Cláudio Couto Lóssio Neto1, Érica Bantim Felício Calou1, Matheus Freitas de Almeida1, Jairo Fernandes Frutuoso1, Luana Lóssio Carvalho2, Irma Bantim Felício Calou3, Ítalo Wanderson de Moura Gabriel3 and Modesto Leite Rolim Neto4*
1Department of General Surgery, The Federal University of Cariri – UFCA, Barbalha, Ceará, Brazil
2Faculty of Medicine, Juazeiro do Norte, Ceara, Brazil
3Leão Sampaio University - UNILEÃO, Juazeiro do Norte, Ceará, Brazil
4School of Medicine, Universidade Federal do Cariri (UFCA), Rua Divino Salvador, Rosário, Barbalha, Ceará, Brazil
- *Corresponding Author:
- Modesto Leite Rolim Neto
School of Medicine
Universidade Federal do Cariri (UFCA)
Rua Divino Salvador, 284, Rosário
Barbalha, Ceará 63180000, Brazil
Tel: +55 88999042979
E-mail: modesto.neto@ufca.edu.br
Received Date: July 22, 2020; Accepted Date: July 31, 2020; Published Date: August 07, 2020
Citation: Lóssio Neto CC, Felício Calou EB, Freitas de MA, Frutuoso JF, Carvalho LL, et al. (2020) Post-Trauma Testicular Ectopia in the Scrotal Region: A Case Report. Arch Med Vol. 12 Iss.5: 25. DOI: 10.36648/1989-5216.12.5.326
Copyright: © 2020 Lóssio Neto CC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Cryptorchidism; Trauma; Testicular dislocation
Introduction
The cryptorchidism is defined as the absence of at least one testicle outside their usual anatomical location, being more frequent in child age [1]. It is considered the most frequent congenital urological malformation in males, affecting about 3% of newborns born full term [2]. In the minority of cases, cryptorchidism can be diagnosed outside the child age, being characterized as acquired cryptorchidism - which can also be described as testicular dislocation or ectopic testis - which occurs mainly due to trauma to the scrotal area [3].
In most cases, the trauma promotes a direct external pressure in the perineum by moving the testis to the soft tissue surrounding, typically, the groin. The main component that promotes this mechanism of injury is the motorcycle accident, which can happen resulting from direct collision against the handlebars or because of the trauma of the impact against the gasoline tank [4,5].
It is worth noting that testicular dislocation in most cases occurs at the time of trauma; however, there are reports that indicate a late onset of dislocation weeks after the trauma [6]. In addition, 90% of displacement cases are unilateral; 50% are identified in the superficial inguinal area, 18% in the pubic region, 8% canalicular, 8% penile, 6% intra-abdominal, 4% perineal and 2% crural region [6,7].
Case Report
A patient C.D.F.M, 24-years-old, male, motorcyclist, with a history of trauma, side-by-side motorcycle-car collision, occurred on 8/3/2019 at 5 pm.
He attended the Regional Hospital of Cariri (HRC) the next day (8/4/2019) with a hematoma and pain in the scrotal and right inguinal areas, without other significant post-traumatic injuries. A scrotal ultrasound was then performed, in which the following result was identified: topical and homogeneous testicles with normal contours and dimensions; small amount of anechoic free fluid with slight permeable debris in both hemiscrotum; edematous infiltration involving both hemiscrotum associated with thick heterogeneous areas adjacent to the testicles, which can translate hematomas.
In view of the case and after analyzing the imaging exams aforementioned, a right inguinal hematoma drainage procedure was performed. Then, the patient was discharged with improvement of the condition.
