Ehsan Soolari1, Amin Soolari 2 and Ahmad Soolari3
1College of Chemical and Life Sciences, University of Maryland, USA
2Churchill High School, Potomac, MD, USA
3Private periodontal practice in Silver Spring and Potomac, Maryland, USA, Diplomate, American Board of Periodontology.
Introduction
Multiple myeloma patients with a history of long term use of IV Bisphosphonates are at risk for complications of ONJ. One of the major precipitating factors for ONJ is tooth extraction, which is reported to be the cause of the ONJ lesions.[7] Other factors such as radiation therapy and invasive surgical procedures have been noted as predisposing factors as well.[2] Multiple factors likely contributed to the initial and continued expansion of the necrotic bone from a stable and small lesion (4 x 2 x 2 mm), into a symptomatic and large lesion (6 x 12x 4 mm), which, in turn, has remained outsized and active. At the present time there is considerable confusion among patients and practitioners about the prevention and treatment of osteonecrosis of the jaw. To this day, there is no solid treatment plan or option that has been agreed upon universally in the medical and dental fields as to how to combat ONJ and the complications it brings forth. A recently published article in the January of 2008 by Glick states “some studies do not help clarify the potential adverse effects of dental treatment in patients taking bisphosphonates.” [15]
The progressive and aggressive nature of the disease presented in this case report demand attention. However, it is important to keep in mind such important factors like the potency of the BP used to treat the patient, the duration of treatment with BPs, and the types of surgical procedures recommended for the patient at risk for ONJ due to previous intravenous bisphosphonate use. In order to alleviate the risk of ONJ in these patients, our jobs as practitioners should be to identify those individuals at risk, and do everything we can in order to strive for the prevention of this condition. By continued correspondence between healthcare providers, dental surveillance and prophylactic care, and most importantly, early diagnosis and management, morbidity resulting from ONJ due to bisphosphonate use may be reduced greatly.[1]
Also, through continued research and reports on the subject matter, more successful treatment plans will arise.
