Keywords
Ebola outbreak; Nigeria; Lessons learned; Outbreak response; Epidemic preparedness
List of Abbreviations
BSL: Biosafety Level; CDC: Centers for Disease Control and Prevention; EVD: Ebola Virus Disease; DNA: Deoxyribonucleic Acid; ETC: Ebola Treatment Center; EEOC: Ebola Emergency Operations Center; FMOH: Federal Ministry of Health, HR: Human Resources, IDSR: Integrated Disease Surveillance and Response; IHR: International Health Regulations; IPC: Infection Prevention and Control; MOH: Ministry of Health; MSF: Médecins Sans Frontieres; NFELTP: Nigeria Field Epidemiology and Laboratory Program; NGO: Non-governmental Organization; RT-PCR: Reverse Transcriptase-Polymerase Chain Reaction; VHF: Viral Hemorrhagic Fever; WHO: World Health Organization
Introduction
An extra-ordinary outbreak of Ebola which started in Guinea in December 2013 rapidly spread to Liberia and Sierra Leone in 2014 affecting at least eight countries with 28,646 cases and over 11,323 deaths [1]. The disease was introduced into Nigeria on the 20th July 2014 by a 40 year old man who arrived Lagos by air from Liberia. It was the first time EVD was spread to any country by air travel [2]. The introduction also marked the onset of Nigeria’s first outbreak of Ebola virus disease (EVD) which lasted between July and September 2014, affected two complex mega cities, Lagos and Portharcourt with a combined population of 25 million and a high influx of people from neighboring countries with limited supportive infrastructure. Many crowded slums and squatter settlements exist in both cities providing a good setting for the rapid spread of EVD and making control difficult. The spread of EVD to Lagos caused great concern in the international community and triggered the declaration of a Public Health Emergency of International Concern (PHEIC) by the Director General of the World Health Organization (WHO). Overall, the outbreak recorded 20 cases were with 8 deaths, and was declared over by the WHO on October 20, 2014 [3].
The Nigerian Centre for Disease Control (NCDC) of the Federal Ministry of Health (FMOH) in collaboration with the State Ministries of Health in Lagos and Rivers States utilized existing local capacities and the Integrated Disease Surveillance and Response (IDSR) system to rapidly diagnose and control the EVD, while also repurposing existing public health resources to address the new challenges posed.
This paper describes the key activities of the response, highlights key achievements and presents major lessons learned and implications for future epidemic preparedness. These could provide valuable information for developing countries that are reinforcing their epidemic preparedness and response capacities for future outbreaks of EVD and other epidemic-prone diseases.
Methods
The EVD response in Nigeria was led by the NCDC of the federal ministry of health in collaboration with the Lagos and Rivers States Ministry of Health, research and academic institutions, private sector organizations and international technical partners. The approach used was a coordinated and integrated rapid implementation of EVD control measures using multidisciplinary teams [4].
Standard case definition
The WHO standard case definition for EVD was adapted and used:
Suspected case definition: A suspected EVD case under investigation is defined as any person with or without known history of travel or stay in a country that has reported contact with at least one confirmed case of EVD, within a period of 21 days before the onset of symptoms [5], and who presents with:
Sudden onset of high fever (>38.0°C) and at least three of the following symptoms:
• Headache, vomiting, diarrhea, anorexia/loss of appetite, lethargy, stomach pain, aching muscles or joints, sore throat, and difficult breathing (or)
• Inexplicable bleeding/hemorrhaging (or)
• Inexplicable sudden death
A probable case: A suspected case evaluated by a clinician (or)
Any deceased suspected case (where it has not been possible to collect specimens for laboratory confirmation) having an epidemiological link with a confirmed case.
A confirmed case: A suspected case with laboratory confirmation (positive IgM antibody, positive RT-PCR or viral isolation).
Rapid case investigation and laboratory diagnosis
Laboratory analysis of blood samples from suspected EVD cases were carried out at the virology laboratory of the Lagos University Teaching Hospital (LUTH)-a BSL II laboratory with known RT-PCR capacity for diagnosing viral hemorrhagic fevers (e.g. Lassa fever) in the country. Laboratory investigation using Pan Filo wobble primers for blood samples were undertaken. Dengue and Lassa viruses were analyzed in samples negative for EVD. In addition, Pan Filo virus and Ebola Zaire MGB virus strain specific genomic analysis were conducted at the World Bankfunded African Centre of Excellence for Genomics of Infectious Diseases (ACEGID), Redeemers’ University in Ogun State to detect the Ebola Zaire viral DNA in blood samples. Samples were shipped for further confirmatory analysis and quality assurance to the WHO Collaborating laboratory for VHF-the Bernhard Notch Institute Hamburg.
