Key words
Perceived barrier, cervical cancer, screening, Botswana.
Introduction
Cancer of the cervix is a major burden on women’s health worldwide. It is the second most common cause of cancerrelated death among women globally as well as in Botswana [1,2]. It is estimated that 493,000 new cases and 274,000 deaths occur every year due to this prevenTable disease [2]. Cervical cancer is a major cause of mortality and morbidity among women in less developed countries including Botswana. A study found that cervical cancer is one of the most prevenTable human cancers, because of its slow progression, cytological identifiable precursors, and effective treatments [3]. Therefore, Papanicolaou (Pap) cervical cytology screening has helped to reduce cervical cancer rates dramatically through early detection of premalignant lesions [4,5].
In Botswana, the crude incidence rate of cervical cancer per 100,000 women is 19.8, and the annual number of new cervical cancer cases is 156 per 100,000 women. It is the second highest rate of cancer in Botswana after breast cancer (crude incidence rate of 21.4 per 100,000 women) [2]. Despite being the second highest occurring type of cancer in Botswana, the crude mortality rate from cervical cancer remains the highest when compared to other types of cancers with a crude mortality rate of 15.9 per 100,000 women, followed by the crude mortality rate from breast cancer of 15.7 per 100,000 women [2]. Furthermore, despite effective preventive and screening programs that are available in the country’s health care system for free cervical cancer screening, the annual number of deaths from cervical cancer in Botswana has remained high at 126 per 100,000 women [2].
Worldwide, high incidence of cervical cancer is associated with lack of cervical cancer screening or lack of regular cervical cancer screening and follow-ups of abnormalities. A recent study from Botswana reported that lack of cervical cancer screening is noted for different reasons like lack of knowledge, access, financial constraints, etc [6]. These perceived barriers to cervical cancer are major factors that determine a woman’s likelihood to participate cervical cancer screening although attitudes of health providers, availability and cost are other important determinants [7].
Many studies have identified fear of report of having a cancer, embarrassment, pain, financial constraints, attitudes of health workers, lack of convenient clinic times and lack of female screeners, etc as the major barriers to cervical cancer screening. A study from Jamaica reported that 42% of the study population feared that their health provider would find cervical cancer if they do Pap smear test, 46% reported that their major concern was pain associated with the procedure and 24% reported that not receiving the result back was the main reason why they were not interested in doing cervical cancer screening [8]. Another study compared women who had a Pap smear and those who never had a Pap smear test done. The findings showed that 82.4% of those who had a Pap smear test felt very sure or completely sure that they could discuss issues regarding Pap smear test with their healthcare provider. However, 78% of those who had never been screened felt that they could get a Pap test done even if they were worried that it will be painful (74% vs. 57%), and that they could get a Pap test done even if they were worried that it would be embarrassing (49.6% vs. 22%) [9].
A study on Cervical cancer and Pap smear screening in Botswana found that only 40.0% of study participants had ever had Pap smear tests and the major barriers to obtaining Pap smear tests included inadequate knowledge about Pap smear screening, provider attitudes, and limited access to physicians. Reasons for limited knowledge included cultural norms of secrecy, providers not informing the public, and policy makers’ limited attention to cervical cancer. Providers’ major barriers to providing Pap smear tests was found to include clients’ inadequate knowledge of Pap smear screening, providers’ inability to see the importance of Pap smear tests, and workload and staff shortages) [6]. If these barriers of doing cervical cancer screening are addressed, the uptake of cervical cancer screening can improve given that these barriers deter most women from doing cervical cancer screenings especially misconceptions and cultural beliefs. Therefore, determining ways of overcoming these problems is a pre-requisite for improving the uptake in cervical cancer screening program. Thus, the objectives of this study were to describe the women’s perceived barrier to cervical cancer and the association between socio-demographic characteristics and perceived barrier to cervical cancer.
Methods
The study was a cross sectional study. The study was conducted in Mahalapye District Hospital which is a 250 bed hospital. The hospital offers outpatients and inpatients services to the Mahalapye sub-district community. It is one of the 6 district hospitals managed by the Ministry of Health in Botswana. It serves as a referral facility to 44 health facilities in the subdistrict comprising one primary hospital, 15 clinics, 28 health post and mobile clinics [10]. Mahalapye sub-district has a total population of 109,811 people, comprising 53,318 males and 56,493 females [11]. The hospital is located in the central part of Botswana about 200km from Gaborone, along the A1 road that runs across the country from North to South.
Mahalapye district Hospital was chosen because it runs both outpatients and inpatients services to both males and females. On average, approximately 180 to 240 patients are seen in outpatients daily, approximately 80 patients in Infectious Disease Control Centre (IDCC), and the hospital has an average bed occupancy rate of 102 patients for inpatients cases [12]. It has a good information management system in place that enables the capturing and retrieval of relevant information with some degree of accuracy and reliability.
The target population for the study comprised all women served by Mahalapye District Hospital who were above the age of 18 years. From the census report, Mahalapye sub-district has a total population of 109,811 people, comprising 53,318 males and 56,493 females [11]. The target population of the study included 37,662 of the 56,493 female population served by Mahalapye District Hospital. Since outpatients department forms the entry point of all patients to the hospital, the sampled populations were interviewed mainly at the outpatients department.
A minimum sample size was calculated using a standard formula for known population size for a cross sectional study. The formula is given below [13]:

Where n = sample size of adjusted population, N = population size and e = accepted level of error taking alpha as 0.05.
The estimated number of women seen in Mahalapye District Hospital monthly was estimated from Hospital records to be about 800. Substituting this figure into the formula below, a sample size of 267 was obtained.

n = 267.
However, since convenience sampling was used to interview the participants, the sample size was increased to 300 participants.
Convenience sampling was performed by approaching all eligible women who presented to outpatients department during the month of sample collection for interview (June, 2009). The purpose of the research and procedure was explained to them and those who consented to participate were interviewed. The researcher and the assistant ensured that no woman was interviewed more than once by asking if they had previously been interviewed.
