Keywords
Femoroacetabular impingement; Osteoarthritis; Prognosis
Introduction
The femoroacetabular impingement (FAI) disease has recently become a popular topic in the hip preservation and sport literature. FAI is a frequent pathology that occurs due to an abnormally shaped proximal femur and/or acetabulum resulting in an abnormal contact between the femoral head-neck junction and the acetabular rim. It is considered to be the main cause of early hip osteoarthritis, especially in young and active patients [1-11].
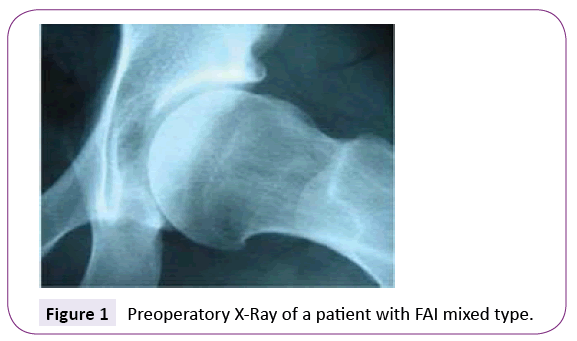
There are three types of FAI: cam, pincer and mixed. The first, cam type, is from femoral origin and is caused by an insufficient concavity of the femoral head–neck junction, which creates an increased radius of curvature that is mismatched for the more congruent acetabulum [2,12,13]. Its origins can be either by a primary bone protrusion at the femoral head-neck junction (which can correspond to an abnormality in femoral epiphysis growth) [5]; or due to a primary retroverted femoral neck or head [6], posttraumatic [7] or related to pathologies such as Perthes disease [8,9] or slipped capital femoral epiphysis [10-12]. The second, pincer type, is originated at the acetabulum, where there is a focal over coverage (primary anterior over coverage or in the acetabular retroversion) or general over coverage of the femoral head (coxa profunda, acetabular protrusion) [1,3]. The impingement is mixed when both components coexist: cam and pincer [13-15] (Figure 1).
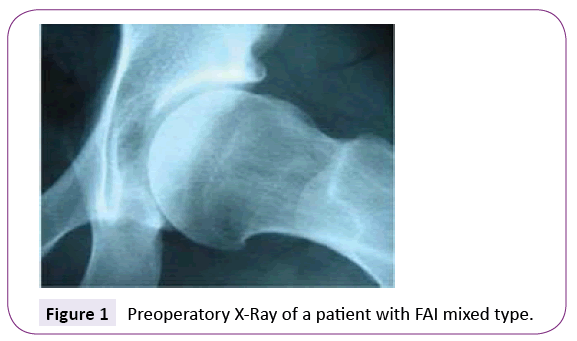
Figure 1: Preoperatory X-Ray of a patient with FAI mixed type.
Labral and chondral injuries related to the FAI are frequent [1,2,16,17]. They are produced by recurrent microtraumatisms [17] and are usually located in the anterosuperior region. Cam type impingement lesions are labral disinsertions of the adjacent acetabular cartilage [1,3,16], while in the pincer type impingement more extensive and intra-substance labral tears are observed [3], with less profound acetabular chondral lesions [1,16] and a present chondral contre-coup injuries [4,18].
FAI prevalence has been estimated in 10-15% of whole population [19]. It generally occurs in young patients aged 20-40, active and sports players [1,3,19]. Cam impingement is more frequent in young men, while pincer impingement has been observed more in middle aged women [1,3,20]. According to a systematic review, the prevalence of an asymptomatic cam deformity is 37%-54.8% in athletes versus 23.1% in the general population. The prevalence of asymptomatic hips with pincer deformity was 67% (range 61% to 76% between studies) [21].
Clinical presentation is typically with an insidious and sporadic progressive coxalgia which is exacerbated with sporting activities and some vicious positions. Activities that require extreme hip flexion such as putting on shoes and socks, sitting in a car, remaining seated for a long time or sporting activities evoke pain. The physical exam generally detects restricted range of motion, especially anterior impingement with a flexion and internal rotation, with a positive “impingement test”. Impingement test is pain in supine position with a 90° degree hip flexion, internal rotation, and passive abduction [1]. Passive flexion is usually lower than 105°, concentrating between 90° an 100° [1,4] and the flexion internal rotation is limited <=20° [22]. A previous history of rigidity and lack of flexibility before becoming symptomatic has been described in the group of patients’ clinical history [22], as well as an alteration of foot angle while walking [23].