In Port Harcourt, a mobile laboratory was established at the University of Port Harcourt Teaching Hospital (UPTH) by the laboratory staff from the Lassa Fever Research and Training Institute, Irrua with the support of WHO.
Contact tracing, active case search and rapid control efforts
Contact tracing and follow-up was conducted according to a national standard operating procedure (SOP) adapted from WHO [6]. Trained contact tracers comprised Residents of the Nigeria Field Epidemiology and Laboratory Training Program (NFELTP), Epidemiologists from the NCDC and Lagos and Rivers States Ministry of Health and WHO surveillance officers.
A contact was defined as any person without any disease signs and symptoms but had physical contact with a case (alive or dead) or the body fluids of a case within the last three weeks. Physical contact includes sharing the same room/bed, caring for a patient, touching body fluids, or closely participating in a burial.
All contacts to a confirmed case were identified, listed and classified into the four following categories to reflect the level of risk associated with the exposure
• Touched body fluids of the case (blood, vomit, saliva, urine, feces)
• Had direct physical contact with the body of the case (alive or dead)
• Touched or cleaned the linens, clothes, or dishes of the case
• Slept or ate in the same household as the case
Daily temperature measurements were recorded by the contact tracers on an android mobile phone application with GIS features, which also recorded the location of the assessment against the registered residential address of the contacts. Contacts were reclassified as suspected cases if they were observed to have temperature ≥ 37.5°C axillary or ≥ 38.0°C core and met one of the following criteria:
• Had vomiting, diarrhea, or bleeding from stool or mucous membranes; or
• Had two additional symptoms including headache, myalgia, arthralgia, or weakness.
The contacts were counseled, advised on social distancing during the period of 21 days of monitoring. The mobile phone application was centrally monitored real-time at the Ebola Emergency Operations Centre. This was used as an innovation in the response for data collection by contact tracers. It also ensured that all contacts were effectively tracked and eliminated provision of fictitious information by some contact tracers without physically visiting a contact [7]. A few contacts proved very difficult to follow-up or escaped follow-up. Special teams were set up to track such non-compliant contacts.
Alert and rumor management
An alert and rumor management system was established and alert teams were sensitized in all other states in the country to investigate and respond to any alert, rumor of a suspect case or escape contact, and conduct active case search. Toll-free telephone lines were opened to the public to report suspicious cases using community case definitions, and improve early case detection. The toll-free lines, manned by trained health workers were widely disseminated alongside preventive measures through awareness campaigns in the electronic and social media. Members of the public were encouraged to call in when they have alert cases or when they have any query. All incoming alert calls were registered using alert forms and the information conveyed to the relevant team or alert team for verification/ investigation.
Managing the cases
Ebola Treatment Centres (ETC) were established in Lagos and Port Harcourt to manage suspected and confirmed cases of EVD using a clinical management protocol. In Lagos, a 40-bed ETC was established by the Lagos State MOH with the support of the NCDC at the Mainland hospital, Yaba with another surge facility with a capacity of 10 beds. The ETC was managed by WHO, MSF, and Nigerian health workers. A team of Nigerian health workers including 15 doctors, 28 nurses and 16 ancillary staff were identified and trained on Ebola case management and infection prevention and control (IPC) by WHO. These personnel provided 24 hours care alongside the WHO and MSF staff.
In Port Harcourt, a 26 bed ETC was established by the Rivers state MOH supported by Partners, with a surge capacity of 8 beds. A team of 12 doctors, 24 nurses and 24 environmental health officers drawn from Rivers State MOH, WHO and MSF were trained and worked at the ETC. All ETCs were fully equipped with medicines and consumables, personal protective equipment (PPEs), body bags, communication facilities and ambulances.
Decontamination and burial teams disinfected the homes of all cases, and vehicles including ambulances, and conducted safe burials of the deceased respectively.
Safeguarding the points of entry (PoE)
The point of entry team carried out entry and exit screening under the leadership of the Port Health Service and supported by airport, seaport and land border authorities [8]. They also worked with airline operators, national aviation authorities, immigration, maritime, custom and security officials to establish screening facilities and protocols for checking temperatures and screening of incoming and exiting passengers in Lagos and Portharcourt airports, sea ports and ground crossings. 500 Volunteers were engaged and supplied with 1247 thermo-scans for temperature screening. Holding facilities were also set up at the PoE to temporarily keep any detected suspected case before transfer to the ETC in an ambulance for further evaluation. Personal Protective Equipment (PPE) was supplied to the PoE team for use when handling suspected cases.