In this report, we present a BRONG case of a patient on IV Bisphosphonate with a chief complaint of a “sticky, paint-like smell”, and a “salty/sour tasting material” in the mouth. There is no predictable treatment option for resolution of non healing lesion in anterior mandible. However, The PBSCD rinse was able to speed up the sequestration of necrotic bone and complete closure of the lesion.
Case:
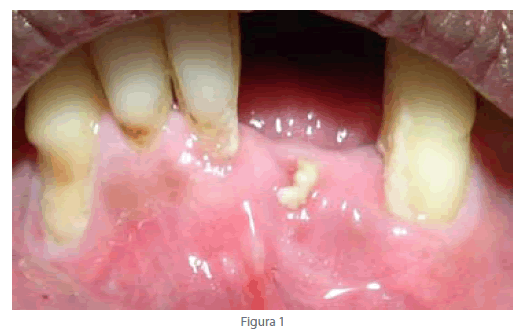
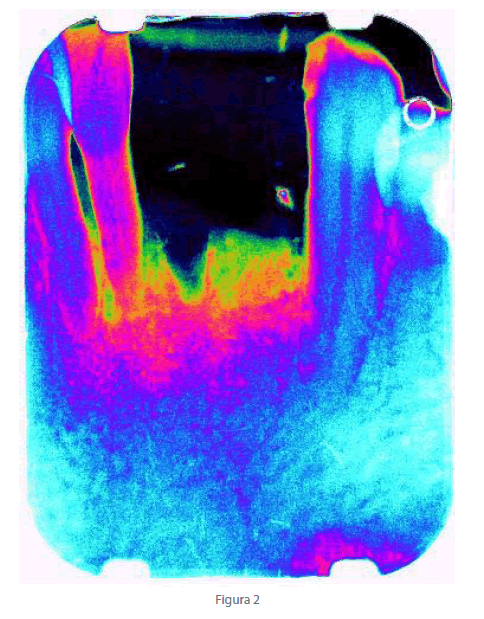
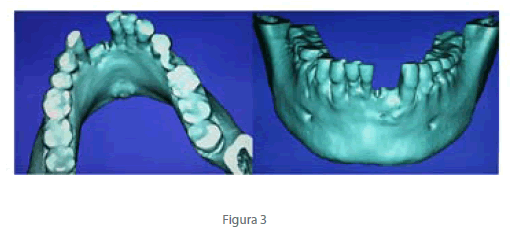
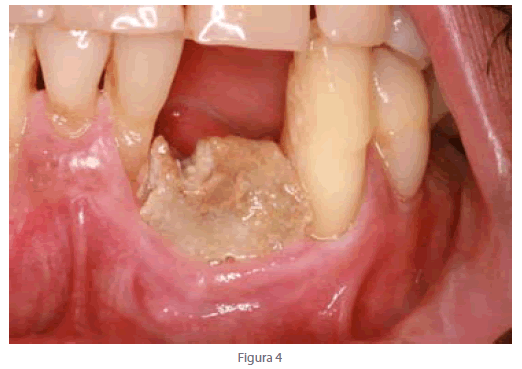
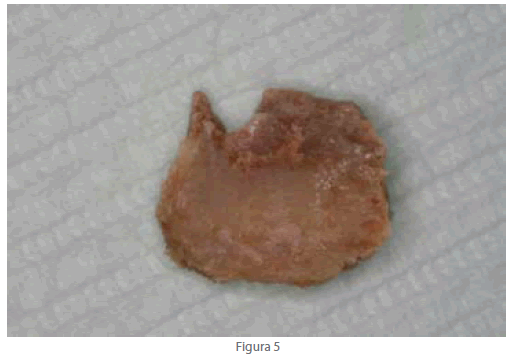
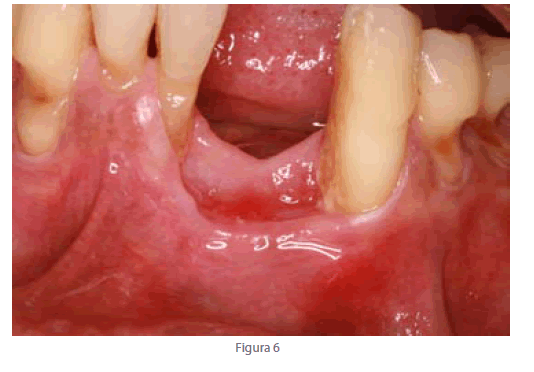
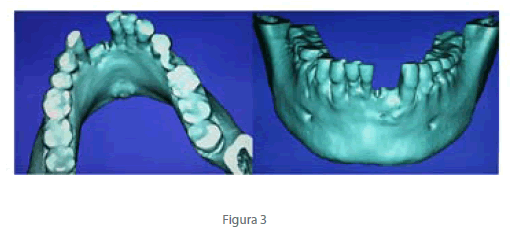
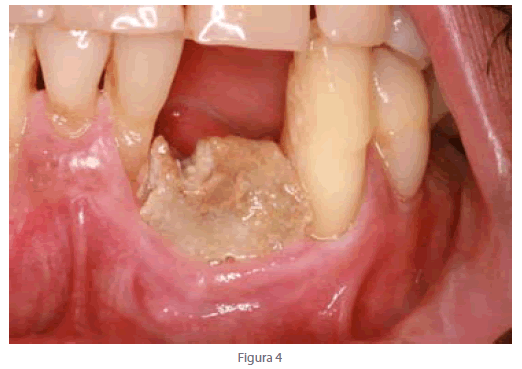
Patient is a 64 year old African American with a history of long term use of IV Bisphosphonate. The medical consultation with the patient’s hematologist/oncologist revealed that the patient was diagnosed with multiple myeloma in early 2005 and initially started on Dexamethasone and had received 4 mg zoledronic acid treatments intravenously, on a monthly basis, until January 2007 (six month post-extraction of tooth # 24 and two years post treatment with zoledronic acid), when the treating medical personnel had discovered the emergence of ONJ. However, the discontinuation of zoledronic acid treatments in January 2007 did not help our patient. This finding is in agreement with Ruggiero et al, whom stated that “there is no evidence to suggest interrupting bisphosphonate therapy will prevent or lower the risk of ONJ.”[12,13] Clinical (Figure 1) and radiographic (Figure 2) evaluation revealed 2 x 4 x 2 mm size lesion on extraction site, which was asymptomatic and stable in Feb 2008. Three dimensional image of the area revealed break in cortical plate and a non healing socket (Figure 3). The lesion became aggressive and increased in size (Figure 4). Patient called and stated that he has aches and pain on mandibular anterior area.
Patient was treated with Augmentin 500 mg 30 tab I. P.O. TID and Chlorohexidine16oz rinse twice daily. Patient response was positive and stated that he felt much better. Aches were gone but chief complained remained unresolved as how to close the open wound, which was easy for patient to see it on a daily basis.