The anterior-posterior pelvic x-ray is useful in the initial imaging study. In the cam type FAI, the anterior-posterior pelvic x-ray can show a protrusion at the lateral side of the femoral head-neck junction (pistol grip deformity) [3,5,24] and a triangular index higher than the femoral head ratio +2 mm [25]; while for the pincer impingement, depending on its origin, a center-edge angle >=40° can be found, 0° or negative acetabular index, decreased extrusion index, focal acetabular retroversion with cross over sign, coxa profunda or acetabular protrusion [3]. The axial projection shows better the cam-type deformity, an increased angle (42 to 55°) [3,18,26,27,28], decreased anterior offset (<8mm) or a low offset ratio (<0.18) [3]. A femoral retro torsion and coxa vara can also be observed [29]. The Dunn projection with a 45° flexion has provided to have greater sensibility to detect an increased angle [30]. The false profile radiography in the pincer impingement assessment can show a linear indentation at the femoral neck due to recurrent subluxation in advanced stages of the impingement or a decrease space between the posterior-inferior acetabulum and the posteromedial femoral head, signs of bad prognosis [3].
The CT scan gives more details regarding the bone anatomy and acetabular version, femoral head-neck junction offset, sphericity of the femoral head, articular congruence and subchondral degenerative changes such as fibrocystic lesions [4]. It is useful if coxa vara is suspected and the surgical planning of the resection, especially the femoral one [3]. The high resolution magnetic resonance and arthro-resonance provide greater detail to assess the related intra-articular lesions (of the acetabular labrum and articular cartilage) and some bone alterations [3,4,31], as a linear indentation at the femoral neck in advanced cases of pincer impingement [3]. It is also useful to discard FAI in those patients whose radiography did not show diagnostic signs [31,32].
The treatment is surgical, and can be performed in a variety of methods including surgical dislocation of the hip, hip arthroscopy with or without a limited anterior approach, limited anterior approach alone, and finally a periacetabular osteotomy when indicated [2,33,34]. It consists in improving articular congruence, stabilizing chondral and labral intra-articular lesions, relieving the patients’ symptomatology and potentially stopping its progression to articular degeneration [1,3,4,16,17]. It will be determined by the anatomical location of the lesion, related to intra-articular damage and degree of articular degeneration. In cases of advanced articular degeneration, the treatment of choice will be articular replacement with a total hip arthroplasty.
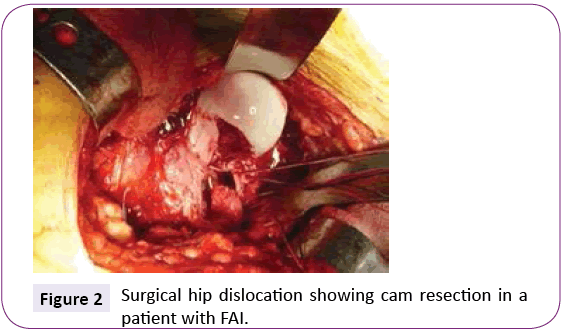
Surgical hip dislocation has been a full proven technique to treat FAI with a high success rate [2,8,35-39], allowing a direct view of the femoral and acetabular deformity, intra-articular lesions, and permits femoroplasties, acetabuloplasties and labral reinsertions with no risk of avascular necrosis [37,40].
Recently, new literature has been published about predictors of poor prognosis of surgical hip dislocation for the treatment of FAI [34,41]. Despite to this, there are little known about the factors that lead to a good functional result after the surgical treatment of this pathology, as also regarding factors of bad prognosis for medium term results of the FAI treatment.
Methods
We realized a prospective observational study in a case series of 50 hips in 44 patients with FAI, 21 female and 23 male, 6 bilateral (12%), with average age of 34.9 years (14-60). In the same hospital, all patients were operated with surgical hip dislocation by the same surgeon, between 2001-2006. Coxalgia was the main symptom in all cases. In the physical exam they all had a positive impingement test and internal rotation restriction in 90° flexion. The anterior-posterior and axial pelvic x-ray projections showed the asphericity of the femoral head; offset decrease of the femoral head-neck and focal or general acetabular over-coverage [42].
The surgical treatment was an open surgery with surgical hip dislocation [40]. A resection osteoplasty of the femoral head-neck junction was performed in all mixed and cam type impingements (Figure 1) and an acetabuloplasty was performed in all pincer and mixed type impingements [43].
Clinical, radiological, surgical and functional factors were assessed: age, symptomatology time at the consultation, impingement type (cam, pincer or mixed), degree of radiological osteoarthritis at consultation time and preservation of the acetabular labrum in the intraoperative phase.
