Keywords
Erectile dysfunction, penile prosthesis, surgical complications, surgical treatment.
Introduction
Erectile dysfunction ( ED) is the persistent inability to attain and maintain a sufficient erection for a satisfactory sexual performance [1]. ED has long been considered as a quality of life (QoL) issue rather than a medical condition [2]. Depending on the cause, ED is classified as organic, psychogenic or mixed [3]. The development of ED is generally considered to be multi-factorial with several risk factors such as diabetes mellitus, cardiovascular disease, smoking, aging, hormonal disturbances and metabolic syndrome.
The treatment for ED offers many options, which requires a structured strategy that depends on efficacy, safety and cost-effectivity as well as patient and partner satisfaction [4]. Oral pharmacotherapy and intracavernosal injections are the first-line treatment recommended by most surgeons, prior to moving onto prosthesis surgery [5]. Surgical management is the treatment of choice for patients who fail first-line treatment or for those who want a permanent solution. The results are generally improving in terms of erection, personal and partner satisfaction with satisfaction rates up to 70-87 % after appropriate consultations [6]. In spite of the encour aging results, the possibility of severe complications makes penile prosthesis implantation (PPI) a delicate surgery [7].
The lack of standardization for reporting surgical complications of PPI is an important issue in the urologic literature. Objective and reliable outcome data is requested by patients and payers to assess the quality and cost of health care. To report the complications of a certain procedure, standardization is necessary to allow comparison between different centers, within one center over time, and between different instruments and/or operating techniques for the same procedure. Satava and Clavien grading systems are the two most commonly used classification systems for reporting intraoperative and postoperative complications, respectively [8-14]. In the current study, we briefly went over the mechanisms of the complications of PPI surgery and ways to manage them. The aim of this study is to adapt the two most common grading systems of surgical complications, the Satava and the modified Clavien grading systems, to the surgical complications of penile prosthesis surgery.
Methods
Between Oct 1990 and Dec 2011, 422 patients with ED were treated with PPI. The complications and the other data were collected from the charts. We classified the postoperative complications according to the modified Clavien grading system [10] and the intraoperative complications according to the Satava system [14]. We defined the intra operative complications as; corporeal crossover (proximal or distal), corporeal perforation (proximal or distal and with and without urethral involvement), and bladder perforation. Postoperative complications were defined as; infection (periprosthetic infection, wound infection without the involvement of any part of the prosthesis and systemic infection), erosion, reservoir complications (herniation over the transversalis fascia, displacement near the iliac vessels or erosion into adjacent viscera), glandular problems (complaining of the loss of erection of the glans penis and glandular hypermobility) and mechanical failure (fluid loss, autoinflation, failure to deflate, aneurismal dilatation of the cylinders, buckling of the cylinders and pump problems).
We categorized the procedures as follows: A: Malleable PPI, B: Inflatable PPI, (B1: for 2 piece inflatable penile prosthesis (IPP), B2: for 3 piece IPP), C: Dual PPI with an artificial urinary sphincter (AUS), synchronously or metachronously (C1: A+ AUS, C2: B1+ AUS and C3: B2+ AUS). Type A, B1 and B2 surgeries were performed through an infrapubic, penoscrotal, and an infrapubic or penoscrotal incisions, respectively. Type C1, C2 and C3 surgeries were done using an infrapubic, penoscrotal, and infrapubic and/or penoscrotal, respectively, depending on whether the operation was a synchronous implantation or not.
The implants and the dilators were kept in antibiotic solution. The surgical field, implants and the instruments were washed with the same solution by an assistant throughout the procedure. An antibiotic prophylaxis was done and the general rules for disinfection during prosthetic surgery were obeyed meticulously [5,15]. Ice packs were used for 6-8 hours postoperatively. The urethral catheter was kept in place for one day and the patients were discharged at the end of the 1st postoperative day.
Results
The mean age was 58(40-74). The numbers of overall intraoperative and postoperative complications were 21(5%) and 45(10%), respectively.