All adult women age above the age of 21 years attending Mahalapye District Hospital who consented to participate were included in the study. We excluded all women attending Mahalapye District Hospital who were below the age of 21 years since they cannot give consent to participate according to Botswana law as well as women above 21 years who refused to consent for participate in the study.
A structured self-administered questionnaire was used to collect data for those who could read and write. For those who could not read or write, the research assistant administered the questionnaire. The perceived barrier of cervical cancer was assessed using 5 point LIkert-type scale questions in the questionnaire. Each question was scored ranging from strongly agree (5) to strongly disagree (1). The scale was revised for negatively worded questions. The total scores for perceived barrier subscale had a possible range from 12 to 60. The categorical dependent variable rated yes or no whether a woman had ever had cervical cancer screening. If the answer was yes, she was asked if the cervical cancer screening was done within the past 3 years.
The questionnaire was translated to the local Setswana language and was pre-tested using 30 patients in another health facility outside Mahalapye by the researcher to identify gaps and modify the questionnaire appropriately. The questionnaire was then pilot tested and modified to ensure it answered the research questions. Piloting of the questionnaire was done in Palapye Primary Hospital. Palapye is another town about 70 kilometers from Mahalapye.
The questionnaire was administered by the researcher and a trained assistant who speaks the local language to exclude personal prejudice. The questionnaire was also translated to the local Setswana language and administered to participants to eliminate bias due to non-response because the participant could not read or write.
Ethical Considerations
Ethical clearance for the study was obtained from Medunsa Campus Research and Ethics Committee (MCREC) of the University of Limpopo, South Africa. Permission to conduct the study was obtained from the National Health Research Unit (HRU) of the Ministry of Health, Botswana, and the Management of Mahalapye District Hospital before commencement of the study. Informed consent of participants was obtained. Confidentiality of participants was maintained at all times. To further maintain confidentiality, no form of identifiers was in the questionnaires. Participation was voluntary, and participants were informed that they could withdraw from the study at any stage of the interview if they so desired without any penalty.
Data analysis
Data were entered into a Microsoft Excel 2003 spreadsheet and imported to SPSS 17.0 for Microsoft Window version for analysis. The analysis results of participants’ demographics and outcome variables were summarized using descriptive summary measures, expressed as mean (SD) for continuous variables and percent for categorical variables. The chi-square test was used to find an association between categorical variables. Binary logistical regression was carried out to find the significant predictor for doing a Pap smear test. All statistical tests were performed using two-sided tests at the 0.05 level of significance. For all regression models, the results were expressed as effect (or odds ratios for binary outcomes), corresponding two-sided 95% confidence intervals and associated p-values.
P-values were reported to three decimal places with values less than 0.001 reported as <0.001. A high score was considered 75% or more and a low score was considered as less than 75%.
Results
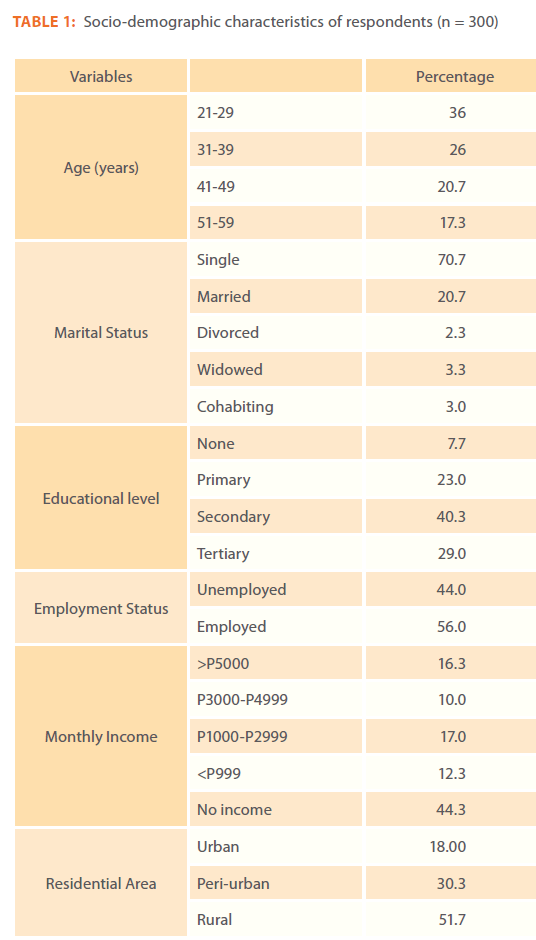
Table 1 summarized socio-demographic characteristics of the study participants. A total of 300 participants were recruited with mean of 36.9 years (SD = 11.04). More than one third of the women were between the age of 21 and 29 years (36%). Majority of them were (71%) were single, and 21% were married. Only 8% had no form of education and 69% had attained at least secondary education. Almost all participants were of black African race (98%). Less than half (44%) were unemployed. The residential status was almost equally distributed with rural (51%) and urban plus peri-urban (49%).
