bone destruction or degenerative changes, total knee arthroplasty would be used as the primary treatment method to resect the lesion thoroughly, prevent recurrence, relieve pain, and improve joint function. Hamlin et al. [15] reported 18 cases of PVNS treated by TKA, whose follow-up time of 9.9 years old, mean Knee score of 89, and 14 cases don’t show loose of knee prosthesis. The patient in this case had joint destruction and severe pain, TKA could help in relieve pain and re-achieve joint function. Low molecular weight heparin is helpful for DVT prevention [16].
PVNS involved in multi-joint is rare, which should be evaluated and treated as early as possible. And total synovectomy plus radiotherapy is the best treatment option and prevent recurrence.
6482
References
- Granowitz, S.P., D'Antonio, J., Mankin, H.L. The pathogenesis and long-term end results of pigmented villonodularsynovitis.ClinOrthopRelat Res 1976; 114: 335-351.
- Miller WE. Villonodularsynovitis: pigmented and nonpigmented variations.South Med J 1982; 75: 1084-1086, 1092.
- Kay, R.M., Eckardt, J.J., Mirra, J.M. Multifocal pigmented villonodularsynovitis in a child. A case report.ClinOrthopRelat Res 1996; 194-197.
- Myers, B.W., Masi, A.T. Pigmented villonodularsynovitis and tenosynovitis: a clinical epidemiologic study of 166 cases and literature review.Medicine (Baltimore) 1980; 59: 223-238.
- Kramer, D.E., Frassica, F.J., Frassica, D.A., Cosgarea, A.J. Pigmented villonodularsynovitis of the knee: diagnosis and treatment.J Knee Surg 2009; 22: 243-254.
- Loriaut,P., Djian, P., Boyer, T., Bonvarlet, JP.,Delin, C., et al. Arthroscopic treatment of localized pigmented villonodularsynovitis of the knee.Knee Surg Sports TraumatolArthrosc 2012; 20: 1550-1553.
- Kotwal, P.P., Gupta, V., Malhotra, R. Giant-cell tumour of the tendon sheath. Is adiotherapy indicated to prevent recurrence after surgery?J Bone Joint Surg Br 2000; 82: 571-573.
- Ogilvie-Harris, D.J., McLean, J., Zarnett, M.E. Pigmented villonodularsynovitis of the knee. The results of total arthroscopic synovectomy, partial, arthroscopic synovectomy, and arthroscopic local excision. J Bone Joint Surg Am 1992; 74:119-123.
- Chin, K.R., Barr, S.J., Winalski, C., Zurakowski, D., Brick, G.W. Treatment of advanced primary and recurrent diffuse pigmented villonodularsynovitis of the knee.J Bone Joint Surg Am 2002; 84-A(12): 2192-2202.
- Wu, C.C., Pritsch, T., Bickels, J., Wienberg, T., Malawer, M.M. Two incision synovectomy and radiation treatment for diffuse pigmented villonodularsynovitis of the knee with extra-articular component.Knee 2007; 14: 99-106.
- Flandry,F.C., Hughston, J.C., Jacobson, K.E., Barrack, R.L., McCann, S.B., et al. Surgical treatment of diffuse pigmented villonodularsynovitis of the knee. ClinOrthopRelat Res 1994; 300: 183-192.
- Sharma, V., Cheng, E.Y. Outcomes after excision of pigmented villonodularsynovitis of the knee.ClinOrthopRelat Res 2009; 467: 2852-2858.
- Heyd, R., Seegenschmiedt, M.H., Micke, O. The role of external beam radiation therapy in the adjuvant treatment of pigmented villonodularsynovitis. Z OrthopUnfall 2011; 149: 677-682.
- Griffin, A.M., Ferguson, PC., Catton, C.N., Chung, P.W., White, L.M., et al. Long-term outcome of the treatment of high-risk tenosynovial giant cell tumor/pigmented villonodularsynovitis with radiotherapy and surgery. Cancer 2012; 118: 4901-4909.
- Hamlin, B.R., Duffy, G.P., Trousdale, R.T., Morrey, B.F. Total knee arthroplasty in patients who have pigmented villonodularsynovitis. J Bone Joint Surg Am 1998; 80: 76-82.
- Ciccone, M.M., Cortese, F., Corbo, F., Corrales, N.E., Al-Momen, A.K., et al. Bemiparin, an effective and safe low molecular weight heparin: a review. VasculPharmacol 2014; 62: 32-37.