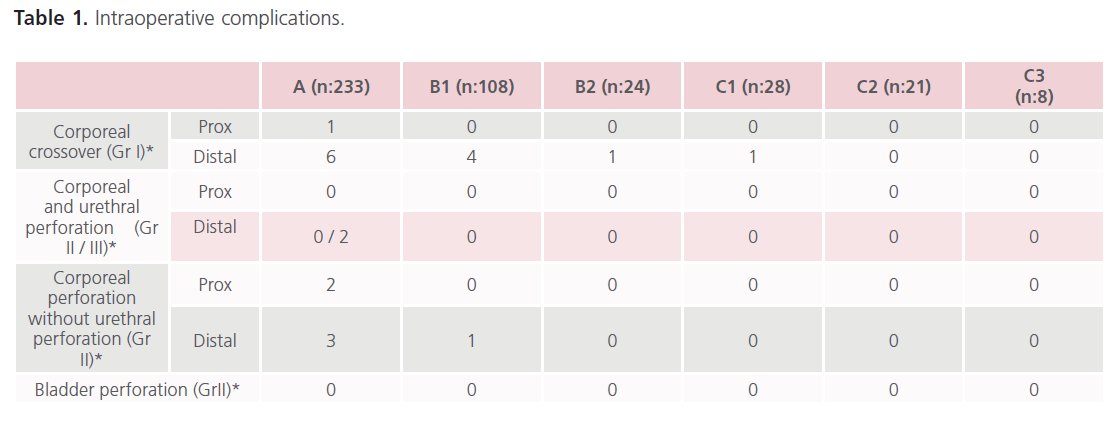
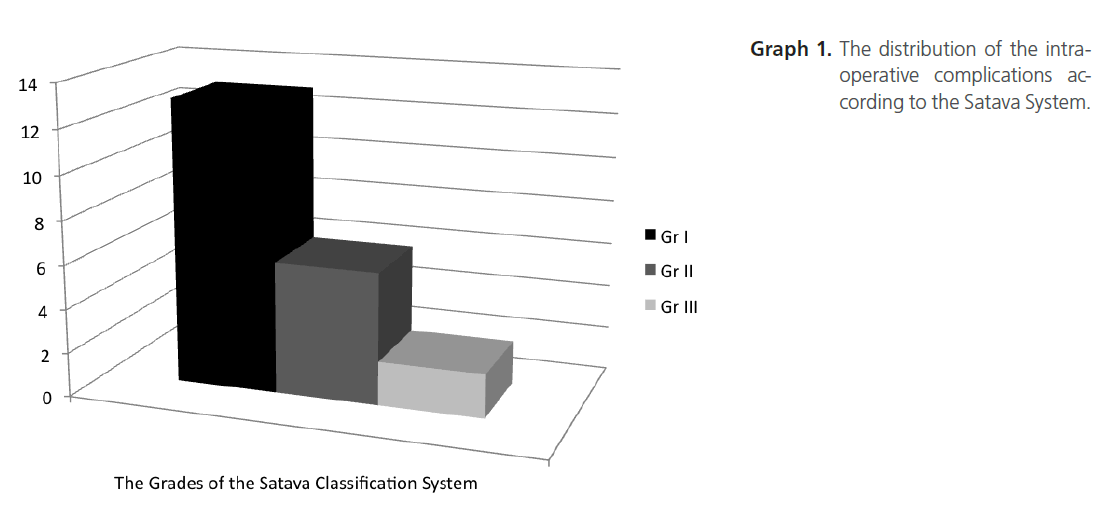
The distribution of intraoperative complications were; 13/21(62%), 6/21(29%) and 2/21(9%) for Grades 1, 2 and 3, respectively, according to the Satava classification system. Corporeal crossover (13/21) was the only complication classified as Gr I. Corporeal perforation without urethral involvement (6/21), urethral perforation which did not necessitate the abortion of the procedure (0/21) and bladder perforation (0/21) were classified as Gr II. Urethral perforation which resulted in termination of the procedure (2/21) was classified as Gr III (table 1, graph 1).
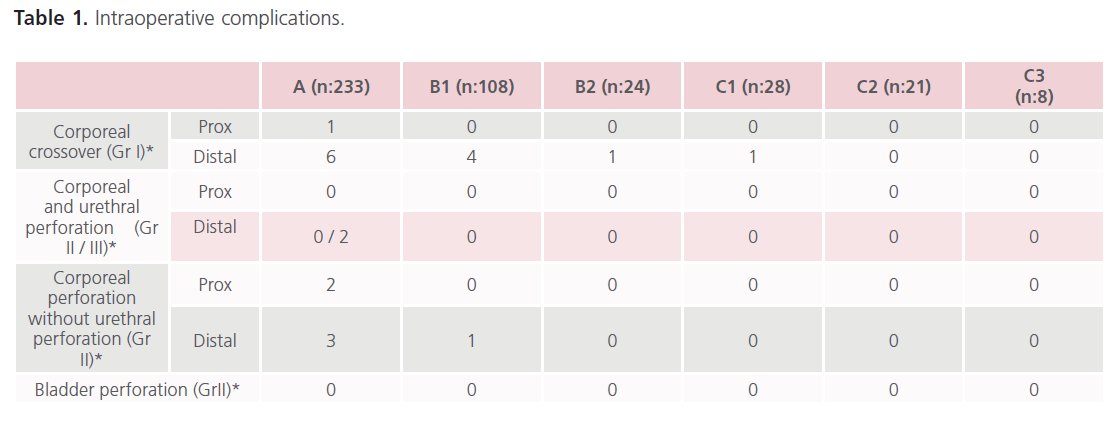
Table 1: Intraoperative complications.