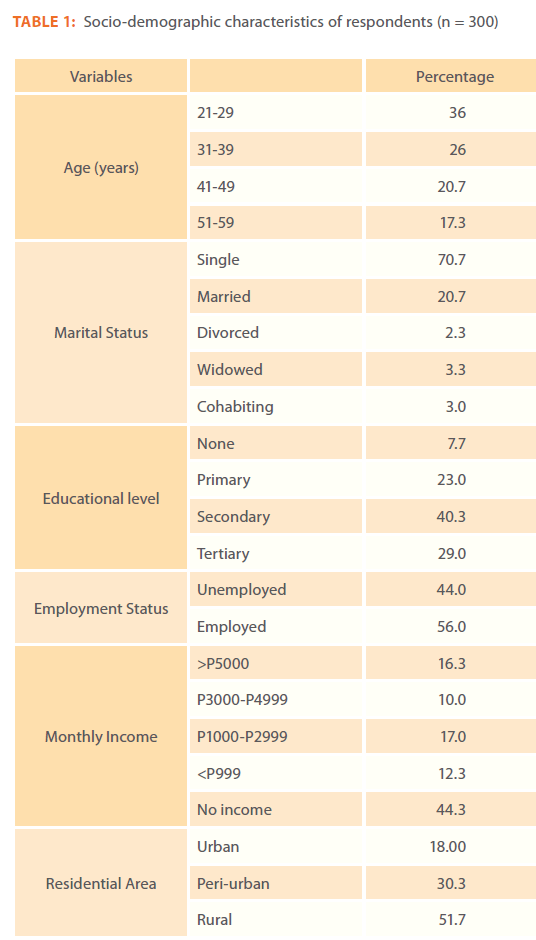
Table 1: Socio-demographic characteristics of respondents (n = 300)
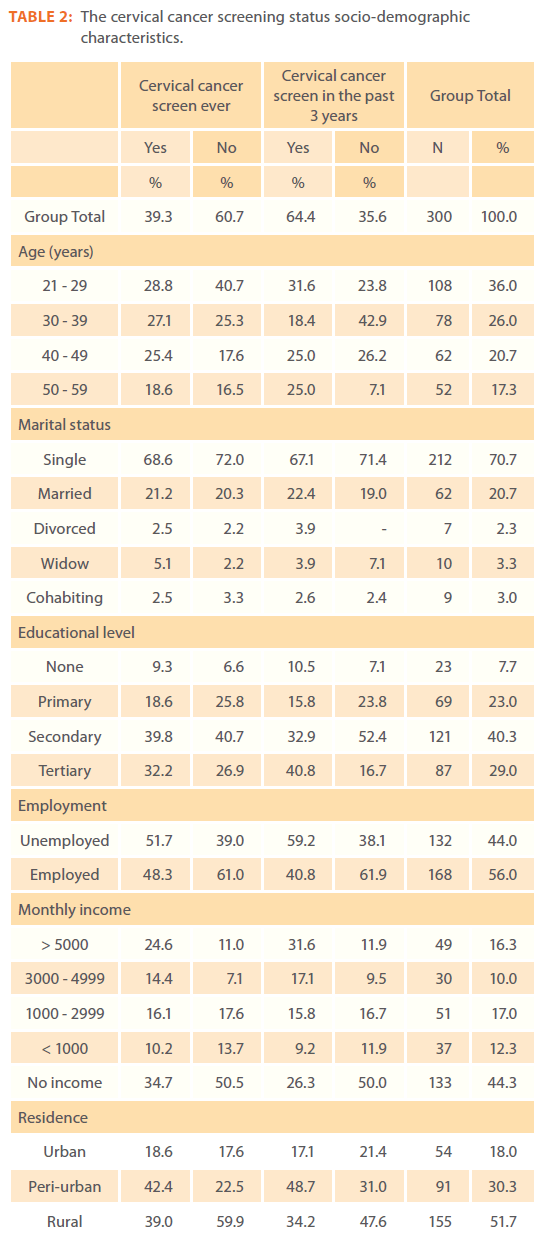
Table 2 showed the distribution of cervical cancer screening status of the participants. Most of those that had ever screened for cervical cancer (64%) actually did the screening within the past 3 years. Most (72%) of the ever screened had attained at least secondary school education. Regarding age, the highest testing rates were among the age group 40 – 49yrs.
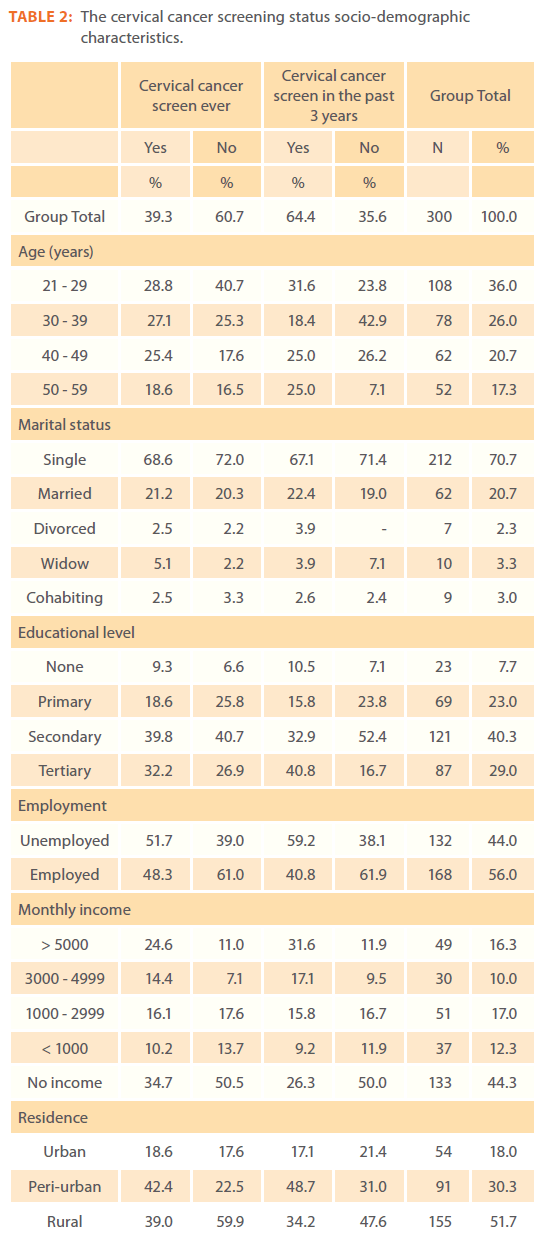
Table 2: The cervical cancer screening status socio-demographic characteristics.