Involving the community and creating public awareness
Ebola key messages on preventive measures were distributed from house to house by trained community mobilizers. Community sensitization meetings were held with traditional and religious leaders, school teachers, market women associations, youth organizations and the Association of General and Private Medical Practitioners of Nigeria (AGPMPN). Electronic, print and social media platforms were also used to disseminate information to members of the public to increase their awareness of EVD.
Ensuring effective coordination of the response
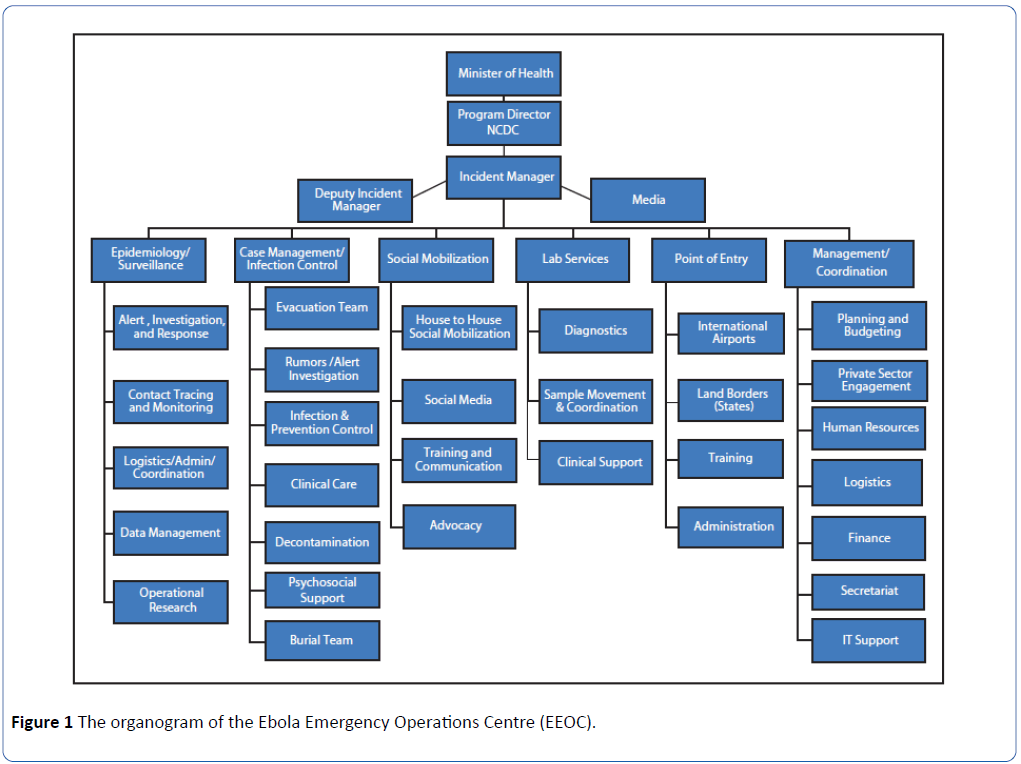
Ebola Emergency Operations centers were established in Lagos and Port Harcourt by the NCDC in collaboration with the State Ministries of Health in Lagos and Port Harcourt and international Partners to ensure an effective and efficient coordination of the response. An Incident Management System (IMS) was introduced by the FMOH under the oversight of the NCDC, and response teams and operations were streamlined for a more efficient and rapid response (Figure 1).