The clinical results were determined through a survey done by an independent observer from the surgical team, which classified patients according to their symptomatology in: “asymptomatic” (patients do not have pain or discomfort in the operated hip), “better” (with a variable improvement in symptomatology, but some degree of discomfort persists) and “the same or worse” (without changes or progression of pain in the operated hip), regarding to its pre-operative status. All included patients were contacted. This subjective scale was used in the symptomatology assessment due to the fact that all existing scales at date are referred to patients with osteoarthritis and assess prosthetic results. Despite to this, all patients were examined by the surgical group and evaluated with a “modified Harris Hip Score” (HHS).
The statistical analysis was performed with an SPSS software 15.0, where p<0.05 was considered statistically significant.
Results
The average evolution time up to the moment of consultation was of 26.4 months (1 month-10 years). Radiologically, 31 hips (62%) presented coxarthrosis; 14 grade I, 9 grade II and 8 grade III, according to Tönnis scale [43]. The impingement was pincer type in 11 cases (22%), cam type in 23 cases (46%) and mixed in 16 cases (32%).
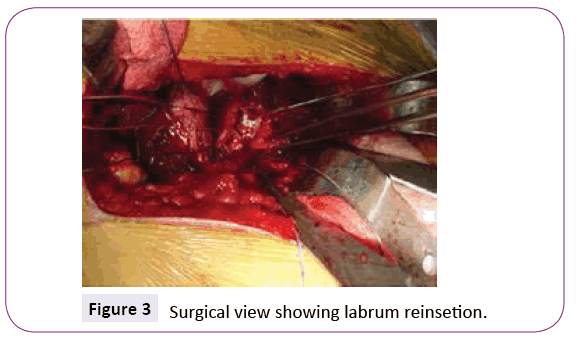
35 partial labrum resections were performed on hips with labral lesions and 2 labrum reinsertions in pincer impingement were performed on 17 years old patients (Figures 2 and 3).
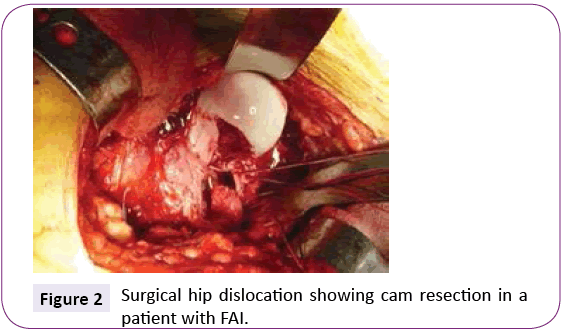
Figure 2: Surgical hip dislocation showing cam resection in a patient with FAI.
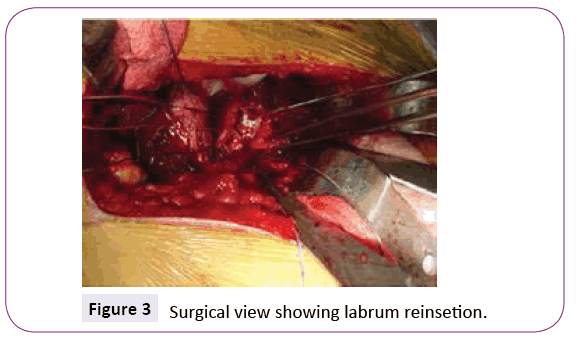
Figure 3: Surgical view showing labrum reinsetion.
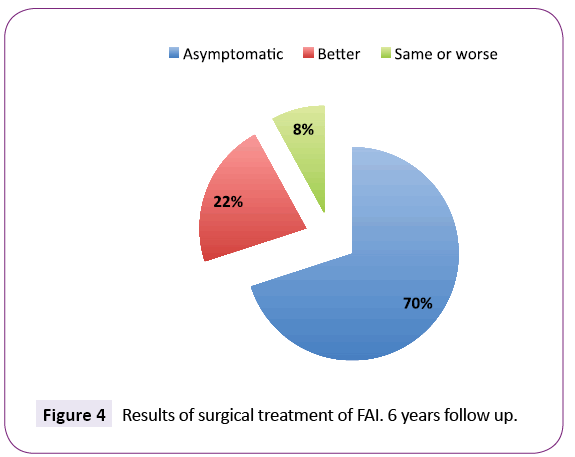
Upon assessment, after an average follow-up of 6.2 post-operative years (5-10.1), 35 hips (70%) were “asymptomatic”, 11 (22%) were “better”, and 4 (8%) were “the same or worse” (Figure 4). These subjective groups were related with HHS outcomes. Initial HHS on average was 83.76 (73-96) and the end of follow up was 96.16 (62-100). Considering patients with improvement of HHS (92% of patients) the rise was 13.04 points on average, corresponding at “asymptomatic” and “better” groups. “Asymptomatic” groups had an improvement on average of 14.2 points (85.8-100) and better group 14.09 points (80-94.09). Moreover “the same or worse” had a decrease of 8 points (76.25-68.25).