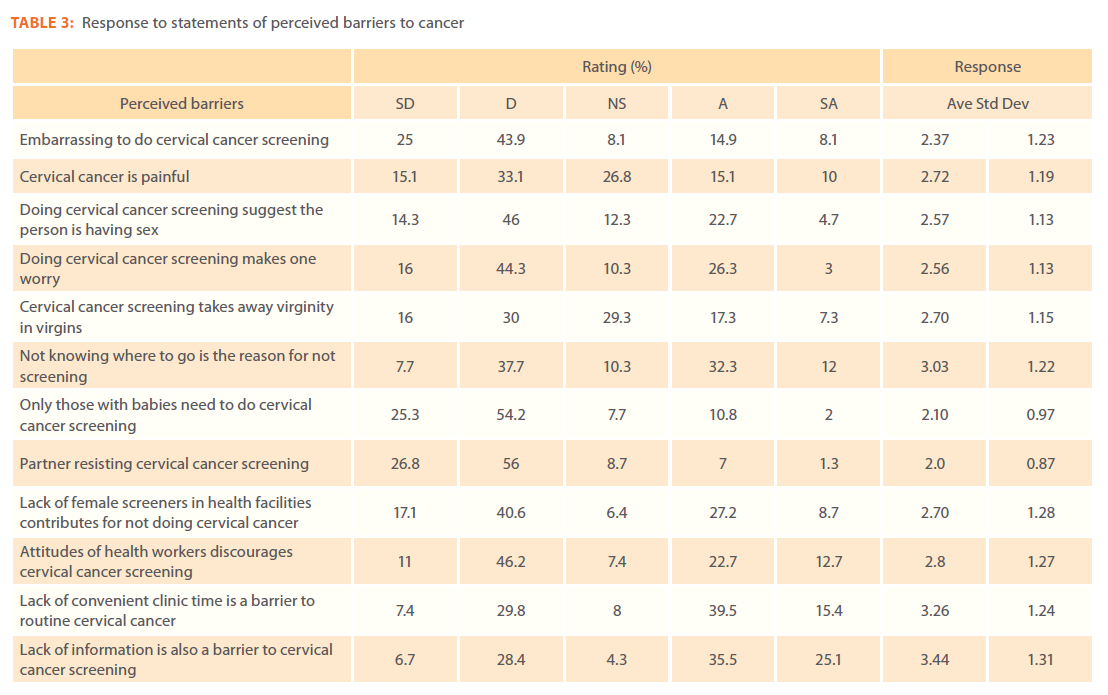
Table 3 summarized the responses to perceived barriers to cervical cancer screening. In general, most of the ratings were below 3.0. That is, most participants disagreed or strongly disagreed about the statements on perceived barriers. This showed that most participants believed that: cervical cancer screening was not embarrassing (68%) and doing cervical cancer screening did not suggest someone was having sex (48%).
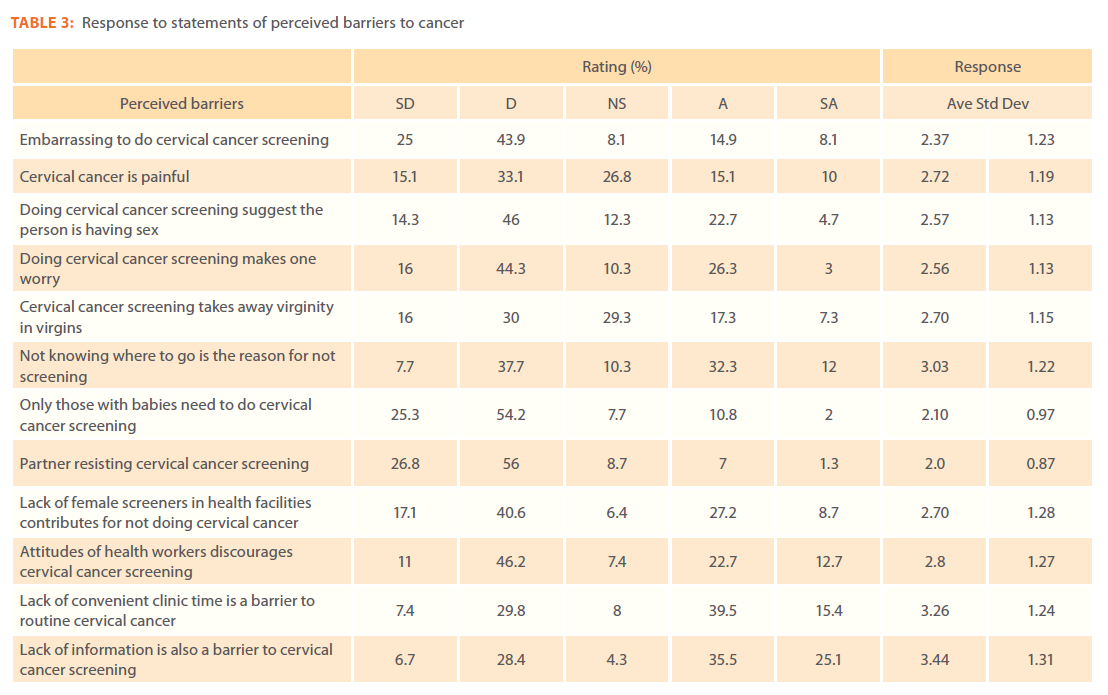
Table 3: Response to statements of perceived barriers to cancer
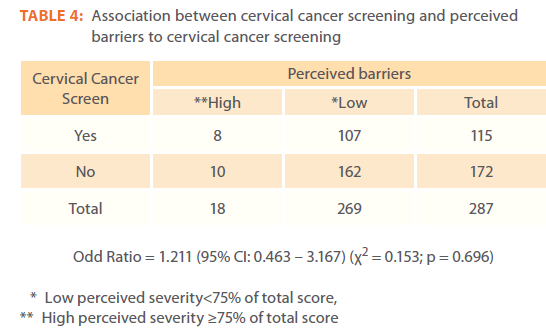
When the ever screened and never screened were compared (Table 4), 44.4% of the ever screened had high perceived barriers and 60% of the never screened has low perceived barriers. There were no significant association between perceived barriers for cervical cancer screening and screening for cervical cancer (c2 = 0.153; p = 0.696).