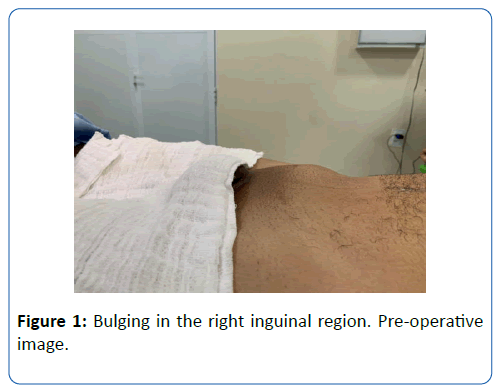
The patient remained asymptomatic. However, he noticed, after weeks, the appearance of right inguinal bulge associated with the absence of the testis in the hemiscrotum. He underwent a new ultrasound of the scrotum (9/27/2019), presenting the following result: right testicle projecting into the right inguinal canal, measuring 4.5 × 1.4 cm, evidenced by Doppler, pampiniform plexus veins with flow and without ectasias. There is also symmetrical uptake of bilateral intratesticular vessel flow. In possession of the ultrasound scans, the patient sought care at the surgery clinic of general hospital of brejo santo. During physical evaluation, there was an absence of testicle in the right scrotum and bulge in an elliptical shape of approximately 5 centimeters in the ipsilateral inguinal region, of fibroelastic consistency, painless to palpation and immobile. He affirmed to be convinced of the pre-existence of the right testicle in the scrotum before the incident.
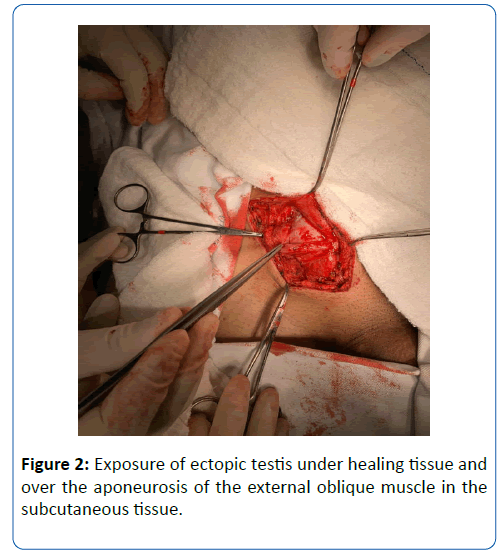
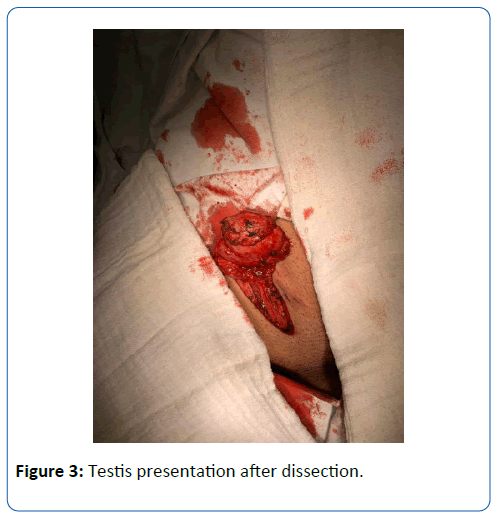
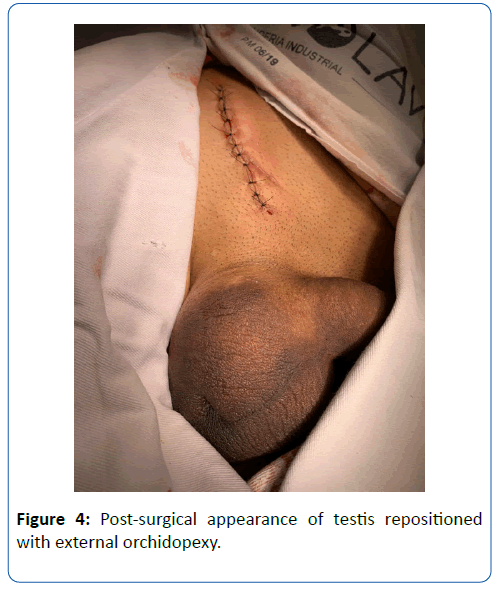
He underwent an elective surgical procedure, orchidopexy, on 10/10/19 (Figures 1-4).