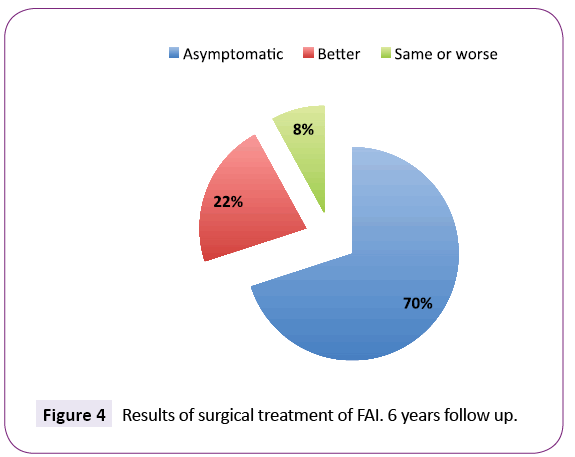
Figure 4: Results of surgical treatment of FAI. 6 years follow up.
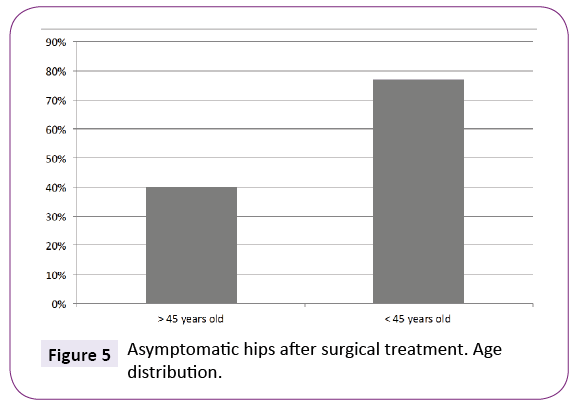
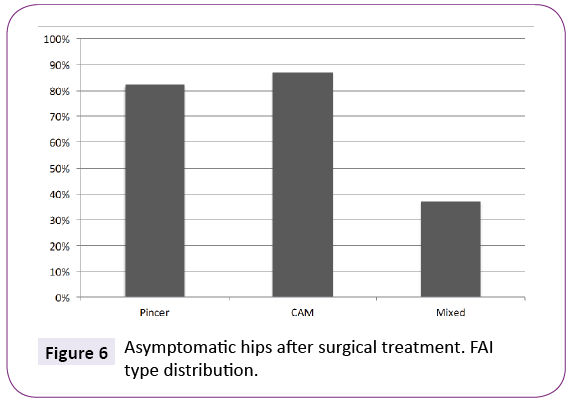
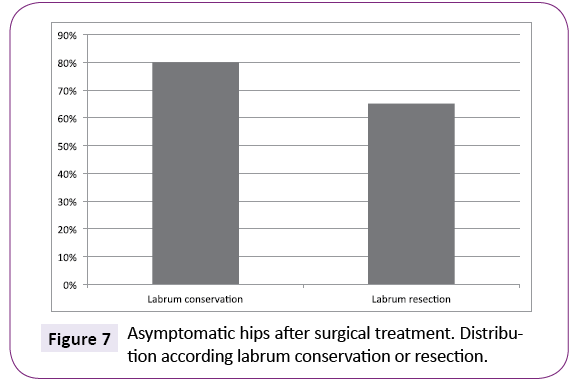
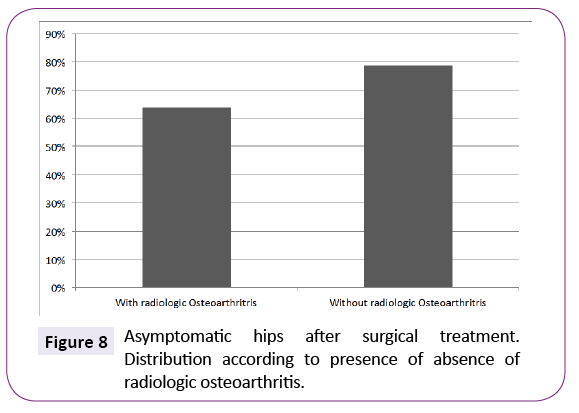
40% of the patients older than 45 were “asymptomatic” versus 77% who were less than 45 years old (P=0.03) (Figure 5). 37% of the patients with mixed impingement where “asymptomatic” versus 87% with cam impingement and 82% with pincer impingement (P=0.003) (Figure 6). In cases where the labrum was preserved, 80% became “asymptomatic” versus 65% in cases where it was resected (Figure 7). 64% of the cases that presented pre-operative radiologic osteoarthritis according to Tönnis criteria were “asymptomatic” versus 79% cases that did not have osteoarthritis (Figure 8). Extended symptomatology was related to a higher prevalence of osteoarthritis and we observed that the risk of osteoarthritis increased when the patients was older than 35 (P<0.001).