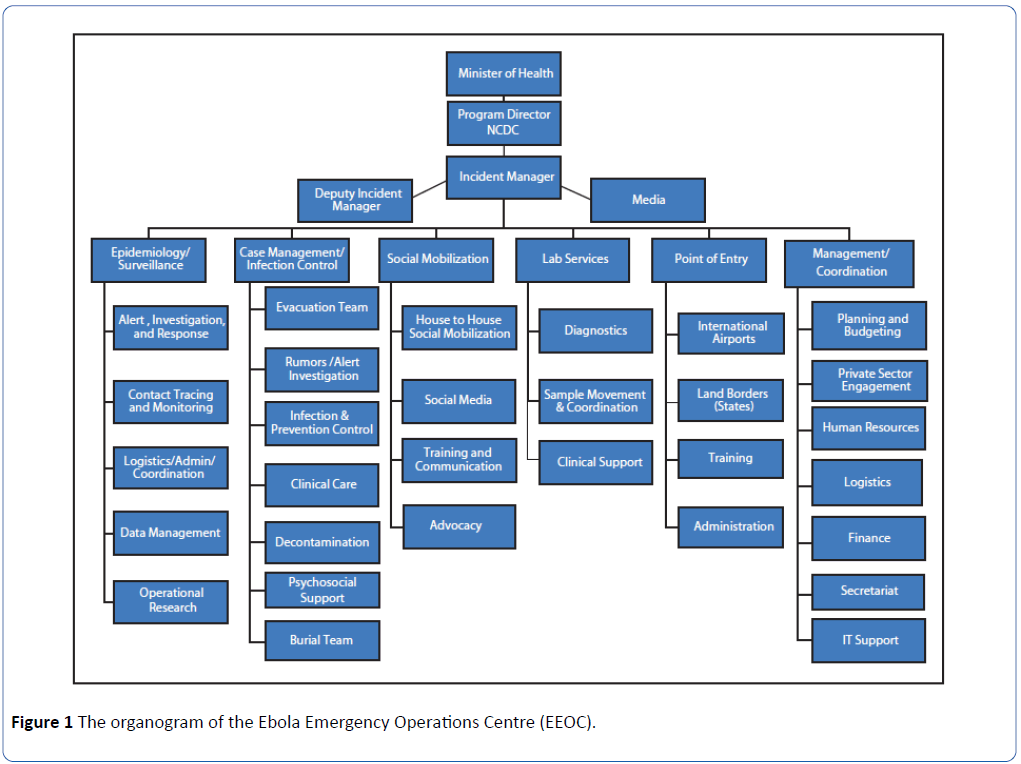
Figure 1: The organogram of the Ebola Emergency Operations Centre (EEOC).
The response teams were organized into (i) Epi-surveillance comprising alert/rumor management, contact tracing, data management and operations research, (ii) Case management comprising clinical management, Rapid response, infection prevention and control, psychosocial support, decontamination, burial sub teams; (iii) social mobilization, (iv) Points of entry and (v) Management and coordination comprising HR, administration/finance, and logistics/procurement. Each response team had a Leader working with the sub-team heads, under the overall leadership of an Incident Manager. A technical strategy group chaired by the Incident Manager provided the day-to-day strategic direction on the management of the response and had representatives of the NCDC, State MOH, the Team Leads of WHO, UNICEF, MSF and CDC as members. A daily situation report of the response activities was disseminated to all stakeholders.
Providing strong political leadership
The President of Nigeria declared the EVD outbreak as an emergency within 24 hours of its diagnosis. All Commissioners of health and state Governors were directed to take all necessary measures to prevent the spread of the disease in the country. The Governors also transmitted the same message to the local government Chairmen in their respective States. The Minister of health as the Chief public health officer of the country assumed the day-to-day overall coordination of the response and reported progress regularly to the president and the executive council.
Results
The EVD outbreak in Nigeria occurred from July to September 2014 in the two large cities of Lagos and Portharcourt.
Transmission pattern
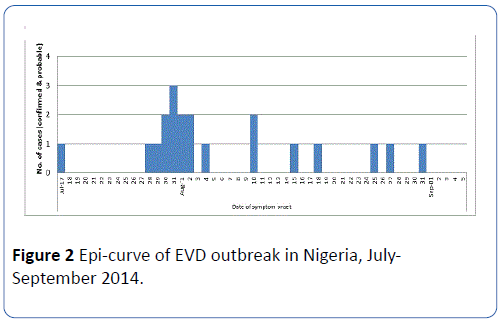
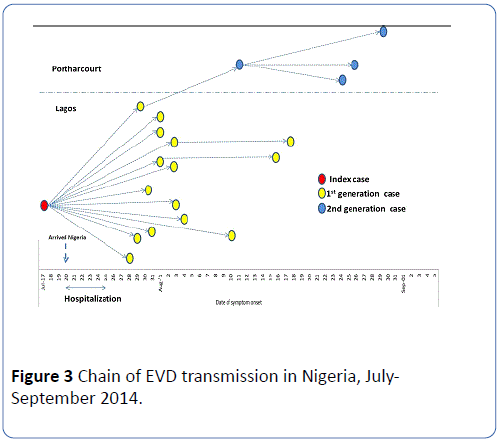
In Lagos, a total 16 cases were recorded (15 confirmed, 1 probable) and 6 deaths, while in Port Harcourt, 4 confirmed cases with 2 deaths were recorded giving a total of 20 cases and 8 deaths (CFR 40%) (Table 1). The epi-curve displaying the onset of illness of all confirmed cases (confirmed and probable) associated with the outbreak is showed in Figure 2; the transmission chain is shown in Figure 3.
