Sagrario Maria Santos Seoane*
Hospital San Agustin, Camino Heros 6, Aviles, Asturias, 33401, Spain
*Corresponding Author:
Sagrario Maria Santos Seoane
Hospital San Agustin, Camino Heros 6
Aviles, Asturias, 33401, Spain
Tel: +34620318904
E-mail: smsspulp@yahoo.es
Received date: July 06, 2017; Accepted date: July 12, 2017; Published date: July 20, 2017
Citation: Seoane SMS (2017) Multiple Plasmacytoma. Ann Clin Lab Res. Vol.5:No.3:182. doi:10.21767/2386-5180.1000182
Multiple solitary plasmacytomas is defined as the presence of more than one plasmacytoma (occurring concurrently or sequentially) in the absence of bone marrow evidence of multiple myeloma. Approximately 30 to 50 percent of patients with suspected solitary plasmacytoma of bone will have multiple asymptomatic lesions detected by PET/CT or MRI of the spine. Many clinicians advocate the use of local radiation directed at the symptomatic site with further treatment postponed until the development of symptoms. For others, the treatment is considered depending upon the number and location of involved sites. If a patient has two different concurrent plasmacytomas without involvement of the bone marrow, it would be treated with radiotherapy in both places, followed by observation as long as the radiation fields are limited. If the radiation fields are large and may interfere with the collection of stem cells or bone marrow reserve, a systemic therapy identical to that used for MM instead of radiation would be administered. If a patient has more than two concurrent lesions, a systemic therapy identical to that used for multiple myeloma would be administered, even if the bone marrow is normal. If the patient develops two or three apparently solitary lesions within a period of one to two years, subsequent therapy should be as if the patient has multiple myeloma. Keywords :
Clinical Image
Multiple solitary plasmacytomas is defined as the presence of more than one plasmacytoma (occurring concurrently or sequentially) in the absence of bone marrow evidence of multiple myeloma.
Approximately 30% to 50% of patients with suspected solitary plasmacytoma of bone will have multiple asymptomatic lesions detected by PET/CT or MRI of the spine.
Many clinicians advocate the use of local radiation directed at the symptomatic site with further treatment postponed until the development of symptoms. For others, the treatment is considered depending upon the number and location of involved sites.
If a patient has two different concurrent plasmacytomas without involvement of the bone marrow, it would be treated with radiotherapy in both places, followed by observation as long as the radiation fields are limited. If the radiation fields are large and may interfere with the collection of stem cells or bone marrow reserve, a systemic therapy identical to that used for MM instead of radiation would be administered.
If a patient has more than two concurrent lesions, a systemic therapy identical to that used for multiple myeloma would be administered, even if the bone marrow is normal.
If the patient develops two or three apparently solitary lesions within a period of one to two years, subsequent therapy should be as if the patient has multiple myeloma.
Clinical Case
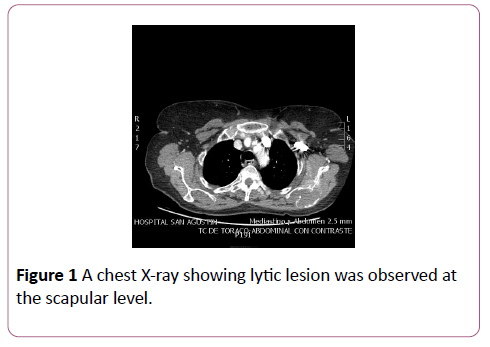
We present the case of an 84-year-old woman who consulted for pain in the left hemithorax irradiated to the lumbar region, without fever, cough or hemoptysis but with decreased appetite in the last weeks without weight loss. The chest X-ray showed a left pleural effusion. A thoracentesis was performed, confirming the presence of a lymphocytic exudate with high proteins (5.47 gram). The pleural biopsy as well as cultures and flow cytometry were negative. The TAC showed a large hypercaptive mass in the posterior mediastinum, which displaced the aorta and esophagus, behind the left atrium to the spinal column (Figure 1), which extended to the wheight of the kidneys, and another mass of the same characteristics in the left posterior pararenal space (Figure 2). Biopsy of the retroperitoneal mass was performed, confirming the diagnosis of plasmacytoma (CD138+, CD20, cytokeratin AE1/AE3-, S100-). The percentage of plasma cells in MO was 0.1% and immunofixation revealed a monoclonal IgA (1419)/Lambda (443) peak. The final diagnosis was giant mediastinalretroperitoneal plasmocytoma with left pleural effusion and monoclonal IgA-lambda secretion. Radiotherapy was started.
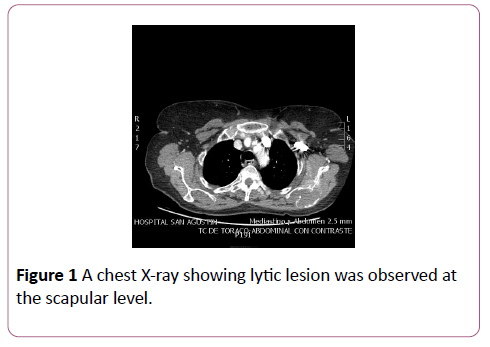
Figure 1: A chest X-ray showing lytic lesion was observed at the scapular level.
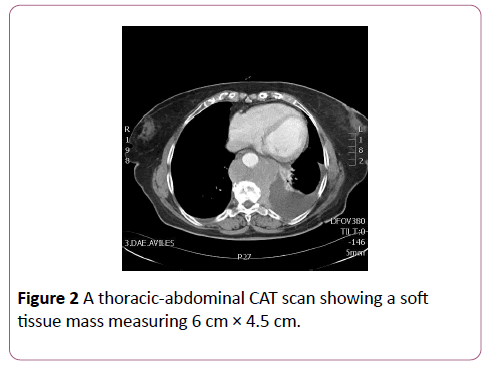
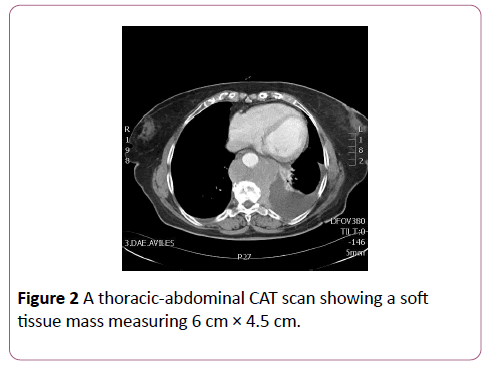
Figure 2: A thoracic-abdominal CAT scan showing a soft tissue mass measuring 6 cm × 4.5 cm.
Three years later, she started with pain at the left shoulder level. In addition, the patient had been evaluated by ORL weeks before for headache and left tinnitus, and she was pending to perform a cranial CT of ambulatory form. A chest xray was performed and a lytic lesion was observed at the scapular level (Figure 1). A thoracic-abdominal CAT scan was then requested, with a soft tissue mass measuring 6 cm × 4.5 cm with lysis at the level of the left scapula (Figure 2). The cranial CT scan revealed the presence of another soft tissue mass at level of the left petrosal apex with thinning/lysis of the locoregional cortex, and which was rodened the internal carotid artery (Figure 3). Biopsy of the scapular mass was performed confirming the presence of a new plasmacytoma. Treatment with cycles of melphalan, prednisone and velcade biweekly was initiated, as well as zolendronic acid very 4 weeks, with reduction of both lesions.

Figure 3: The cranial CT scan revealing the presence of another soft tissue mass at level of the left petrosal apex.
20250