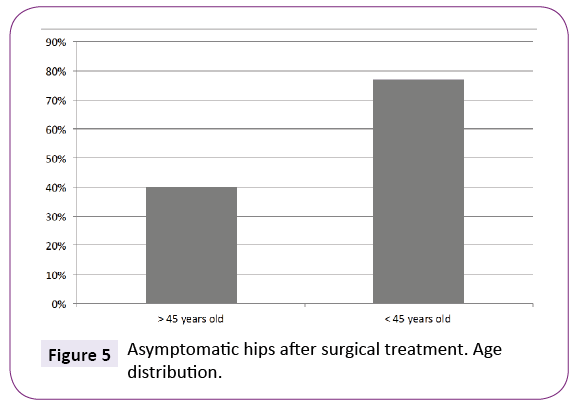
Figure 5: Asymptomatic hips after surgical treatment. Age distribution.
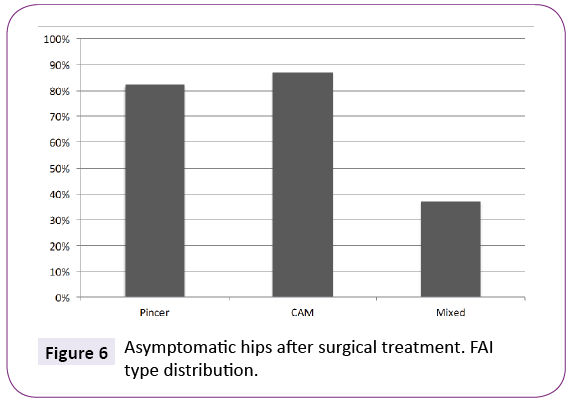
Figure 6: Asymptomatic hips after surgical treatment. FAI type distribution.
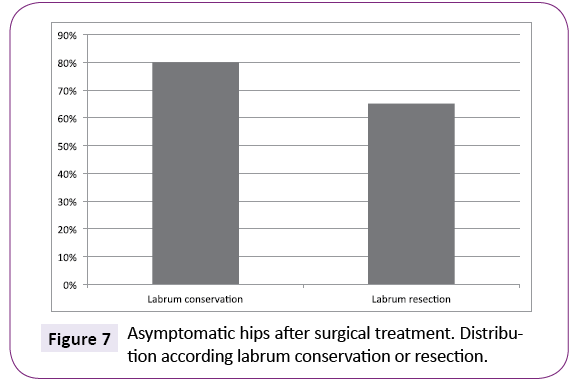
Figure 7: Asymptomatic hips after surgical treatment. Distribution according labrum conservation or resection.
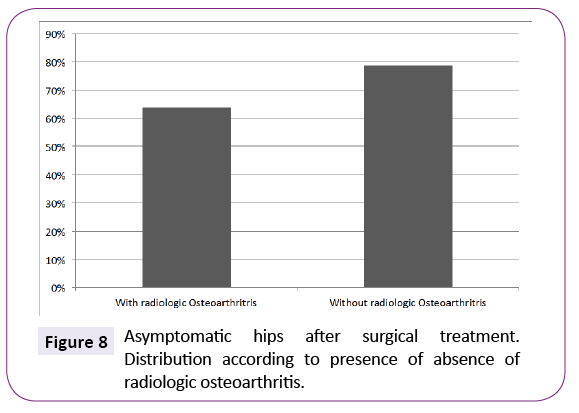
Figure 8: Asymptomatic hips after surgical treatment. Distribution according to presence of absence of radiologic osteoarthritis.
The four patients that were classified “the same or worse” had pre-operative radiologic osteoarthritis (1 G1, 2 G2, 1 G3); the labrum was resected in all of them and they all required a total hip arthroplasty at 14 month average (12-16) with an average of 43 years. Three of the four patients had mixed type impingement. The probability of require hip prosthesis in patients older than 40 was 11% versus 6% in patients younger than 40 years old (Figure 9).