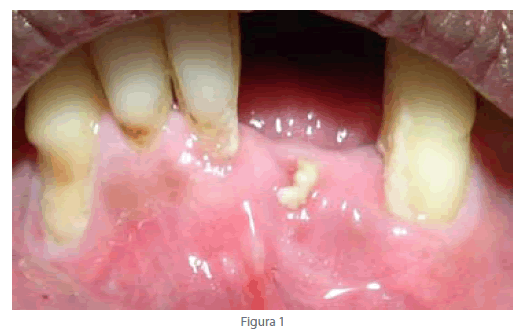
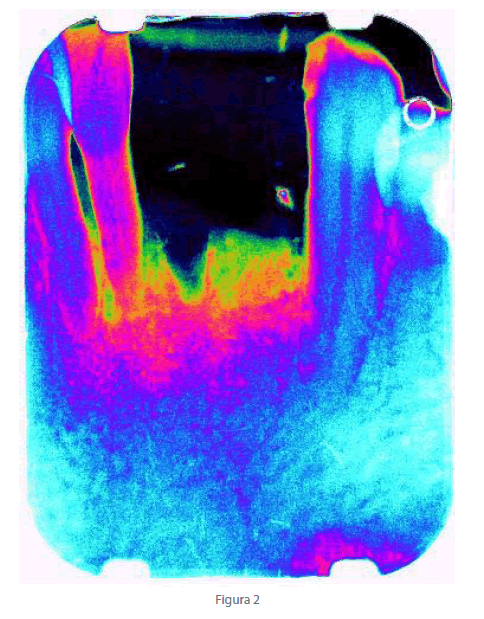
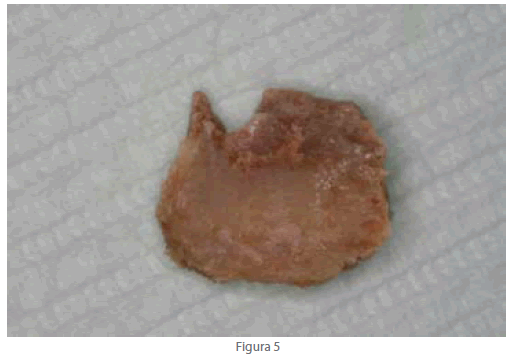
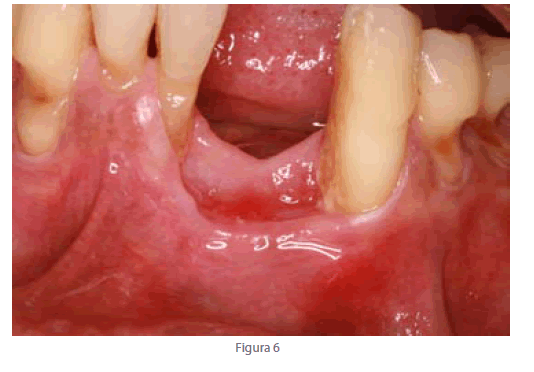
Patient was instructed to rinse with the PBSCD (CloSYS II-Rowpar Pharmaceuticals) for 30 second three times a day. Four month later patient presented to our office with the necrotic bone in his hand (Figure 5). Patient was happy with the mouth wash and stated that the rinse helped him getting rides of the loose bone. Clinical evaluation disclosed complete soft tissue healing on previously exposed necrotic bone on mandibular anterior region (Figure 6). We recommend this product. Our results are in agreement with the previous report by Marder (2009) that the PBSCD has potential rinsing solution to facilitate release of necrotic bone and closure of an open wound.