| Description |
Lagos
N (%) |
Portharcourt
N (%) |
Total
N (%) |
| Cases: |
16 (80.0) |
4 (20.0) |
20 (100.0) |
| Confirmed |
15 (75.0) |
4 (20.1) |
19 (95.0) |
| Probable |
1 (5.0) |
0 (0.0) |
1 (5.0) |
| Deaths |
6 (75.0) |
2 (25.0) |
8 (100.0) |
| Confirmed |
5 (62.5) |
2(25.0) |
7 (87.5) |
| Probable |
1 (12.5) |
0 (0.0) |
1 (12.5) |
| Case Fatality Rate: Confirmed and probable (%) |
-40 |
-50 |
-40 |
| Cases among healthcare workers |
9 (81.8) |
2 (18.2) |
11 (100.0) |
| Deaths among healthcare workers |
4 (80.0) |
1(20.0) |
5 (100.0) |
| Confirmed cases admitted into ETC* |
11 (84.6) |
2 (15.4) |
13 (100.0) |
| Discharged |
7 (53.8) |
1 (7.7) |
8 (61.5) |
| Died |
4 (30.8) |
1 (7.7) |
5 (38.5) |
| *ETC: Ebola Treatment center |
Table 1: Summary of EVD cases, deaths and ETC discharges in Nigeria, July-September 2014.
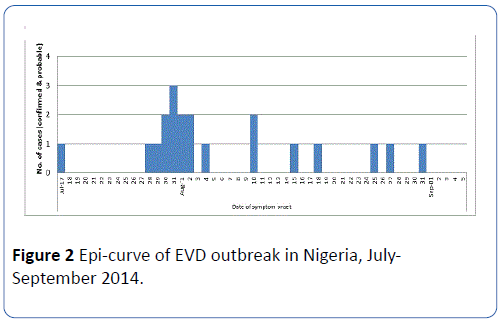
Figure 2: Epi-curve of EVD outbreak in Nigeria, July-September 2014.
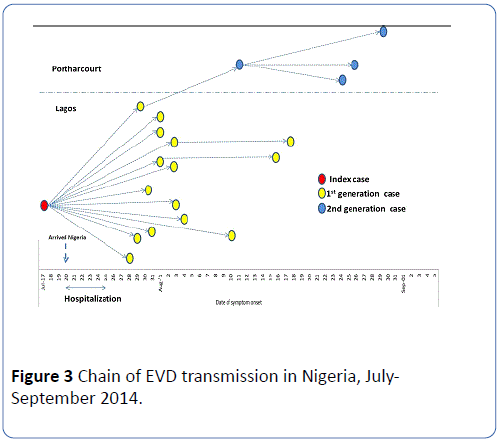
Figure 3: Chain of EVD transmission in Nigeria, July-September 2014.
Contact tracing
A total of 892 contacts were listed for daily follow-up. In Lagos, 362 (40.6%) contacts were registered comprising 70 primary contacts of the index case and 292 secondary contacts located in 17 local government areas of Lagos State. They were all followed-up for 21 days by 15 contact tracing teams. In Port Harcourt, a total of 530 (59.4%) primary contacts were listed from 7 local government areas of Rivers State and were followed up by 30 teams of contact tracers for 21 days (Table 2).
| Description |
Lagos
N (%) |
Portharcourt
N (%) |
Total
N (%) |
| Number of contacts listed |
362 (40.6) |
530 (59.4) |
892 (100.0) |
| Contacts monitored for 21 days |
362 (40.6) |
530 (59.4) |
892 (100.0) |
| Contacts lost to follow-up |
0 |
0 |
0 |
| Number of LGAs covered* |
17 (70.8) |
7 (29.2) |
24 (100.0) |
| Number of contact tracing teams |
18 (37.5) |
30 (62.5) |
48 (100.0) |
| *LGA: Local Government Area (of contact’s residence) |
Table 2: Contact tracing during the EVD outbreak response in Nigeria, July-Sept 2014.
Alert and rumor management
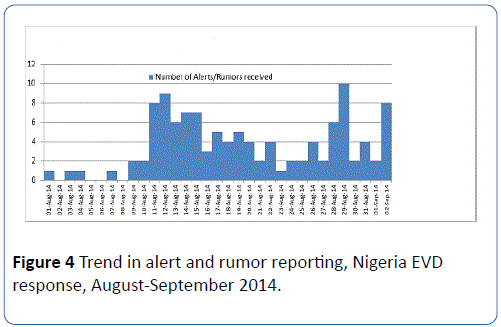
A total of 117 alerts and rumors were reported and investigated between August and September, 2014. All alerts and rumors were investigated within 24 hours (Figure 4).