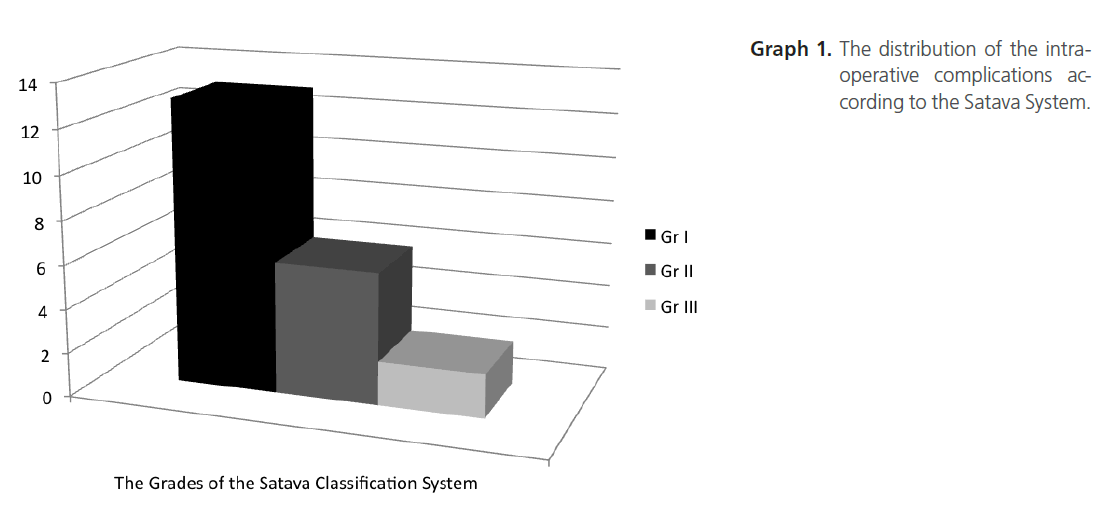
Graph 1 The distribution of the intraoperative complications according to the Satava System.
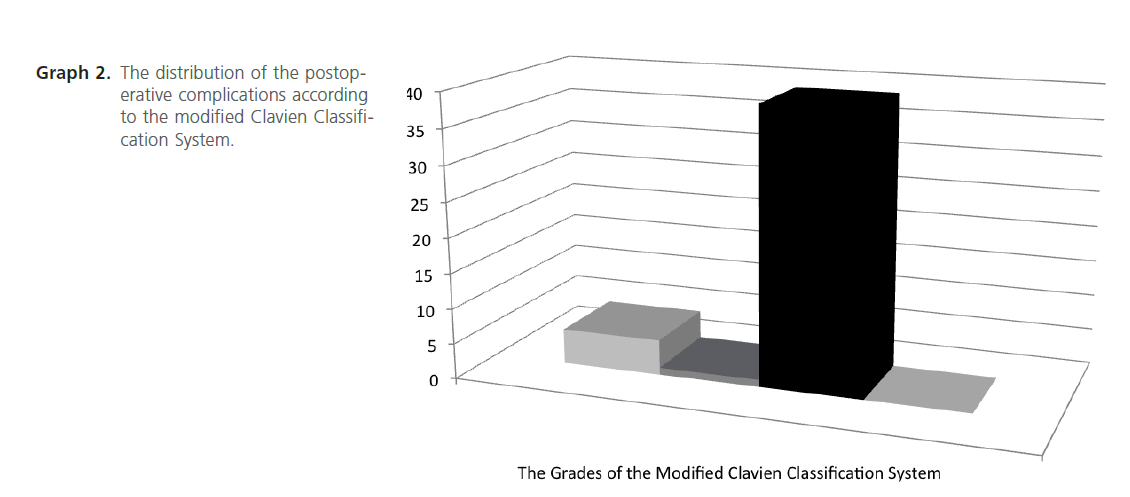
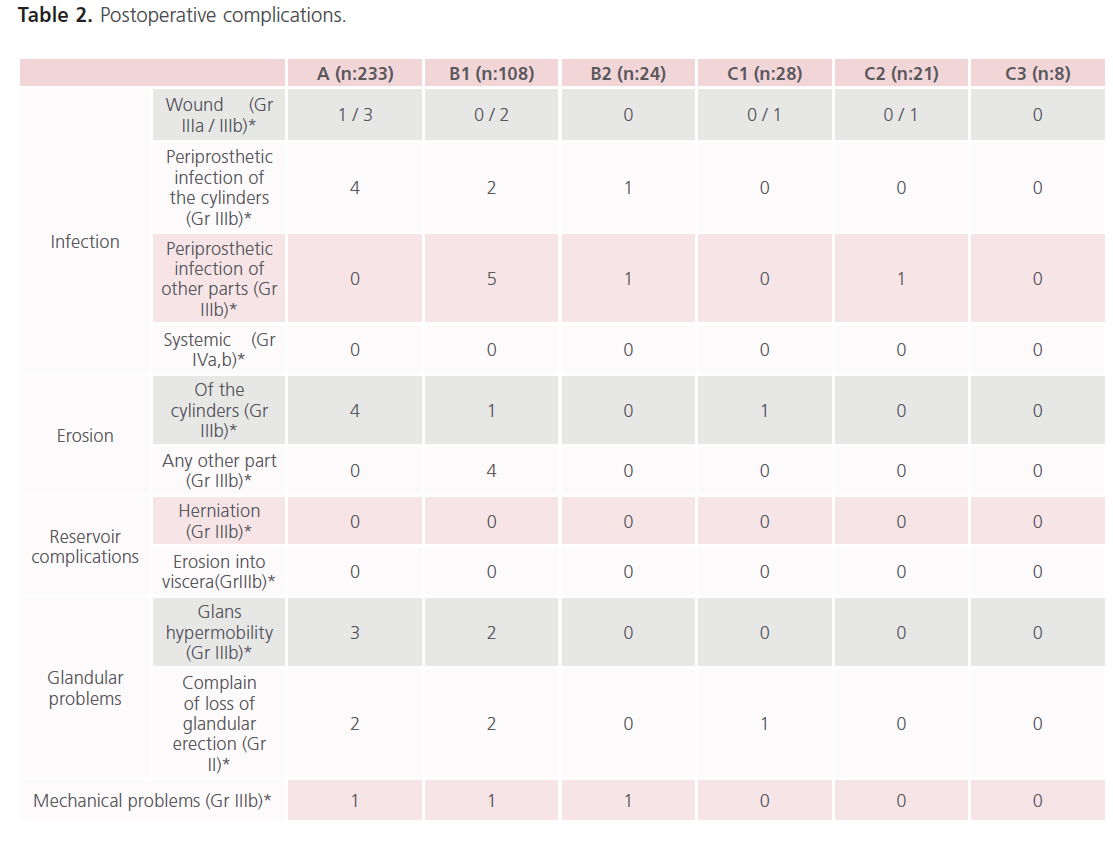
The distribution of postoperative complications were; 0, 5, 1, 39, 0, 0 and 0 for Grades I, II, IIIa, IIIb, IVa, IVb and V, respectively, according to the modified Clavien classification system. The complain of loss glandular erection was classified as Gr II(5/45). Wound infection was classified as either Gr IIIa(1/45) or Gr IIIb(7/45) according