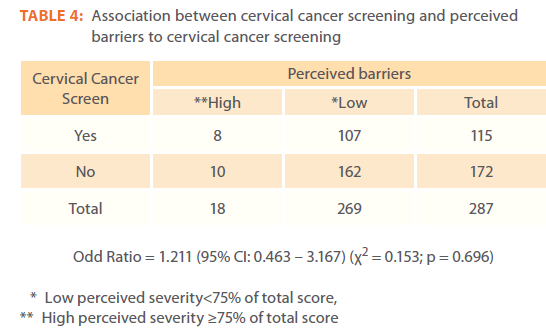
Table 4: Association between cervical cancer screening and perceived barriers to cervical cancer screening
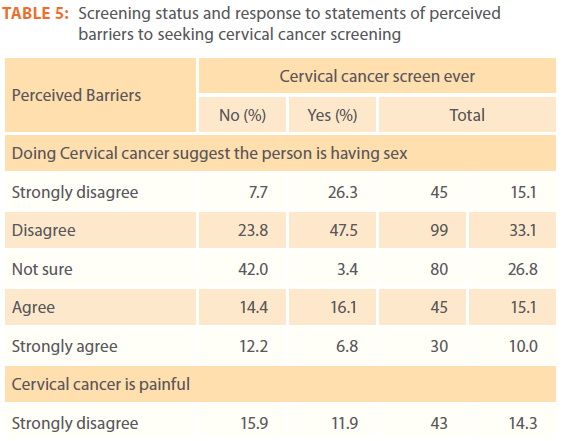
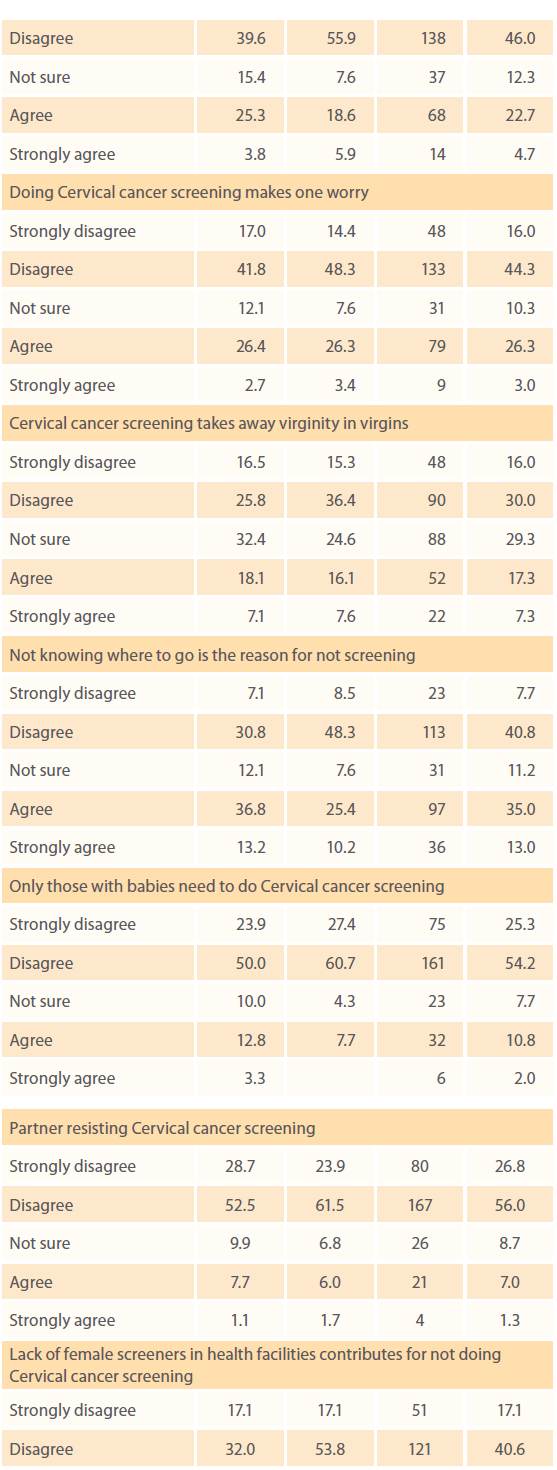
When the screened respondents were compared with the never screened (Table 5), 74% either strongly disagreed or disagreed that doing cervical cancer screening suggest a person is having sex as opposed to 26% of never screened who responded not sure. About 55.5% of the never screened either strongly disagreed or disagreed that cervical cancer screening is painful while 67.8% of those that have screened either strongly disagreed or disagreed that cervical cancer is painful. Majority of both the screened and the never screened either strongly disagreed or disagreed that only women who had babies should participate cervical cancer screening, their partners will be resistant to their participating in cervical cancer screening. The never screened either strongly agree or agree that lack of information was a barrier to cervical cancer screening (66.3%) as opposed to 51.7% of those that had screened.