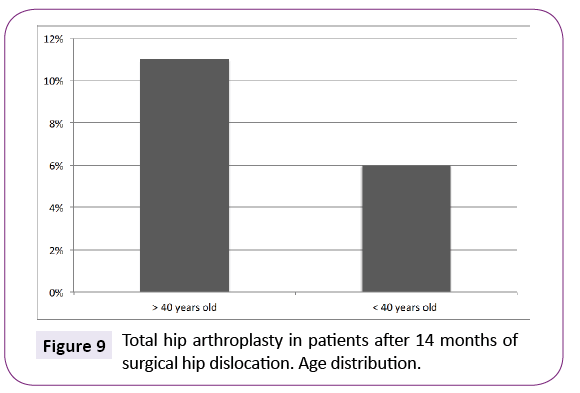
Figure 9: Total hip arthroplasty in patients after 14 months of surgical hip dislocation. Age distribution.
8 patients presented bursitis in relation to the osteosynthesis used in the greatest trochanter osteotomy, which was completely resolved by withdrawing the osteosynthesis material; 3 presented greater trochanter pseudoatrhrosis, 1 patient presented deep venous thrombosis, 1 had dislocation, and 1 had a greater trochanter fracture. There was no associated avascular necrosis or neurologic lesions.
Discussion
Surgical hip dislocation is a surgical technique that is used to treat the morphological alterations of the FAI with excellent clinical results [8,34-39,41]. However, the factors that lead to bad results in the treatment of this pathology are little known. In our work, young patients have better clinical results compared to older patients (>45 years old). This is probably because older patients are exposed longer to the aggressive mechanical factors and the damage is greater, a theory that supports what is described by Murphy et al. [8] and Beck, et al. [36]. In 2004, regarding to the better prognosis of early surgical treatment, we also observed that patients with radiologic osteoarthritis and extended symptomatology had less favorable results.
We observed that in patients younger than 40 years old, treated for FAI, the probability of requiring a total hip prosthesis at 14 months was nearly half when compared to patients older than 40 years old (6% vs. 11%). As the same as described in the literature, it increases up to 18% in patients older than 60 years old at 12 months average [45].
Greater intra-articular damage is related to mixed type impingement because it concerns the two patterns of morphologic alterations of the FAI; thus it has more related with intra-articular damage and worse results when it is compared to cam or pincer type impingement, as is shown in our statistical analysis. On the other hand, repair and preservations of the labrum has recently been proven to have better results [36]. This is coherent with our results; nevertheless these results show only a tendency and they are not statistically significant. The labrum reinsertion was performed on two 17-year old patients who were sports players. A labral disinsertion without degenerative lesions was observed in the intraoperative phase. It is worth mentioning that these cases were operated between 2001 and 2006 when the labral reinsertion was not a routine procedure, so we do not have sufficient number of reinsertion cases to validate the reinsertion results.
Besides, in 100% of labrum resection cases there was some degree of radiologic osteoarthritis, which is concordant with the literature, regarding to the relationship between labrum lesions and damaged cartilage [11,29], which significantly influences the prognosis [11]. Osteoarthritis diagnosis in patients undergoing FAI treatment is increased with age, so there is more probability to the need of a future prosthesis.
Whereas age and impingement type are statistically the most relevant data, it is also observed differences regarding other assessed factors that are not statistically significant. Probably, due to the number of patients who had bad results. However, there is a clear tendency to obtain worse results when there is extended symptomatology, pre-operative radiologic osteoarthritis and when the acetabular labrum is resected. These results are shown in the Figure 10.