to the intervention necessary to heal it. The periprosthetic infections, any kind of erosion, reservoir complications, glandular hypermobility and mechanical problems were classified as Gr IIIb. Systemic infection was classified as either Gr IVa, or IVb. 5/45(11%), 1/45(2%) and 39/45(87%) of the postoperative complications were Gr II, Gr IIIa and Gr IIIb, respectively (table 2, graph 2).
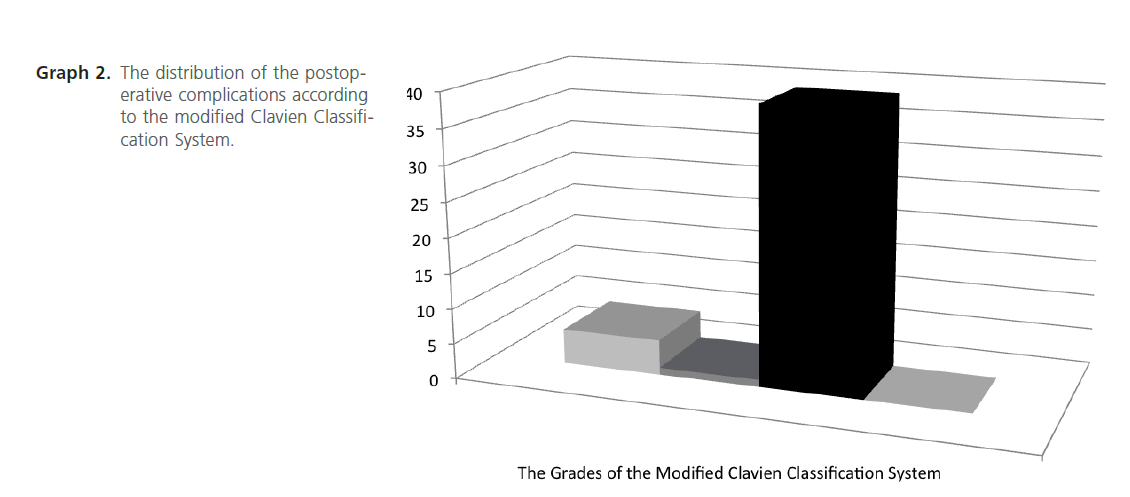
Graph 2 The distribution of the postoperative complications according to the modified Clavien Classification System.
