Nagaraja HR*, Deshmukh A, Shivanna Y, Thungappa KS and Rohit S
Cornea and Refractive Services, Narayana Nethralaya, Bangalore, India
*Corresponding Author:
Nagaraj H
Cornea and Refractive Services, Narayana
Nethralaya, West of Chord Road, Rajaji
Nagar, 1st‘R’ Block, Bangalore, Karnataka,
India 560010.
Tel: 9849562314
E-mail: harshdr@gmail.com
Received date: September 03, 2017; Accepted date: September 06, 2017; Published date: September 10, 2017
Citation: Nagaraja HR, Deshmukh A, Shivanna Y, Thungappa KS, Rohit S (2017) Ocular Parasitosis: A Report of Two Contrasting Cases. Arch Clin Microbiol. Vol. 8 No. 5:62 doi: 10.4172/1989-8436.100062
Purpose: We report two cases of ocular subconjunctival parasitosis presenting
with similar complaints of persistent pain, redness and watering in the affected eye.
Methods: Both cases were diagnosed based on slit lamp examination and anterior
segment OCT and the parasite was found to be motile on exposure to external
light.
Results: In the first case the subconjunctival parasite was found under the upper lid
and was surgically removed on the same day while in the second case the parasite
was found in the temporal interpalpebral area and possibly migrated posterior to
the globe due to the delay in surgical removal and constant light stimulus.
Conclusion: Prompt immediate surgical removal of the parasite and patching of
the eye in cases where the parasite is in light exposed areas is of importance in
managing these cases.
Keywords
Parasites; Subconjunctival; Diofilariasis
Introduction
Ophthalmic parasitosis is common in the developing countries where parasitic infections are frequent owing to the poor sanitary conditions and environmental factors [1]. The common parasites responsible for ocular infection include protozoa like Acanthamoeba spp., Leishmania spp., helminths that include round worms like Angiostrongylus spp., Loa loa, Dirofilaria spp., and flat worms like Taenia solium and Schistosoma spp [1]. Loa loa, Onchocerca and Dirofilaria are some of the parasites that are found subconjunctivally [1,2]. Ocular Dirofilariasis has been reported in India from Kerala, Karnataka and Gujarat [2-4]. While symptomatology and serology are not reliable for diagnosis, surgical removal and histopathological diagnosis is the best way to identify the parasite [5]. Chemotherapy has been reported to be ineffective in management of such cases [5].