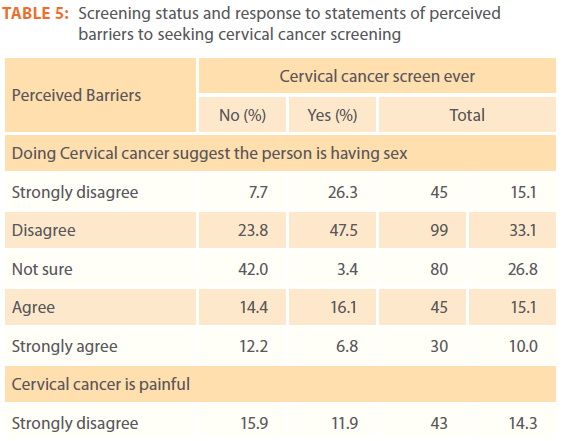
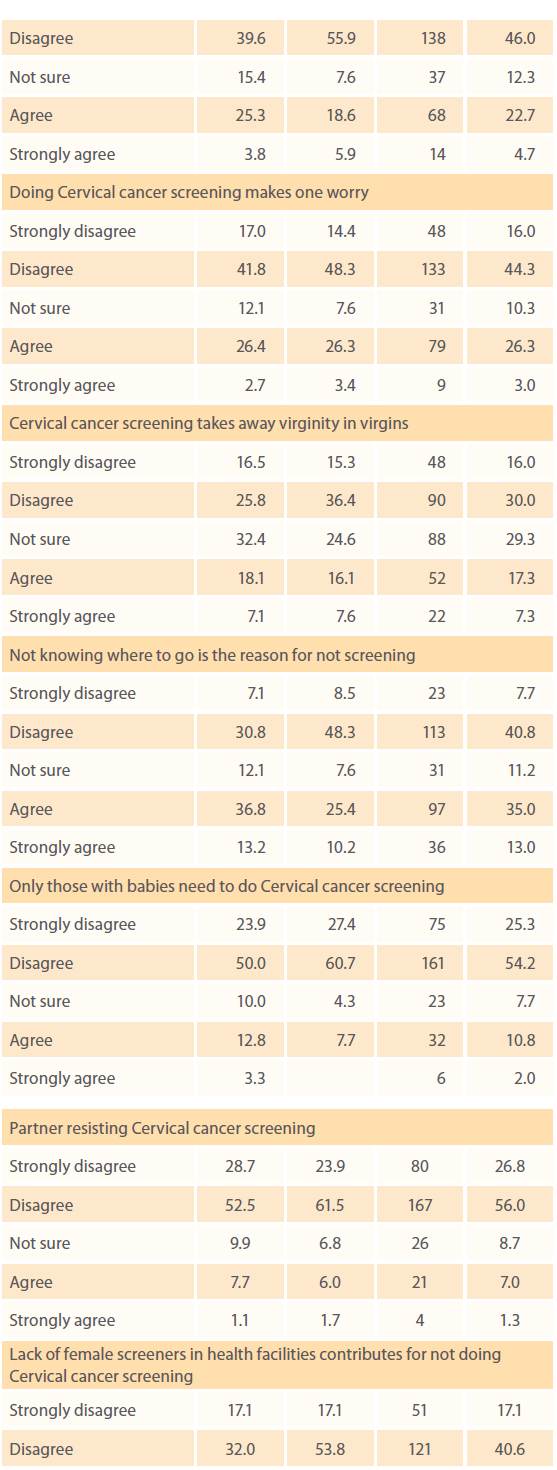
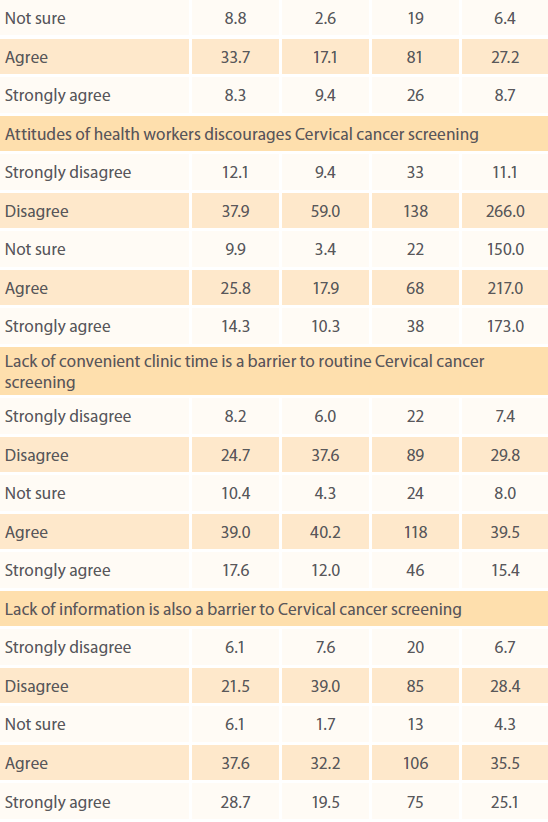
Table 5: Screening status and response to statements of perceived barriers to seeking cervical cancer screening
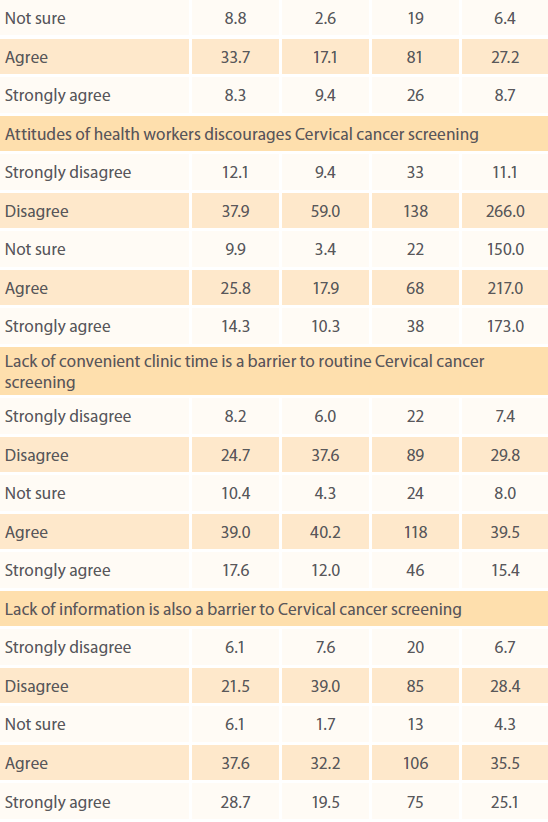
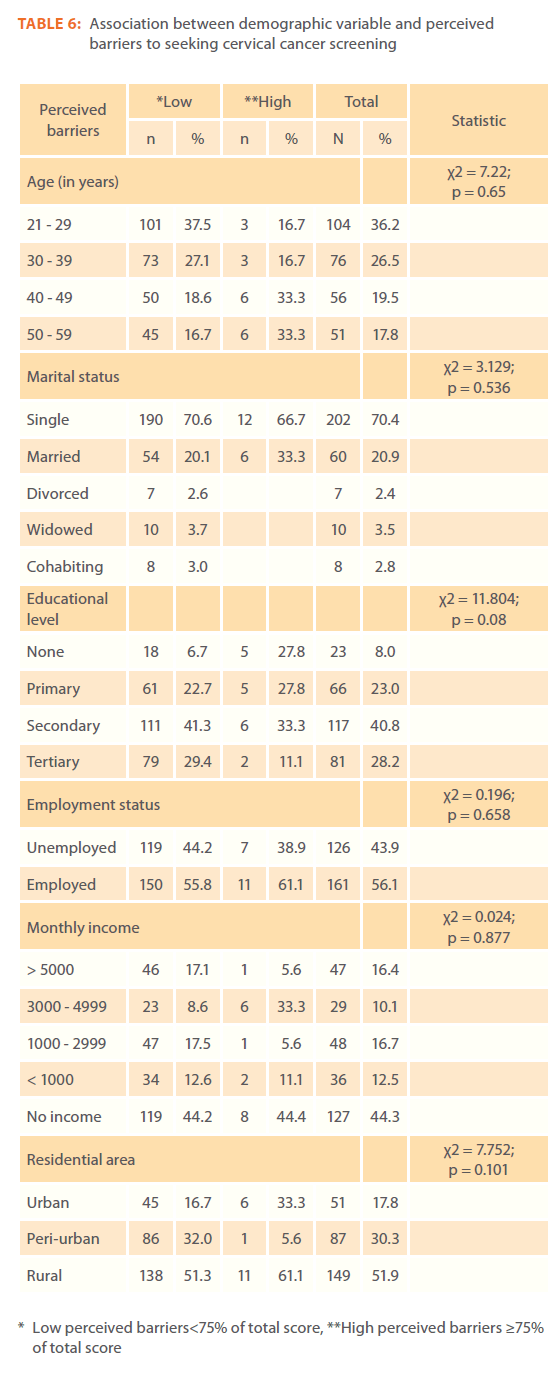
Table 6 showed that there was no significant association between socio-demographic factors and perceived barriers to seeking cervical cancer screening (all p-values > 0.05).