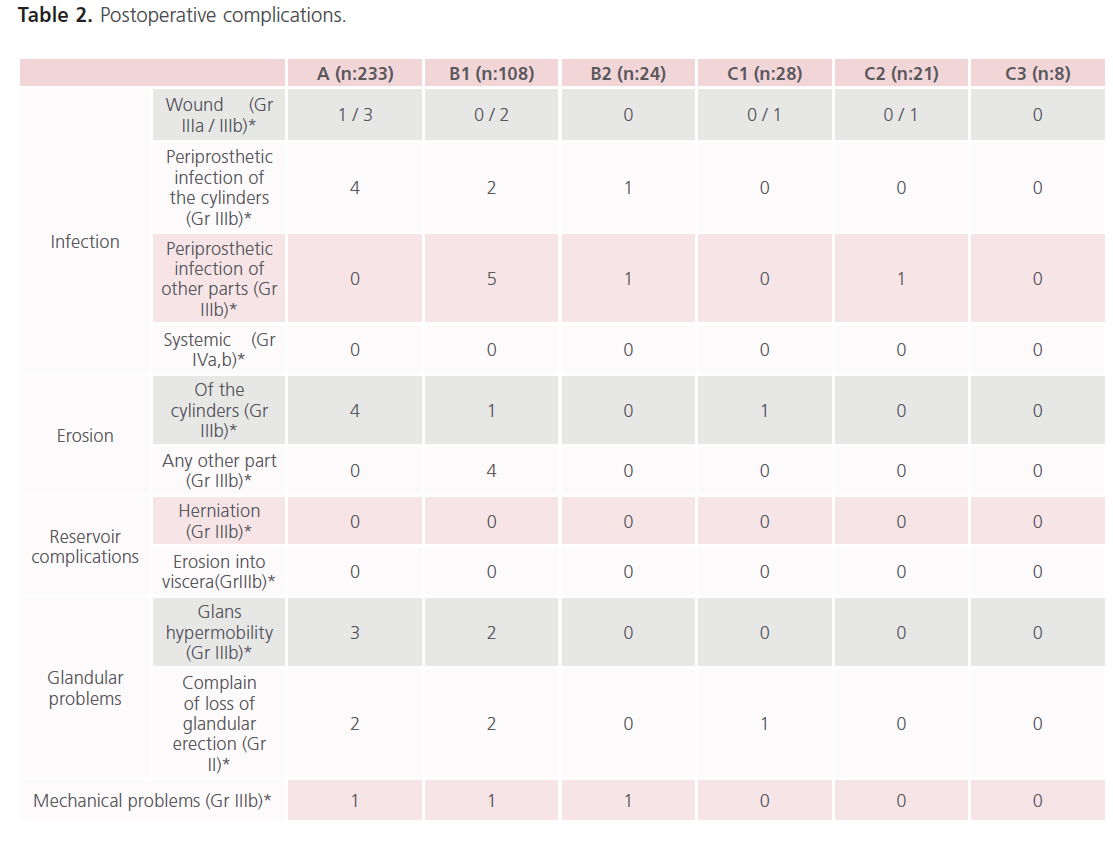
Table 2: Postoperative complications.
Discussion
PPI is the third-line and definitive therapy for ED in the era of effective and safe oral medications. The two and threepiece IPP are the types of prosthesis most commonly used in market now together with the malleable ones. These devices are subject to continuous development and have gained better mechanical reliability and safety in the last decades [7], but device-related complications together with the well known complications of PPI can still occur [5,16,17]. Despite of numerous articles emphasizing the complications of PPI, standardization of these complications is lacking. Clavien et al. first published a system in which complications were systematically graded which is the basis of the Clavien grading system. In 2004, Dindo et al reevaluated and modified their own criteria to increase its accuracy and applicability, which is increasingly becoming more and more popular in urology. The modified Clavien system focuses mainly on the therapeutic consequences of a complication, emphasizing the level of the intervention required. The system is generally used to report complications occurring up to 90 days postoperatively, although it can also be applied for late complications [8,9]. The Satava classification system deals with intraoperative complications (Gr I: incidents without consequences, Gr II: incidents repaired intraoperatively, Gr III: incidents requiring reoperation) [14].