We report two cases of subconjunctival parasitosis that presented to us with similar clinical features and presentation but with different treatment outcomes. One of the parasites was successfully removed while the other migrated probably to the posterior aspect of the globe making it inaccessible to surgical removal. With this report, we would like to highlight the importance of prompt removal of ocular parasites and also the further management of such cases.
Case Reports
Case 1
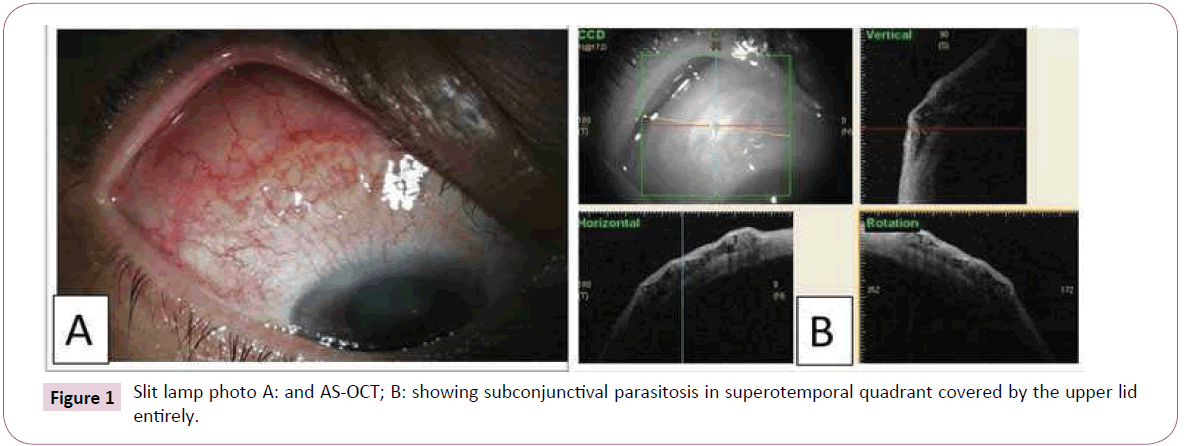
Fifty-five year old male patient presented to our cornea clinic with chronic redness and pain in the right eye since 6 months. He was being treated elsewhere for chronic conjunctivitis with no response to topical antibiotics and topical steroids providing intermittent relief from symptoms. On slit lamp examination, right eye showed diffuse superficial conjunctival congestion, papillae were noticed in the upper tarsal conjunctiva and a subconjunctival whitish mass was noticed in the subconjunctival superotemporal quadrant measuring about 4 mm in diameter which was found to be motile when exposed to slit lamp light source (Figure 1A). A diagnosis of subconjunctival helminthiasis was made and anterior segment optical coherence tomography (Casia SS-1000, Tomey, Nagoya, Japan) of the affected area showed coiled subconjunctival parasite (Figure 1B). Fundus examination was normal. Surgical removal of the subconjunctival parasite was done under topical anaesthesia on the same day and was sent for identification. The species was later identified as Dirofilaria repens. Patient was advised topical antibiotic steroids in tapering doses and was referred to a physician for systemic anti-helminthic treatment and the patient responded to treatment well with resolution of symptoms by 2 weeks follow-up.
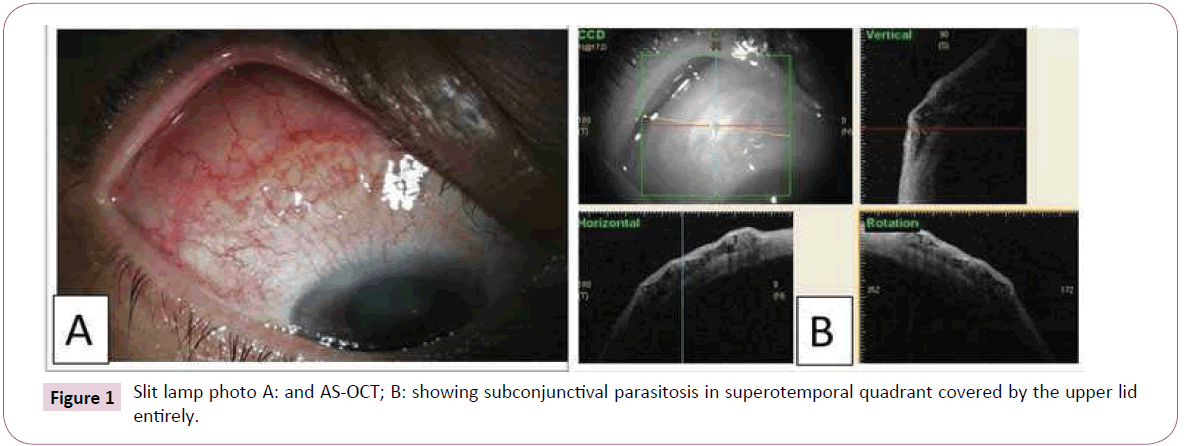
Figure 1: Slit lamp photo A: and AS-OCT; B: showing subconjunctival parasitosis in superotemporal quadrant covered by the upper lid entirely.