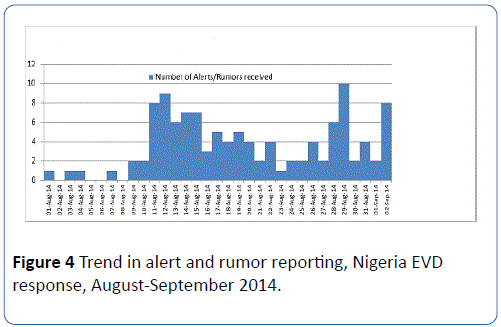
Figure 4: Trend in alert and rumor reporting, Nigeria EVD response, August-September 2014.
Case Isolation and management
Thirteen confirmed cases were isolated in the ETC; 11 (84.6%) in Lagos and 2 (15.4%) in Port Harcourt, River state. Of these 7 died in the ETC, one died at home and the other one is the index case that died at the admitting health facility. One confirmed case in Port Harcourt was transferred to Lagos ETC (Table 1).
Discussion
Lessons learned and implications for future epidemic preparedness
The response to the EVD outbreak in Nigeria provided important insights into the elements in epidemic preparedness and response that countries need to take into consideration in leveraging health system changes aimed at bolstering population health security.
The first lesson learned is that building a critical pool of incountry technical expertise in field epidemiology, laboratory, clinical care, anthropology and psychosocial support for immediate deployment as rapid response teams in outbreak settings can help to truncate infectious disease transmission. This capacity should be established in all the different regions of the country and equipped with rapid deployment capabilities. Nigeria deployed a rapid response team comprising NFELTP residents, clinicians, MOH and in-country partners including from the private sector with sufficient capacities, hence the response was effective. Contact tracing was done by field epidemiologists from the NFELTP and WHO surveillance officers from the Polio program. This improved the quality of contact tracing, a feat that was aptly described by WHO as “a piece of world class epidemiological detective work” [3]. Additionally, the provision of hazard incentives and life insurance was helpful in dousing the initial fear among healthcare workers and motivated them to come forward and provide service.
The second lesson learned is that adequate and quality laboratory capacity is critical in mounting a quick and effective response to any outbreak. The establishment of laboratory capacity for detection of viral hemorrhagic fevers in the country due to previous experiences of Lassa fever outbreaks came very handy for the diagnosis of the first EVD case. Delays in diagnosis could lead to delay in isolation of EVD cases and exacerbate the spread of the disease. Also noteworthy is the fact that the diagnostic primers and reagents for EVD diagnosis were available in the laboratory at the time and there were trained laboratory scientists to undertake the assays. This underscores the need for countries to establish capacities for adequate and qualitative diagnoses of pathogens of epidemic potential.
The third lesson learned is that the weak infection prevention and control (IPC) practices including the absence of triage in the health facilities predisposed many health workers (and some patients) to the risk of EVD infection, thus some of them were needlessly lost. Health care workers infection accounted for majority of the cases and deaths recorded in the Nigeria EVD outbreak [9]. Currently, majority of public and private health facilities do not place appropriate value on basic IPC practices such hand hygiene or triage of patients. Thus, nosocomial spread of infections is common. Basic IPC practices (standard precautions) need to be fully institutionalized, closely monitored and rewarded in all health facilities to ensure safety of health workers, patients and their families. Availability of basic hygienic supplies and personal protective equipment (PPE) in health facilities must also be ensured [10].
Adherence to minimum safety standard of care in private health facilities as well as public health facilities should be monitored regularly. Private health facilities often complement public health facilities and continue to provide services to the public during periods of frequent health workers’ strikes when public health facilities are closed. All private health facilities including for-profit ones should be empowered to meet recommended minimum IPC standards, and compliance rewarded. Equal attention should be paid to building IPC capacities for both private and public health workforce. Regulatory authorities in the ministry of health should be empowered to monitor compliance and implement sanctions on persistently non-compliant health facilities or workers.
We also learned that early community engagement is vital for effective response. The community must be seen by health workers as an interested ally and not just as a beneficiary, and must take ownership of its health including responding to epidemics [11]. Communities are better poised to mobilize themselves and identify resources that could be rapidly deployed at the onset of an outbreak to stop further propagation. For instance, working with the community, the health workers were able to overcome and resistance to establishment of ETCs in some communities due to the fear and anxiety of the spread of Ebola [12]. With little incentives, communities were also helpful in tracking down escapee contacts, notifying suspect cases, promoting hand-washing, social distancing and increasing population awareness of EVD preventive measures such as unsafe burial practices, and in many instances prevailed on community members to co-operate with healthcare workers in tracing and following up contacts of Ebola cases. Traditional and religious leaders, as community gatekeepers, played very important roles in this respect. Youth leaders, women leaders, local NGOs, community-based organizations (CBOs) and faith-based organizations (FBOs) were all engaged. In our experience, we found that the management of EVD outbreak and the care of affected people go beyond addressing their medical needs. Anthropological and psychosocial services were critical and beneficial in providing care to the affected individuals, communities and contacts [13-15].
