Introduction
Human cystic echinococcosis is a chronic zoonotic disease that results from infection with the larval stage of the dog tapeworm, Echinococcus granulosus. The disease is highly endemic in most Mediterranean and Middle Eastern countries. In Iran, the annual incidence rate of hydatidosis has decreased from 0.72/10,000 in 2002 to the current estimate of 0.61/100,000 some regions having the highest incidence rates (1.33 cases/ 100,000) [1]. Eggs are passed though dog feces and transmitted via oral route to an intermediate host such as humans and larvae subsequently lodge in organs such as the liver (70% of cases), lungs (22% of cases) or others such as heart, brain, kidney, spleen, muscle, skeletal system, skin (8% of all cases in total) [2]. Simultaneous hydatid cysts in liver and lung are rare and constitute about 5-13% of all cases [3].
Homemakers and farmers living in rural areas where contact with animals such as dogs or sheep is more common, have the highest rate of infection (51.3%-75%). The most probable cause of infection in other patients is believed to be the ingestion of contaminated or uncooked foods or raw vegetables [1,4].
We report the case of a 35year- old woman who presented to our hospital with multiple cystic lesions in the liver and lung.
Case Report
An otherwise healthy 35-year-old woman presented to our hospital with the acute onset of severe sharp right upper quadrant abdominal pain of 5 days duration. She also complained of one day of severe cough associated with blood-tinged sputum, wheezing, fever, and generalize bony pain. History of loose stools and an approximate 6 kg weight loss in the prior month was also elicited.
She worked as a fruit-picker in the western Iranian province of Hamedan and reported close contact with cattle and dogs.
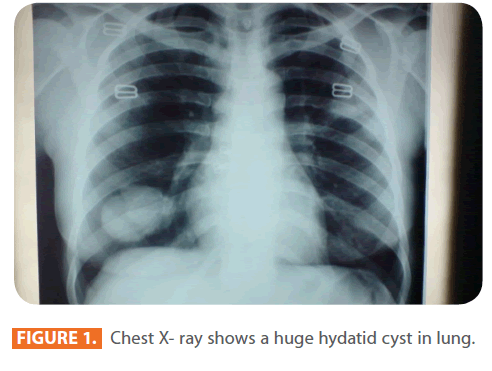
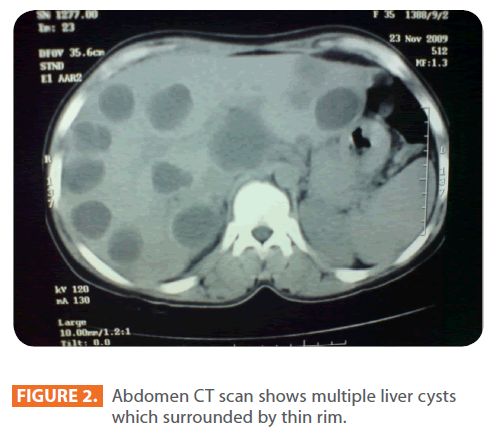
On physical exam she had blood pressure of 105/75mmHg, and a respiratory rate of 32 breaths per minute. Her heart, lung and abdominal exam were within normal limits. On routine laboratory work up her complete blood count and serum biochemistries profile were unremarkable with a White Blood Count (WBC) of 12000/ml. Eosinophil count was 26 (19%) per/mm3, and Neutrophil count was 39 (47%) per/mm3, a Hemoglobin of 12g/dl, a Platelet Count (PLT) of 187000/mm3, an Erythrocyte Sedimentation Rate (ESR) of 37 mm/hr, an Alanine Aminotransferase (ALT) and Aspartate Aminotransferase (AST) of 22 and 24 Us/L, respectively. On serological examination, her hydatid cyst antibody (IgGAb) was positive. On chest X-ray, a four cm3 lesion was noted in the inferior right lobe of her lungs hydatid disease; cyst with internal structures and possibly calcific shell (fig 1) and her abdominal CT scan showed multiple cystic lesions in the liver (fig 2).
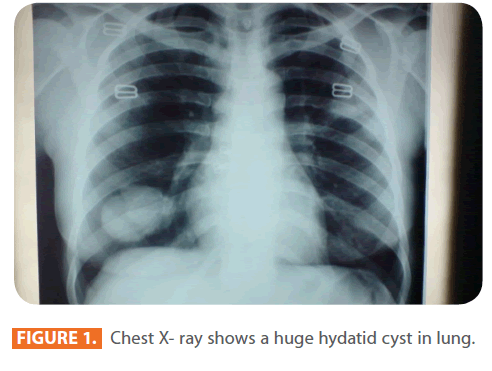
Figure 1: Chest X- ray shows a huge hydatid cyst in lung.