Thorough discussion of the pathogenesis and detailed analysis of all the complications of PPI, or the historical aspects of the development of prosthetic devices is far beyond the scope of this article. We will mention briefly about the complications and the ways to manage them to help categorize each complication according to the present classification systems.
Intraoperative complications
Corporeal crossover: Corporeal crossover more commonly occurs during distal dilatation of the cavernosal bodies and will not cause any ill consequences if proper rerouting and replacement of the cylinders is done. There is no need to find the place of the septal perforation and fix it. Some authors may even be underreporting this event. The best way to avoid important problems due to a crossover during IPP placement is to place the Keith needles bilaterally before introducing the cylinders. The authors classified this occasion as Gr I.
Corporeal perforation without urethral involvement: A proximal corporeal perforation should be suspected when the dilators inside the two cavernosa are asymmetric or if there is a significant difference in their length. A proximal perforation must be repaired directly or a well-demonstrated method like the windsock patch repair must be done [18,19]. Distal corporeal perforation should also be repaired intraoperatively. If corporeal perforation is repaired properly intraoperatively, it will not cause any important consequences. So it can be categorized as Gr II.
Corporeal perforation with urethral involvement: Urethral perforation generally occurs during distal dilatation of the cavernous bodies especially if there is overt fibrosis. If the defect is large, the reasonable choice is to abort the procedure according to the authors’ point of view. If the defect is small, there are different opinions about aborting the procedure. If one side is successfully dilated and ready for introducing a single cylinder and a perforation occurs on the contralateral side, the surgeon may choose to place the cylinder in the intact side after plugging the tubing of the perforated side [5] and leave the urethra for spontaneous healing with a foley catheter for 10 days. Or if the surgeon can repair the small defect intraoperatively, then again he/she may go on with the surgery with a foley catheter for an appropriate time period. But if urethral perforation occurs during the dilatation of the initial side, then the powerful choice is to abandon the procedure for spontaneous recovery of the urethra, only that the surgeon must keep in mind the difficulty he/she must face on the next operation due to fibrosis [20]. In case of any kind of urinary involvement, another point of view may be abandoning the procedure. Diversion techniques like perineal urethrostomy or suprapubic cystostomy can be used intraoperatively. The urethral involvement is obviously an event with consequences. According to the course of the surgery, it can be classified depending on whether the procedure is continued or aborted, as Gr II or Gr III, respectively.
Bladder perforation: This is an extremely rare condition with an empty bladder and must be dealt intraoperatively with primary closure of the defect and keeping the catheter long enough for the healing process. There is no need to abort the procedure due to a bladder perforation; this complication can be classified as Gr II.
Postoperative complications
Infection: Infection is one of the most fearsome complications which can occur within a wide range of time, from a few weeks to more than a year [21]. Most infections associated with penile prostheses occur within the first 3 months; with a typical sign of persistent, unchanging or increasing pain. With antibiotic prophylaxis, the infection rate is 2-3% and may further be reduced by using antibiotic-impregnated or hydrophilic-coated implants [4,22,23]. Infection is more common in patients with spinal cord injuries, diabetes mellitus, and history of urinary tract infection or in those having a secondary revision or a replacement operation. Inadequate perioperative prophylaxis and lax sterile protocol, prolonged hospitalization, prolonged operative time, and repeat implantations are some of the important predisposing factors. Before the operation, it is very important to apply infection control protocol consisting of antibiotic prophylaxis, intraoperative shaving, scrubbing of the operation site for10- minutes with antiseptic solutions prior to painting the skin with iodophore [5]. In the authors’ practice, a first generation cephalosporin given 1-2 hours prior to surgery is adequate as surgical prophylaxis for patients with no previous history of genitourinary or prosthetic infection. For others, a surgical prophylaxis with aminoglycoside and vancomycin combination is recommended [5,17]. Infections are generally caused by S. epidermidis and S. aureus, followed by Gram (-) bacteria and anaerobic organisms. Systemic antibiotic therapy is not sufficient to treat this complication. Although it is stated in the literature that either immediate or delayed replacement of a new device after the removal of all the pieces of the device is necessary [17,18], we have the experience of 4 patients with infection limited with the pump area macroscopically. We performed salvage surgery to these patients as quickly as possible. During the salvage surgery, we separated the tunica albuginea at the point of insertion of the pipes. If there was any purulent drainage coming out from the cavernosa with mild massage, the device was completely extruded, and a new device was introduced after aggressive and thorough debridement and lavage of the area of the infected tissues with at least 3 kinds of antiseptic solutions; including povidone iodine and hydrogen peroxide and antibiotics as explained elsewhere [17]. But if there was no purulent discharge, the pipes and the pump were washed and rubbed aggressively with the same solutions and relocated at an uninfected new pouch. Then, we inserted a 12f. Nelaton catheter with little holes created alongside with fine scissors in and out through the scrotal skin to wash and drain the operative field with the closed system of continuous antibiotic lavage in a sterile fashion. We sustained the lavage for 3 days. By this method 3 of the 4 patients with infected pumps were salvaged successfully. All the treatment options for infected prosthesis necessitate postoperative surgical intervention with general anesthesia which means that it should be classified as Grade IIIb complication according to the modified Clavien Grading System [9].