Discussion
Osteonecrosis of the jaw (ONJ) refers to necrotic jawbone due to decrease in blood supply—leading to decay, rotting, and infection in the diseased regions [1-3]. The uses of bisphosphonates (BPs), analogs of pyrophosphonates [4,5], usually prescribed in response to certain cancer treatments [6-12], have been linked with ONJ [3,4,7,8] and have been speculated to be a cause of the condition [14-15]. BPs are recommended to prevent bone resorption by suppressing all activities, and in particular, reducing the bone resorption activities of the osteoclast—it has been noted however, that over suppression of osteoclastic activity may lead to ONJ. The condition most often presented itself following an invasive dental procedure, such as an extraction [3,5,7]. The majority of these ONJ patients were also being treated due to multiple myeloma and breast cancer, which had been metastatic to the bone [3,5,6-12]. The oral bisphosphonate impose much smaller risk in developing BRONG. The 2008 advisory statement of ADA concluded that the risk of developing bisphosphonate –associated osteonecrosis (BON) of the jaw remains low and current screening and diagnostic tests are unreliable for predicting patient’s risk of developing the condition. The expert panel recommended routine general dental care should not be modified solely because of the patient’s use of oral bisphosphonates.[13].Dr. Marder (2008) has reported successful treatment outcome of BON with phosphate buffer-stabilized 0.1% chlorine dioxidecontaining mouth wash (CloSYS II-Rowpar Pharmaceuticals). Authors speculated that this mouthwash has anti inflammatory /anti fungus activities.
We recommended that patient used PBSCD for 30 seconds 3 times a day. Patient was happy with the mouth wash and stated that the rinse help getting rid of the loose bone. Clinical and radiographic evaluation disclosed complete soft tissue healing on previously exposed necrotic bone on mandibular anterior region. However, the radiograph revealed the radiolucency extended to adjacent teeth # 22 and 26. Our main concerns are loss of # 26 and 27 with subsequent bone exposure. Patient was instructed to use this mouthwash indefinitely.[14]
In conclusion, there is a non invasive treatment option is available for patients who are suffering from the BRONJ. The PBSCD facilitated sequestration of a hard to hide necrotic bone in anterior mandible. Complete soft tissue closure of a non healing lesion made patient very happy.
Acknowledgements
The authors, in reference to this case report, have no affiliation or financial support from any institution in the completion of this study.
2583
References
- Quirynen M, Teughels W, Haake SK, Newman MG. Microbiology of periodontal diseases. In: Carranza’s clinical periodontology. Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds. Elsevier, St. Louis, 10th Edition, 2006, pp.134-69.
- Migliorati CA. Bisphosphanates and oral cavity avascular bone necrosis. J Clin Oncol 2003;21(22):4253-4.
- Woo SB. Osteonecrosis of the jaw and bisphosphonates. N Engl J Med 2005;353(1):99-102.
- Wang J. Osteonecrosis of the jaws associated with cancer chemotherapy. J Oral Maxillofac Surg 2003;61(9):1104-7.
- Woo SB, Hellstein JW, Kalmar JR. Narrative [corrected] review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med. 2006 May 16;144(10):753–61. Erratum in: Ann Intern Med. 2006 Aug 1;145(3):235.
- Gralow J. Evolving role of bisphosphonates in women undergoing treatment for localized and advanced breast cancer. Clin Breast Cancer 2005; 5 Suppl(2):S54-62.
- Bagan JV. Avascular jaw osteonecrosis in association with cancer chemotherapy: series of 10 cases. J Oral Pathol Med 2005;34(2):120-3.
- Dimopoulos MA, Kastritis E, Anagnostopoulos A, Melakopoulos I, Gika D, Moulopoulos LA, Bamia C, Terpos E, Tsionos K, Bamias A. Osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates: evidence of increased risk after treatment with zoledronic acid. Haematologica. 2006 Jul;91(7):968-71.
- Calvo-Villas JM .Osteonecrosis of the jaw in patients with multiple myeloma during and after treatment with zoledronic acid. Med Clin (Barc). 2006 Oct 21;127(15):576-9.
- Badros A, Weikel D, Salama A, Goloubeva O, Schneider A, Rapoport A, Fenton R, Gahres N, Sausville E, Ord R, Meiller T. Osteonecrosis of the jaw in multiple myeloma patients: clinical features and risk factors. J Clin Oncol. 2006 Feb 20;24(6):945–52.
- Ruggiero SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg 2004;62(5):527-34.
- Ruggiero SL. Practical guidelines for the prevention, diagnosis and treatment of osteonecrosis of the jaw in patients with cancer. J Oncology Practice 2006;2(1):7-14.
- Edwards BJ et al: Updated recommendations for managing the care of patients receiving oral bisphosphonate therapy. JADA 2008; 139(12):1674-1677
- Marder, MZ, Marder, RW: Bisphosphonate-Associated Osteonecrosis Experiences in a Private Practice: Dent Today; Oct 2008, 27 (10)99-103
- Glick M. Closing in on the Puzzle of ONJ. J Am Dent Assoc. 2008; 139: 12-15.