Community engagement is therefore vital in every epidemic preparedness endeavor and community capacities should be reinforced to support prevention, early detection and response to disease outbreaks and other health emergencies.
Furthermore, collaborating with the organized private sector has the capacity to leverage enormous resources and support for emergency response. Nigeria is the fastest growing economy in Africa and has a robust private sector [16]. At the beginning of the outbreak when government bureaucratic processes delayed the release of funds, the organized private sector such as oil companies, telecommunication and some pharmaceutical companies supported the EEOC with mobile phones, airtime, vehicles, ambulances, infrared thermometers, and medicines. These were very helpful in keeping the operations on track before the availability of public funds.
The EVD outbreak revealed that epidemics could have major social and economic impacts, and therefore is a social problem [2]. Response efforts could sometimes require enormous resources which may not be swiftly provided by the public sector alone. Consequently, in limited resource settings, establishing collaborative mechanisms for co-funding and undertaking outbreak preparedness and response between government, the private sector and international Partners should be explored.
Besides the role of the community in identifying, tracking and following up contacts of Ebola cases, security operatives and telecommunication companies played a major role in providing valuable information that led to the finding of escapee and difficult contacts for follow-up. Security warrants were obtained and mobile telephone records of escape contacts were tracked and they were identified and followed up.
Additionally, the media played a crucial role also in stemming the Nigeria EVD outbreak. People desperately needed information on how to prevent and treat Ebola. However, at the onset of the outbreak, the reportage in electronic and print media fueled a lot of fear (as contracting EVD was considered a death sentence), stigmatization and misinformation among members of the public. In one instance of such misinformation that drinking of salt water prevents Ebola allegedly resulted in the death of at least two persons. Early and intensive dissemination of key messages to the public on Ebola immediately the outbreak was declared, using a wide range of media would have prevented such a situation. However, the EEOC immediately moved to engage and conduct orientation meetings with key media organizations in the country, and this positively reversed the situation. Subsequently, publicity was intensified through the media, providing continuous access to information about the disease, including its mode of spread, preventive measures and actions being undertaken to stop the disease. For instance, the Minister of Health’s press conferences on the progress was widely disseminated through the media. This helped to allay further fear and stigmatization. Additionally, the social media proved to be a veritable tool for information dissemination to the public on the disease e.g. through facebook and tweeter, and provided a platform for providing feedback on questions and comments from the public, addressing misinformation and monitoring community alerts [17]. This approach needs to be further developed and promoted as part of future epidemic preparedness and response efforts.
We learned that strong political will and leadership at the highest level promotes effective coordination of outbreak response and mobilization of adequate resources. The President and the Governors wield enormous power and influence in the country and they put their authority firmly behind the response. The Governors of Lagos and Rivers States particularly provided exemplary leadership, financial resources and personally monitored the response efforts closely. This motivated the healthcare workers in the frontline to make a difference recognizing that they had the support of the leadership at the highest level.
Finally, we learned that that public health response capacity at the points of entry must be fully developed as a matter of priority to prevent the international spread of diseases in this age of globalization. As disease knows no boundary, the need to strengthen public health measures at the points of entry (ground crossings, seaports and airports) as required by the International Health Regulations (2005) becomes imperative. Cross-border surveillance activities including community awareness and engagement, and improved referral system and capacities would reinforce early detection and rapid control of EVD. This approach has been shown to be critical to building and sustaining effective public health response capacities at local, national and global levels [8,18-20].
Limitations and constraints
The Ebola outbreak in Nigeria was rather short-lived, lasting only three months; while this may be attributed to the effective response and rapid containment, it provided a limited opportunity to consider a large number of cases and contacts and the associated features. Secondly, the identification of contacts was dependent on the information on exposure that was provided by individuals and health workers who came in contact with an Ebola case, but sometimes the information provided may not be accurate. However, the use of experienced Field Epidemiologists who were also trained on interviewing techniques minimized this occurrence.