Erosion: Being mostly in combination with device infection, erosion due to any part of the device necessitates surgical repair. Semirigid prosthesis are more prone to cause erosion into the urethra especially on paraplegic or quadriplegic patients with an indwelling catheter or doing clean intermittent catheterization (CIC). The problem is more common in diabetics or patients having a redo implant procedure due to different reasons. Erosion is present as a late complication in up to 80% of patients with an indwelling catheter or doing CIC [5]. Using inflatable devices and constructing a perineal or suprapubic cystostomy helps resolve the problem [24]. In case of a lateral extrusion of the cylinder, distal corporoplasty has better results than windsock reinforcement [25-28]. All the treatment options for erosion necessitate surgical correction with general anesthesia which means that it should be classified as Grade IIIb [9].
Reservoir complications: These are infrequent complications of three piece IPP, including herniation over the fascia with scrotal migration with the incidence of 0.7% [5] or even more rarely erosion into adjacent viscera or displacement laterally near the iliofemoral vessels, causing deep vein thrombosis. Reservoir herniation necessitates surgical intervention under general anesthesia and should be classified as Grade IIIb [9].
Mechanical complications: The most common complications are fluid loss, cylinder rupture, autoinflation and mechanical breakage. As the penile prosthesis become highly developed and technically advanced, the mechanical survival of a three piece IPP is found to be 81.3% at 10 years [29]. When there is a mechanical problem, it needs a surgical correction under general anesthesia which makes it a Grade IIIb complication [9].
Glans problems: Glandular problems are generally of two types; lack of glandular tumescence or coolness and glans hypermobility (SST deformity). The complain of the loss of glandular tumescence can be overcome with PDE-5 inhibitors or intraurethral pharmacological treatment. So it can be classified as Grade II [9]. Glans hypermobility is the drooping of the glans downwards and can be corrected by replacing the cylinders with longer ones. Or if the problem is due to an anatomic variation in the relationship between the tips of the corporeal bodies and the glans penis, this may be corrected by glanulopexy first described by Ball et al. [30,31]. This complication necessitates surgical correction under general anesthesia and should be classified as Grade IIIb [9].
There are some potential limitations of our study; being retrospective is one of them. Secondly, malleable prostheses are the most common devices encountered in the study, which are not the first choice implants used in market today. The complications and the salvage procedures are well-known in the literature; to discuss them thoroughly is far beyond the scope of this article.
Among the intraoperative complications; corporeal crossover will cause no important consequences, and may have been underreported. If corporeal crossover is neglected as an intraoperative complication, the Satava system is a valid tool for grading intraoperative complications (graph 1).
The modified Clavien grading system offers the same grade (IIIb) for 87% (39/45) of all of the postoperative complications (graph 2). Periprosthetic and some of the wound infections, erosion of any part of the device, glans hypermobility and all the mechanical problems fall into the category of IIIb complications. The distribution of numbers of patients within individual grades of complications is far beyond giving the idea that there is an evenly distribution. The authors believe that the modified Clavien system is not the ideal tool for classifying postoperative complications of PPI. A more detailed, reproducible and evenly distributable system is necessary for classifying the postoperative complications of PPI.
The categorization (A, B1, B2, C1, C2, C3) of the operations demonstrated in our series is useful for standardizing the type of the operation and the nature of the implant used.
Penile prosthetic surgery has important complications. Satava grading system works well for reporting the intraoperative complications, but the modified Clavien grading system cannot afford a reproducible and even grading system for classifying postoperative complications. A standard, unique and broadly acceptable classification system for monitoring and reporting the outcomes of PPI is lacking and deserves more investigation.
2342
References
- Lue TF, Giuliano F, Montorsi F, Rosen RC, Andersson KE, Althof S. et al. Summary of the recommendations on sexual dysfunctions on men. J Sex Med. 2004; 1: 6-23.
- Benard F. Erectile dysfunction: a vascular disease in the field of urology. Can Urol Assoc J. 2001; 5 (5): 352-3.
- Lizza EF, Rosen RC. Definition and classification of erectile dysfunction: Report of Nomenclature Committee of the International Society of Impotence Research. Int J Impot Res.1999; 11: 141-3.