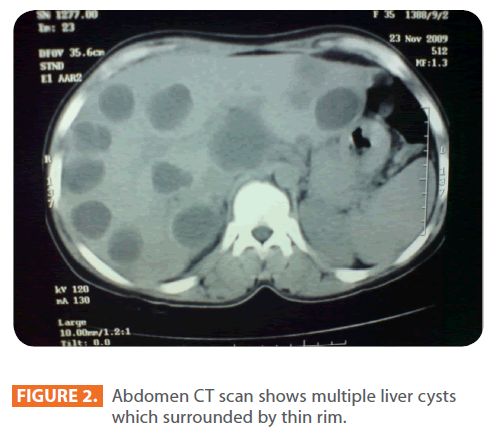
Figure 2: Abdomen CT scan shows multiple liver cysts which surrounded by thin rim.
Based on the above findings, the patient was diagnosed with echinococcosis and was started on 400 mg of oral albendazole twice daily for duration of 28 days. The same treatment was repeated with a 14-days interval for another 3 cycles.
After the treatment course was finished, imaging from chest did not show any lesions and the patients did not have any clinical manifestations.
Review of literature
In contrast to adults where the liver is the most effected organ, in children 77% of the cases involve the lungs. Hydatid cysts can grow as much as 5–10 cm in size within the first year of infection and can survive for years or even decades after that. Infection is often asymptomatic and cysts are often detected incidentally during imaging work up for other conditions. When symptoms do occur, they are usually due to the spaceoccupying effect of the enlarging cyst in a confined space [4].
The clinical presentation of hydatid disease depends on the size and site of the growing cysts. Some cysts may produce dysfunction of involved organs, including biliary obstruction, cirrhosis, bronchial obstruction, renal outflow obstruction, increased intracranial pressure, and hydrocephalus [3]. Complications associated with the free rupture of the echinococcal cyst may cause anaphylaxis and smaller cysts may be released that can circulate to and lodge in other organs [3]. The presence of cysts can be confirmed through imaging studies such as ultrasound or CT scans. The CT scan has an accuracy of 98% in detecting daughter cysts, and is the best test to differentiate hydatid cysts from amebic or pyogenic cysts of the liver. A thin rim of calcification delineating a cyst is suggestive of an echinococcal cyst [5].
The low efficacy of eosinophilia is according to increasing the incidence of false positivity in endemic regions with other parasitic infestation .Nevertheless, when eosinophilia is found in a patient with cysts in relation to liver, investigations should begin in order to rule out hydatid disease by surgery or drug treatment [6-7]. Among the radiological investigations, CT was diagnostic of hydatid disease in all patients (sensitivity 100%), CT also allows differentiation of cysts from solid lesions precise assessment of its relationship to neighboring organs [8]. Surgery and drug therapy have been used for treatment of hydatid cyst disease [9]. Mortality rates of patients undergoing a surgical intervention are reported to be 0-6.3%, depending on the method applied. This rate may increase to 8.0% in complicated cases. Recurrence after surgery has been reported to be 2.2-22% [9].
In recent years, medical and percutaneous drainage methods have been used as alternatives to surgery for the treatment of hydatid cyst disease. Albendazole and mebendazole have been used extensively in the treatment of hydatid cyst since 1977 [10]. Albendazole (10 mg/kg body weight) is an effective and reliable method for the treatment of recurrent hydatid cysts and its scolicidal effect can be seen mostly at the second and third months [11]. In regions where hydatid disease is endemic, it should be included in the differential diagnosis of eosinophilias.
226
References
- Rokni MB. (2009) Echinococcosis /hydatidosis in Iran. Iran J Parasitol 4: 1-16.
- Rahdar M, MaraghiSH ,Rafei A, Razijalali M. (2008) Comparison of some electrolytes in hydatid cyst fluid and serum of liver hydatidosis of sheep. Jundishapur J. Microbiol 1: 10-14
- Pan Z, Hunter WJ. (2007) Hydatid Cyst of the Liver: A Case Report and Review of the Literature. The Internet Journal of Parasitic Diseases 2:1.
- Mamishi S, Sagheb S, Pourakbari B. (2007). Hydatid disease in Iranian children. J MicrobiolImmunol Infect 40: 428-431.
- Guntz M, Coppo B, Lorimier G, Cronier P. (1990) Hydatid cyst of the liver appearing late (10-22 years) after surgical treatment of pulmonary hydatidosis. Physiopathologic problems J Chir Paris 127: 375-81.
- Saidi F. (1976) Hydatid cyst of the kidney. In: Saidi F, ed. Surgery of Hydatid Disease. London: Saunders pp. 217–249.
- Gö?gü¸s O, Be”uk Y, Topukçu Z (1991) Renal hydatid disease. Br J Urol68: 466.
- Gilsanz V, Lozano F, Jimenez J (1980) Renalhydatid cysts: Communicating with collecting system. AJR 135: 357.
- Mentes A. (1994) Hydatid liver disease. a perspective in treatment. Dig Dis 12:150-160.
- Erzurumlu K, Sahin M, Selcuk MB, Yildiz C, Kesim M (1996). Intracystic application of mebendazole solution in the treatment of liver hydatid disease. EurSurg Res. 28:466-470
- Wilson T, Cossetto D, Gruenwald S, Antico V, Hollands M, et al (1990) Treatment of recurrent hydatid disease with albendazole. Third World Congress on Hepatobiliary Surgery, London, J HepatobiliaryPancreatSurg2[suppl]:156