Case 2
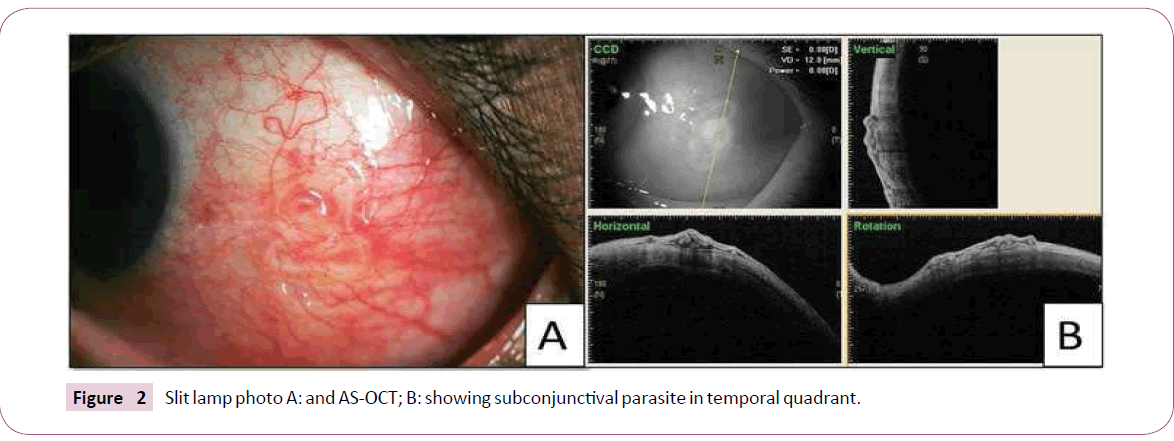
Fifty-seven-year-old female patient presented with redness and irritation in the left eye since 1 week. Slit lamp evaluation showed localized temporal conjunctival congestion with a motile whitish mass in the temporal interpalpebral subconjunctival space (Figure 2A). Fundus examination was normal. Anterior segment OCT confirmed the presence of parasite in the subconjunctival space (Figure 2B). Patient was not willing for the surgical removal Figure 1 Slit lamp photo A: and AS-OCT; B: showing subconjunctival parasitosis in superotemporal quadrant covered by the upper lid on the same day and hence was advised to undergo surgery on the following day. Slit lamp examination on the next day revealed that though the localized conjunctival congestion persisted the subconjunctival parasite was not found in the area noticed earlier. A thorough examination of the ocular surface under topical anaesthesia was performed to identify if the parasite had migrated to any other accessible areas followed by a fundus examination. In view of the parasite not being visible in the anterior ocular surface, it was concluded that it had migrated into the posterior part of the globe. Since the patient refused to get MRI done to localize the parasite, she was advised topical antibiotic steroids tapered over 3 weeks with close follow-up. Patient has been under follow-up for 6 months with no recurrence of congestion or other ocular symptoms.
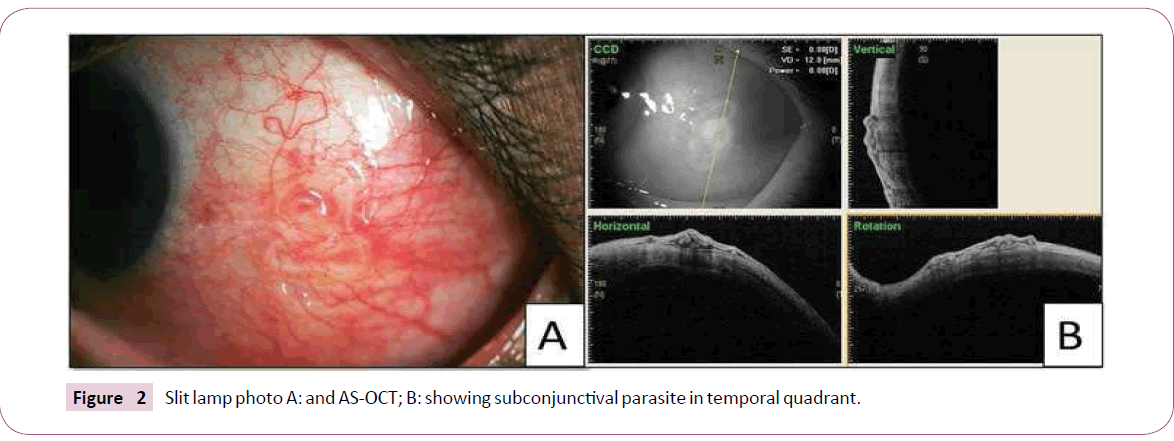
Figure 2: Slit lamp photo A: and AS-OCT; B: showing subconjunctival parasite in temporal quadrant.