- Wespes E, Amar E, Eardley I, Giuliano F, Hatzichristou K, Hatzimouratidis K. et al. Guidelines on Male Sexual Dysfunction: Erectile dysfunction and premature ejaculation. EAU Guidelines 2012; 495-543.
- Sadeghi-Nejad H. Penile prosthesis surgery: A review of prosthetic devices and associated complications. J Sex Med. 2007; 296-309.
- Montague DK, Angermeier KW. Penile prosthesis implantation. Urol Clin North Am. 2001; 28: 355-61.
- Bettocchi C, Palumbo F, Spilotros M, Palazzo S, Saracino GA, Martino P. et al. Penile prostheses. Ther Adv Urol. 2010; 2 (1): 35-40.
- Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 1992; 111: 518-26.
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240: 205-13.
- Mamoulakis C, Efthimiou I, Kazoulis S, Christoulakis I, Sofras F. The modified Clavien classification system: a standardized platform for reporting complications in transurethral resection of the prostate. World J Urol. 2011; 29: 205-210.
- Morgan M, Smith N, Thomas K and Murphy DG. Is Clavien the new standard for reporting urological complications? BJU Int. 2009; 104: 434-6.
- Guven S, Istanbulluoğlu O, Gul U, Ozturk A, Celik H, Aygun C. et al. Successful percutaneous nephrolithotomy in children: Multicenter study on current status of its use, efficacy and complications using Clavien classification. J Urol. 2011; 185: 1419-24.
- Zuazu JR, Hruza M, Rassweiler JJ, de la Rosette JJ. The Clavien classification system to optimize the documentation of PCNL morbidity. Arc Ital Urol Androl. 2010; 82: 20-2.
- Satava RM. Identification and reduction of surgical error using simulation. Minim Invasive Ther Allied Technol. 2005; 14: 257. 15.
- Montague DK, Angermeier KW, Lakin MM. Penile prosthesis infections. Int J Impot Res. 2001; 13: 326-8.
- Garaffa G, Li C, Moncada I, Ralph DJ. Surgical management of erectile dysfunction. Arch Esp Urol. 2010; 63 (8): 728-38.
- Hellstrom WJG, Montague DK, Moncada I, et al. Implants, Mechanical Devices, and Vascular Surgery for Erectile Dysfunction. J Sex Med. 2010; 7: 501-23.
- Carson CC, Noh Ch. Distal penile prosthesis extrusion: treatment with distal corporoplasty or Gortex windsock reinforcement. Int J Impot Res. 2002; 14: 81-4.
- Szostak MJI, Pizzo JJ, Sklar GN. The plug and patch: A nex technique for repair of corporeal perforation during placement of penile prosthesis. J Urol. 2000; 163: 1203-5.
- Jarow JP. Risk factors for penile prosthetic infection. J Urol. 1996; 156 (2 Pt. 1): 402-4.
- Kabalin LN, Kessler R. Infectious complications of penile prosthesis surgery. J Urol. 1988; 139: 953-5.
- Carson CC. Efficacy of antibiotic impregnation of inflatable penile prosthesis in decreasing infection in original implants. J Urol. 2004 Apr; 171 (4): 1611-4.
- Wolter CE, Hellstrom WJ. The hydrophilic-coated inflatable penile prosthesis: 1-year experience. J Sex Med. 2004 Sep; 1 (2): 221-4.
- Steidle CP, Mulcahy JJ. Erosion of penile prosthesis: A complication of penile prosthesis cylinders. J Urol. 1989; 142: 736-9.
- Smith CP, Kraus SR, Boone TP. Management of impending penile prosthesis erosion with a polytetrafluoroetylene distal wind sock graft. J Urol. 1998; 160 (6 Pt. 1): 2037-40.
- Zermann DH, Kutzenberger J, Sauerwein D, Schubert J, Loeffler U. Penile prosthetic surgery in neurologically impaired patients: Long-term follow-up. J Urol. 2006; 175: 1041-5.
- Mulcahy JJ. Distal corporoplasty for lateral extrusion of penile prosthesis cylinders. J Urol. 1999; 161: 193-5.
- Mulcahy JJ. Surgical management of penile prosthesis complications. Int J Impot Res. 2000; 12 (suppl. 4): S108-11.
- Dhar NB, Angermeier KW, Montague DK. Long-term mechanical reliability of AMS 700CX trademark/CXM inflatable penile prosthesis. J Urol. 2006; 176: 2599-601.
- Ball TP, Jr. Surgical repair of penile “SST” deformity. Urology 1980; 15: 603-4.
- Mulhall JP, Kim FJ. Reconstructing penile supersonic transporter (SST) deformity using glanulopexy (glans fixation). Urology 2001; 57: 1160- 2.