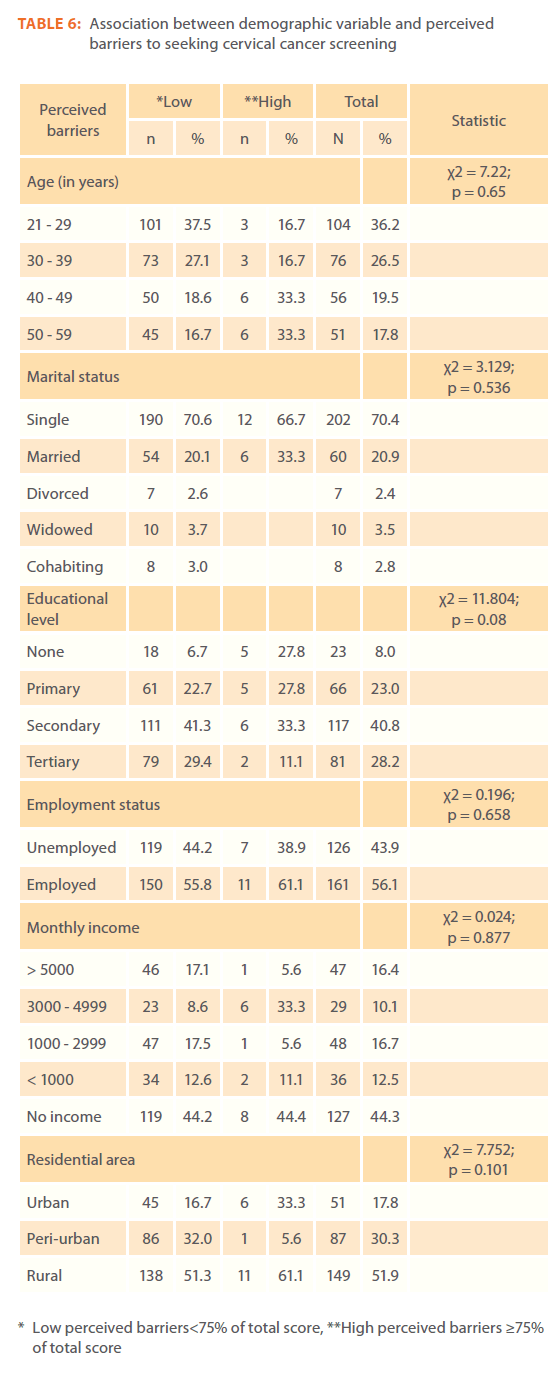
Table 6: Association between demographic variable and perceived barriers to seeking cervical cancer screening
Independent-sample t-test was used to examine the mean difference in perceived barriers between women who had ever screened for cervical cancer and women who never screened. Women who had never screened for cervical cancer had significantly higher mean value of perceived barriers compare to those screened for cervical cancer (μ = 30.6 vs 33.4, P = 0.001, Data not shown).
Bivariate logistic regression was used to examine if perceived barriers predicted screening for cervical cancer. Percieved barriers were not a significant predictor for doing cervical cancer screening (OR = 1.212, p = 0.72, Data not shown).
Discussion
The cervical cancer screening status of research participants was found to be 39%, of which 64% was done within the past 3 years. This cervical cancer screening rate is far too low and do not reach the Ministry of Health’s goal of cervical cancer screening of at least 75% or more. A similar study in Botswana found that only 40.0% of study participants had ever had a Pap smear test [6]. This finding of low participation of cervical cancer screening and low follow-up of screening is consistent with other studies done in less developed countries which reported an average participation rate of 23% and follow up rates of 46% within 3 years [14,15]. Among others, reasons for low participation included at-risk women not perceiving themselves as been susceptible to cervical cancer provided they had no symptoms, lack of information about the benefits of cervical cancer screening and misconceptions such as thinking the screening is painful, it takes away virginity, etc. Although most participants perceived cervical cancer as serious, the assumption was that there was no treatment of cervical cancer made the women uninterested to participating in cervical cancer screening.
Cervical cancer screening status
This study also found that women who had previously screened for cervical cancer had a higher perceived susceptibility to cervical cancer than those who had never screened for cervical cancer. When perceived susceptibility to cervical cancer was compared with cervical cancer screening status, 71% of the participants perceived themselves as having a low susceptibility to cervical cancer and as a result believed that cervical cancer screening was not necessary. This is in keeping with the National Health Interview Survey conducted in 1991 which revealed that most women understood that cervical cancer screening successfully detects cervical cancer early, but they did not see themselves as been at risk of developing cervical cancer, especially if they did not have any symptoms or had no family history of cervical cancer [16]. Majority of the study participants believed that cervical cancer was more common in older women and therefore screening was mainly essential in the older age group. This is consistent with findings of another study which reported that majority of the participants believed that older women are at greater risk of having cervical cancer [17]. Just like other previous studies conducted and found that both the screened and never screened either disagreed or strongly disagreed that the risk of cervical cancer increases with parity but agreed or strongly agreed that cervical cancer was more common to women who were HIV positive. Since there is an association between multiple sexual partners and HIV positive, the risk was also higher among women with multiple sexual partners [18,19].