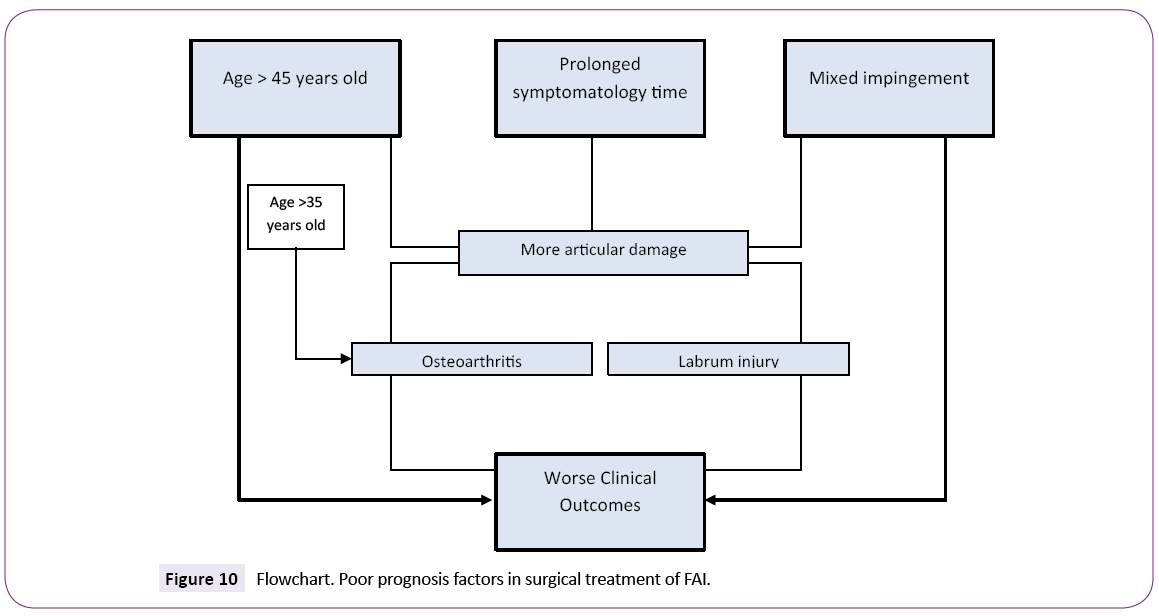
Figure 10: Flowchart. Poor prognosis factors in surgical treatment of FAI.
Conclusion
Patients with FAI treated with surgical hip dislocation achieve an excellent clinical medium term results. Significant statistic factors related to a poor prognosis are as follows: age >45 and mixed type impingement; and in the other hand, radiologic osteoarthritis, lesion and labrum resection, and prolonged symptomatology are related to bad results, tough without statistical significance.
Disclosure
There are not conflicts of interest.
8015
References
- Ganz R, Parvizi J, Beck M, Notzli H, Siebenrock KA (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 417: 112-120.
- Ross JR, Schoenecker PL, Clohisy JC (2013) Surgical dislocation of the hip: evolving indications. HSS J9:60-69.
- Tannast M, Siebernock KA, Anderson SE (2007) Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol 188: 1540-1552.
- Zebala LP, Schoenecker PL, Clohisy JC (2007) Anterior femoroacetabular impingement: a diverse disease with evolving treatment options. Iowa Orthop J27: 71-81.
- Siebenrock KA, Wahab KH, Werlen S, Kalhor M, Leunig M, et al. (2004) Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Ortho Relat Res 418: 54-60.
- Tschauner C, Fock CM, Hofmann S, Raith J (2002) Rotational abnormalities of the hip joint. Radiologe 42: 457-466.
- Strehl A, Ganz R (2005) Anterior femoroacetabular impingement after healed femoral neck fractures. Unfallchirurg 108: 263-273.
- Murphy S, Tannast M, Kim YJ, Buly R, Millins MB (2004) Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Ortho Relat Res 429: 178-181.
- Snow SW, Keret D, Scarangella S, Bowen JR (1993) Anterior impingement of the femoral head: a late phenomenon of Legg Calve-Perthes’ disease. J Pediatr Orthop13: 286-289.
- Leunig M, Casillas MM, Hamlet M, Hersche O, Notzli H, et al. (2000) Slipped capital femoral epiphysis; early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand 71: 370-375.
- Goodman DA, Feighan JE, Smith AD, Latimer B, Buly RL, et al. (1997) Subclinical slipped capital femoral epiphysis. Relationship to osteoarthrosis of the hip. J Bone Joint Surg Am 79: 1489-1497.
- Leuning M, Frautzl XR, Ganz R (2002) [Early damage to the acetabular cartilage in slipped capital femoral epiphysis. Therapeutic consequences]. Orthopade31: 894-899.
- Beck M, Kalhor M, Leunig M, Ganz R (2005) Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Surg Br87: 1012-1018.
- Khanduja V, Villar RN (2007) The arthroscopic management of femoroacetabular impingement. Knee Surg Sports Traumatol Arthros15: 1035-1040.
- Allen D, Beaule PE, Ramadan O, Doucette S (2009) Prevalence of associated deformities and hip pain in patients with came-type femoroacetabular impingement. J Bone Surg Br91: 589-594.
- Lavinge M, Parvizi J, Beck M, Siebenrock KA, Ganz R, et al. (2004) Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res 429: 61-66.
- Laude F, Boyer T, Nogier A (2007) Anterior femoroacetabular impingement. Joint Bone Spine74: 127-132.
- Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, et al. (2006) Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology240: 778-785.
- Leunig M, Ganz R (2005) Femoroacetabular impingement. A common cause of hip complaints leading to arthrosis. Unfallchirurg 108: 9-10.
- Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, et al. (2002) The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 84: 556-560.
- Hack K, Di Primio G, Rakhra K, Beaule PE (2010) Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am 92: 2436-2444.
- Wyss T, Clark JM, Weishaupt D, Notzli HP (2007) Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res460: 152-158.
- Sierra RJ, Trousdale RT, Ganz R, Leunig M (2008) Hip disease in the young, active patient: evaluation and nonarthroplasty surgical options. J Am Acad Orthop Surg 16: 689-703.
- Stulberg SD (1975) Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: Cordell LD, Harris WH, Ramsey PL, MacEwen GD(eds.)The Hip: Proceedings of the Third Open ScientificMeeting of the Hip Society. St Louis, MO: CV Mosby 1975:212–228.
- Gosvig KK, Jacobsen S, Palm H, Sonne-Holm S, Magnusson E (2007) A new radiological index for assessing asphericity of the femoral head in cam impingement. J Bone Joint Surg Br 89:1309-1316.
- Neumann M, Cui Q, Siebernrock KA, Beck M (2009) Impingement-free hip motion: the “normal” angle alpha after osteochondroplasty. Clin Orthop Relat Res 467:699-703.
- Millis M, Kim Y, Kocher M (2004) Hip joint-preserving surgery for the mature hip: the Children’s Hospital experience. Orthopedic Journal at Harvard Medical School 6:84-87.
- Meyer DC, Beck M, Ellis T, Ganz R, Leunig M (2006) Comparison of six radiographic projections to asses femoral head/neck asphericity. Clin Orthop Relat Res 445:181-185.
- Fadul DA, Carrino JA (2009) Imaging of femoroacetabular impingement. J Bone Joint Surg Am 91:138-143.
- Dudda M, Albers C, Mamisch TC, Werlen S, Beck M (2009) Do normal radiographs exclude asphericity of the femoral head-neck junction? Clin Orthop Relat Res 467:651-659.
- Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, et al. (2001) Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 83:1119-1124.
- Hartmann A, Gunther KP (2009) Arthroscopically assisted anterior decompression for femoroacetabular impingement: technique and early clinical results. Arch Orthop Trauma Surg 129:1001-1009.
- Siebenrock KA, Schoeninger R, Ganz R (2003) Anterior femoroacetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am 85:278-286.
- Beaule PE, Le Duff MJ, Zaragoza E (2007) Quality of life following femoral head-neck osteochndroplasty for femoroacetabular impingement. J Bone Joint Surg Am 89:773-779.
- Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, et al. (2004) Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res 2004:67-73.
- Espinosa N, Rothenfluh DA, Becj M, Ganz R, Leunig (2006) Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am 88:925-935.
- Jager M, Wild A, Westhoff B, Krauspe R (2004) Femoroacetabular impingement caused by a femoral osseus head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci 9:256-263.
- Tanzer M, Noiseux N (2004) Osseus abnormalities and early osteoarthritis: the role of hip impingement. Clint Orthop Relat Res 2004:170-177.
- Kili S, Wright I, Jones RS (2003) Change in Harris hip score in patients on the waiting list for total hip replacement. Ann R Coll Surg Eng l85:269-271.
- Tonnis D (1976) Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res 1976:39-47.
- Javed A, O’Donnell JM (2011) Arthroscopic femoral osteochondroplasty for cam femoroacetabular impingement in patients over 60 years of age. J Bone Joint Surg Br93:326-331.
- Frank JM, Harris JD, Erickson BJ, Slikker W 3rd, Bush-Joseph CA, et al. (2015) Prevalence of Femoroacetabular Impingement Imaging Findings in Asymptomatic Volunteers: A systematic review. Arthroscopy31:1199-1204.
- Hellman MD, Riff AJ, Frank RM, Haughom BD, Nho SJ (2014) Operative treatment of femoroacetabular impingement. Phys Sportsmed 42:112-119.
- Steppacher S, Anwander H, Zurmühle C, Tannast M, Siebenrock K (2015) Eighty percent of patients with surgical hip dislocation for femoroacetabular impingement have good clinical result without osteoarthritis progression at 10 years. Clin Orthop Relat Res 473:1333-1334.
- Steppacher S, Huemmer C, Schwab JM, Tannast M, Siebenrock KA (2014) Surgical hip dislocation for treatment of femoroacetabular impingement: Factors predicting 5-year survivorship 472:337-348.