Discussion
Ocular helminthiasis has been commonly reported from all parts of the world [6]. The identification of the parasite requires assistance of a parasitologist to appreciate the microscopic features and identify the causative worm. Surgical excision of the parasite is diagnostic as well as therapeutic. The entire parasite should be removed to prevent allergic reactions to the remnants of the parasite [7]. In our first case, we were able to identify the parasite as D. Repens. It is one of the commonly reported helminths infesting the human eye and in most of the cases it is subconjunctival [7].
In the other case, we were unable to surgically extract the parasite. It has been shown before that helminthic worms show faster movements on exposure to light stimulus [8]. The worms tend to migrate posteriorly or penetrate the anterior chamber in an attempt to move away from the light [8]. We observed a similar behavior in our cases with both live helminths showing motility on exposure to slit lamp and indirect ophthalmoscope light source. In the first case, when the parasite was found under the upper lid, it was covered and protected from the stimulus of light and this possibly made the parasite to remain stationary in the same location. Moreover the parasite was removed on the same day giving it less time to migrate to a different location. In the second case however, the worm was in the interpalpebral area and exposed to the bright external light which could have made the parasite to migrate and also, the time since diagnosis and patient being posted for surgical removal was more than 24 hours providing sufficient time for the parasite to migrate. Tse BC et al. reported a technique of forming a pharamacological barrier using 1% lidocaine with epinephrine in the forniceal conjunctiva to prevent the motility of the worms to inaccessible areas [9]. Patching the eye in order to prevent the worm from getting exposed to light is one of the methods by which the motility of the worm can be reduced, especially when the worm is found in light exposed areas [10].
To conclude, patients presenting with chronic conjunctivitis not responding to regular treatment need to be evaluated thoroughly to rule out ocular helminths followed by immediate surgical removal. Patching of the eye if the helminth is found in light exposed areas is of importance in managing these cases. To the best of our knowledge this is the first report highlighting the possible cause of subconjunctival parasite that could not be surgically removed.
20620
References
- Nimir AR, Saliem A, Ibrahim IA. Ophthalmic parasitosis: a review article.
- Sabu L, Devada K, Subramanian H. Dirofilariosis in dogs and humans in Kerala. Indian J Med Res. 2005 May;121(5):691–3.
- Nadgir S, Tallur SS, Mangoli V. Subconjunctival dirofilariasis in India. Southeast Asian J Trop Med Public Health. 2001 Jun;32(2):244–6.
- Patel R, Singh S, Bhavsar S. A rare case of subconjunctival dirofilariasis by Dirofilaria repens in rural Gujarat. Indian J Ophthalmol. 2014 May;62(5):649–51.
- Bhat KS, Kotigadde S, Vishwanatha Bhat K. Subconjunctival dirofilariasis: Case studies with review of literature. Trop Parasitol. 2014 Jul;4(2):119–21.
- Fuentes I, Cascales A, Ros JM. Human subcutaneous dirofilariasis caused by Dirofilaria repens in Ibiza, Spain. Am J Trop Med Hyg. 1994 Oct;51(4):401–4.
- Kalogeropoulos CD, Stefaniotou MI, Gorgoli KE. Ocular dirofilariasis: a case series of 8 patients. Middle East Afr J Ophthalmol. 2014 Dec;21(4):312–6.
- Jaksic V, Mitic N, Pavlovic I. Discrete eyelid swelling caused by live subconjunctival Dirofilaria repens. Open Medicine. 2011; 6(2):177-180.
- Tse BC, Siatkowski R, Tse DT. A technique for capturing migratory periocular worms: a case series and review of literature. Ophthal Plast Reconstr Surg. 2010 Oct;26(5):323–6.