Perceived barriers to seeking cervical cancer screening
Most participants did not have perceived barriers to cervical cancer screening, as the average response to barrier questions had a mean of less than 3. This is completely opposite to previous studies that reported many barriers among participants and non-participants of cervical cancer screening like pain, lack of convenient clinic times, lack of information, not knowing where to go for cervical cancer screening, too embarrassed to participate in cervical cancer screening, partner’s resistance to the woman’s participation in cervical cancer screening, lack of female screeners, etc as barriers to cervical cancer screening [7,8,18,19].
When comparing responses between the ever screened and the never screened, majority of the ever screened did not believe that participating in cervical cancer screening suggested that a woman is having sex (74%) as opposed only 26% of the never screened. Participants, both screeners and never screened, equally responded to the barrier questions in the questionnaire. No significant association between perceived barriers to cervical cancer screening and cervical cancer screening status suggests that most barriers to cervical cancer screening have been addressed. This is in contrast to other studies that found significant barriers among those never screened when compared to the screened [9,18,19].
Association between socio-demographic characteristics and perceived barriers of cervical cancer screening
This study did not find any significant association between socio-demographic characteristics and perceived barriers to participating in cervical cancer screening. All the various socio- demographic characteristics groups had equal perceived barriers to cervical cancer screening. This contrasts previous studies that report various barriers to cervical cancer screening among the poor, the less educated, the single and the married, etc [8,9,18]. The lack of barriers to cervical cancer screening in this study might suggest that with the most barriers have been addressed as a result of the Ministry of Health’s commitment to improve the uptake of cervical cancer screening through the provision of education to create awareness and the provision of infrastructure to improve access.
Limitations of the study
This study was limited by its cross-sectional design, use of selfreport and convenience sampling. Some women in the sample may have felt sensitive to report negative results, which may have introducing self-selected bias. This study only looked at women attending Mahalapye District Hospital in Botswana and hence it may be difficult to extrapolate to the larger population in Botswana or generalise the findings to the other populations.
Conclusion
The rate of participation of cervical cancer screening among women attending Mahalapye District Hospital is still far too low compared to the national target of greater than 75%. Most women did not specially point out perceived barriers such as embarrassment, pain, lack of convenient clinic time, lack of information, etc as barriers to seeking cervical cancer screening. Therefore, more work needs to be done aimed at increasing the awareness of perceived barriers to cervical cancer screening through provision of education/information, addressing misconception and beliefs as well as improving the sociodemographic condition through employment, education, monthly income and better residential area. Also suggesting policy makers to design intervention programs using appropriate models to increase awareness, testing and self efficacy of individuals through new policy for implementing the program.
Acknowledgment
The authors wish to thank the hospital management team for supporting to conduct the study.
Funding
No funding was received for the study.
Conflict of interest
None.
231
References
- Jamal A, Siegel R, Ward E, Murray T, Xu J, et al (2006) Cancer statistics, 2006. CA: A Cancer Journal for Clinicians 56: 106-30.
- Ferlay J, Bray F, Pisani P, ParkinDM, (2004) GLOBOCAN 2002: Cancer Incidence, Mortality and Prevalence Worldwide.” IARC Cancer Base No. 5, version 2.0. IARC Press, Lyon.
- Lee J, Seow A, Ling SL (2002) Improving adherence to regular pap smear screening among Asian women: a population-based study in Singapore. Health EducBehav 29:207-218.
- NygardJF, Skare GB, Thoresen SO (2002) The cervical cancer screening progrmme in Norway, 1992–2000: changes in Pap smear coverage and incidence of cervical cancer. J Med Screen 9:86-91.
- Devesa SS, Silverman DT, Young JL, Pollack ES, Brown CC, et al (1987) Cancer incidence and mortality trends among whites in the United States, 1947-84. J Natl Cancer Inst 79:701-70.
- McFarland DM (2003) Cervical Cancer and Pap Smear screening in Botswana: Knowledge and Perception. IntNurs Rev 50:167-75.
- BurakLJ, Meyer M (1997) Using the health belief model to examine and predict College women’s cervical cancer screening beliefs and behavior. Health Care Women Int 18:251-262.
- Bessler P, Aung M, Jolly P (2007). Factors Affecting Uptake of Cervical Cancer Screening Among Clinic Attendees in Trelawny, Jamaica. Cancer Control 14:4.
- Leyva M, Byrd T, Tarwater P (2006) Attitudes towards Cervical Cancer Screening: A Study of Beliefs among Women in Mexico. Californian J of Health Promot 4:13-24.
- Reid NG, BooreJRP (1991) Research Method and Statistics in Health care. London; Edward Arnold.
- Carey P, Gjerdingen DK (1993). Follow-up of abnormal Papanicolaou smears among women of different races. J FamPrac 37:583-587.
- Lerman C, Miller S, Scarborough R, Hanjani P, Nolte S, et al (1991) Adverse psychologic consequences of positive cytologic cervical screening. Am J ObstetGynecol 165:658-662.
- Harlan LC, Bernstein AB, Kessler LG (1991) Cervical cancer screening: who is not screened and why? Am J Public Health 81:885-891.
- Barron CR, HoufekJF (2001) Ethnic influences on body awareness, trait anxiety, perceived risk, and breast and gynecologic cancer screening practices. OncolNurs Forum 28:727-738.
- Suwatcharachaitiwong J (2004) Health Beliefs Concerning Cervical Cancer and Pap Smear Test Attendance Among Muslim Women [master’s thesis]. Songkla: Prince of Songkla University.
- Agurto I, Bishop A, Sanchez G, Betancourt Z, Robles S (2004) Perceived barriers and Benefits to cervical cancer screening in Latin America. Prev Med 39:91-98.