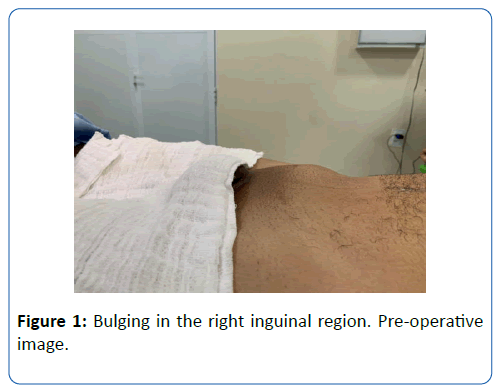
Figure 1: Bulging in the right inguinal region. Pre-operative image.
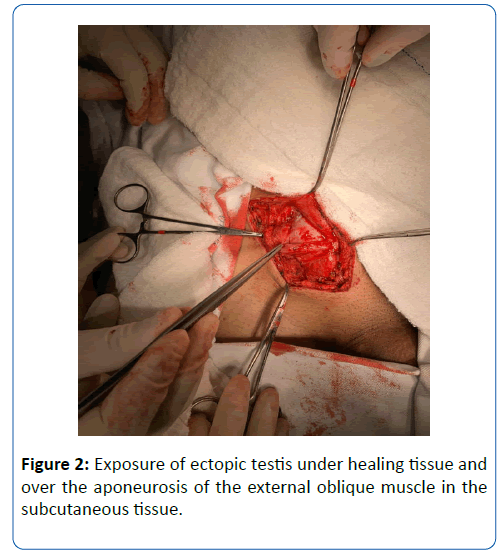
Figure 2: Exposure of ectopic testis under healing tissue and over the aponeurosis of the external oblique muscle in the subcutaneous tissue.
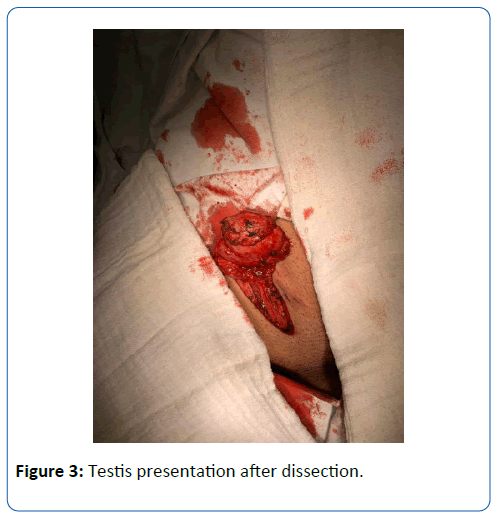
Figure 3: Testis presentation after dissection.
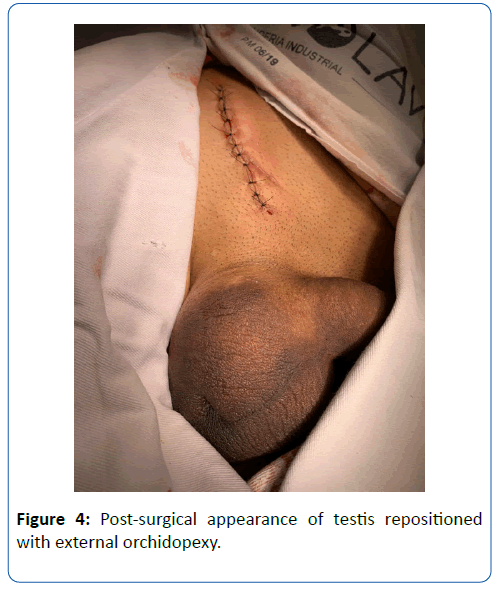
Figure 4: Post-surgical appearance of testis repositioned with external orchidopexy.
The patient evolved in the postoperative period with good general condition, clear diuresis and no evidence of hematoma at the surgical site, being discharged from the hospital.
He returned on 10/25/2019 for revaluation, asymptomatic with surgical wound without phlogistic signs and topical right testicle.
Discussion
The cryptorchidism acquired is considered a rare consequence resulting from trauma to the scrotum. The trauma mechanism results from trauma in the perineum region or happens due to the formation of a pressure force that happens between the perineum and the motorcycle tank [8].