Conclusion
The EVD outbreak in Nigeria was rapidly contained with major lessons learned that could be leveraged to improve epidemic preparedness and future response efforts. While Nigeria was able to successfully stop the outbreak by leveraging existing local capacity, critical improvements are still needed to strengthen early warning systems and rapid response capabilities in preparation for any future re-introduction of EVD to the country. Although no new Ebola cases have been e reported in Nigeria since October 2014, community- based and health facility surveillance, public health measures at Points of Entry have been strengthened and a National EOC set up at the NCDC. Rapid response teams have been inaugurated at the subnational levels (States). Post Ebola containment plan has been developed and the experience acquired from the EVD control activities has been used to fight other new outbreaks such as Lassa fever. Nigeria now needs to focus on rapid implementation of the IHR (2005) core capacities requirement [21,22], which are critical to improving future epidemic preparedness, mitigating potential re-introduction of EVD and assurance of population health security.
Authors' contributions
AN, EM contributed to the conception, design and preparation of the first draft. AN, EM, FS, PN, RGV participated in data collection, analysis and interpretation and preparation of the manuscript. All authors read and approved the final manuscript.
Acknowledgments
We acknowledge the former Honorable Minister of Health, Prof. CO Onyebuchi Chukwu and the Lagos State Commissioner for Health, Dr. Jide Idris, The River State Commissioner of Health, Dr. Sampson Parker, Dr. Olukayode Oguntimehin, Dr. Ismail A Abdus-salam, Dr. Nnanna Onyekwere, Dr. Oni Idigbe, Prof. Sunday Omilabu, Mrs. Sara Nyanti, Mr. Charles Nzuki, all EEOC strategic group members, all the responsible team leads and members at the Lagos and Portharcourt EEOCs.
17522
References
- Chan M (2014) Ebola virus disease in West Africa-no early end to the outbreak.N Engl J Med 371: 1183-1185.
- Shuaib F, Gunnala R, Musa EO, Mahoney FJ, Oguntimehin O, et al. (2014)Ebola virus disease outbreak-Nigeria, July-September 2014.MMWR Morb Mortal Wkly Rep 63: 867-872.
- WHO (2014) Case definition recommendations for Ebola or marburgvirus diseases.
- Tom-Aba D, Olaleye A, Olayinka AT, Nguku P, Waziri N, et al (2015) Innovative technological approach to Ebolavirus disease outbreak response in Nigeria using the open data kit and form hub technology. PloS one 26: e0131000.
- Moore M, Dausey DJ (2015) Local cross-border disease surveillance and control: experiences from the mekongbasin. BMC 8: 90.
- Okwor TJ, Tobin-West C, Oduyebo O, Anayochukwu-Ugwu N, Adebola O, et al (2015) Identifying infection prevention and control gaps in healthcare facilities operating in Rivers state during the EVD outbreak in Nigeria 2014. AntimicrobResisInfecCont 4: 11.
- Marais F, Minkler M, Gibson N, Mwau B, Mehtar S, et al (2015) A community-engaged infection prevention and control approach to Ebola. Health promotint 12: dav003.
- Maduka O, Maleghemi S, Komakech W, Nwaduito I, Green P, et al. (2016) Effective risk communication and contact tracing for Ebola virus disease prevention and control-Experiences from Port Harcourt, Nigeria.Public Health 135: 140-143.
- Ogoina D (2016) Behavioural and emotional responses to the 2014 Ebola outbreak in Nigeria: a narrative review.Int Health 8: 5-12.
- Abramowitz SA, Bardosh KL, Leach M, Hewlett B, Nichter M, et al. (2015) Social science intelligence in the global Ebola response.Lancet 385: 330.
- Umeora OU, Emma-Echiegu NB, Umeora MC, Ajayi N (2014) Ebola viral disease in Nigeria: The panic and cultural threat. Afr J Med Heal Sci 13: 1.
- Oshikoya TW (2008) Nigeria in the global economy. Business Economics 43: 31-43.
- Adebimpe WO, Adeyemi DH, Faremi A, Ojo JO (2015) The relevance of the social networking media in Ebola virus disease prevention and control in Southwestern Nigeria. Pan Afr Med J 22: 7.
- Briand S, Bertherat E, Cox P, Formenty P, Kieny MP, et al. (2014) The international Ebola emergency.N Engl J Med 371: 1180-1183.
- WHO (2014) Ebola virus disease in west africa-the first 9 months of the epidemic and forward projections.N Engl J Med 371: 1481-1495.
- Green A (2014) Ebola emergency meeting establishes new control centre.Lancet 384: 118.
- Gostin LO (2014) Ebola: towards an International Health Systems Fund.Lancet 384: e49-51.
- WHO (2012) Summary of 201 states parties report on IHR core capacity implementation.