Although most cases of testicular dislocation occurs at the time of trauma [9], there are also records of his development in a period of days or even weeks after the injury, as described in this case. The diagnosis of cryptorchidism is known to be clinical, but the solicitation of complementary exams is used to detect the location of the testicles, as well as for identification of complications, feasibility and vascularization assessment, and therapeutic control, or in situations where, on the physical examination, the testicles are not palpable. In this context, ultrasonography stands out, since, in addition to the aforementioned advantages, this exam has an excellent cost/ benefit ratio.
It is noteworthy that, despite being a rare condition, the condition may progress to various complications, especially, when there is delay in treatment. Possible complications include: testicular torsion, diffuse atrophy of seminiferous tubules [10], major impairment of spermatogenesis [11], and acute or chronic pain, directly interfering with daily activities [12]. It is known, however, that several reports have shown that, once treated, the recovery of endocrine and fertility functions are excellent [7,13], and thus the early treatment is essential in order to avoid sequelae.
In the acute phase after trauma, non-surgical treatment can be performed, in some cases, through reduction by manual traction, yet only 15% of non-surgical treatment showed satisfactory results.
In contrast, the surgical treatment - orchidopexy - has the best results, especially when performed early. It consists of inguinal or testicular high intervention for both palpable or not palpable testicle [14,15]. Its advantages includes lower risk of chronic complications and reduced risk of rupture or twist during manual traction. It can also be performed belatedly, with no existent reports in the literature of approach after five months of the trauma [16].
Conclusion
In this context, it is fundamental the need for an evaluation and careful reassessment in multiple trauma patients in the emergency, specially, after motorcycle accidents, in order to carry out the diagnosis of acquired cryptorchidism, enabling, thus, the early surgical approach, orchidopexy, which is considered the procedure with the best outcomes, preventing, thus, the occurrence of complications.
32312
References
- Faria EF, Freitas CH (2010) Urologia Fundamental. São Paulo: Editora Planmark p: 180.
- Garrone G, Liguore R (2010) Urologia Fundamental. São Paulo: Editora Planmark p: 384.
- SILVA, Samira S (2019) Criptorquidia bilateral pós-traumática: um relato de caso. Pinheiro. Monografia. Universidade Federal do Maranhão.
- Barufaldi F, Canuto Pereira G, Fabiano Docussé J, Saber G, Pereira de Azevedo B, et al. (2017) Criptorquidismo adquirido por traumatismo escrotal: relato de caso. Revista Relato de Casos do CBC 1: 1-3.
- De Sousa Oliveira Filho G, Silva Oliveira LC, Gonçalves Da Justa D (2000)Traumatic Testicular Dislocation. Braz J Urol 26: 528-529.
- Perera E, Bhatt S, Vikram SD (2011) Traumatic ectopic dislocation of testis. J Clin Imaging Sci 1: 17.
- Muhammad ZA, Thwaini T, Subramaniam KS (2009) Testicular dislocation: a rare consequence of blunt scrotal injury. Can Urol Assoc J 3: E1.
- Carvalho N, Ximenes Marques AC, Victor L, De Souz T, Soares G, et al. (2018) Bilateral traumatic testicular dislocation. Case Rep Urol.
- Madden JF (1994) Closed reduction of a traumatically dislocated testicle. Acad Emerg Med 1: 272-275.
- Hayami S, Ishigooka M, Suzuki Y, Sasagawa I, Nakada T, et al. (1996) Pathological changes of traumatic dislocated testis. Urol Int 56: 129-132.
- Aleya EP (1929) Dislocation of the testis. Surg Gynecol Obstet 49: 600-616.
- Alonso AR, García PD, Calvo OA (2000) [Bilateral testicular luxation][article in Spanish] Actas Urol Esp 24: 58-56.
- Gapany C, Frey P, Cachat F, Gudinchet F, Jichlinski P, et al. (2008) Management of cryptorchidism in children: guidelines. Swiss Med Wkly 138: 492-498.
- Zavras N, Siatelis A, Misiakos E, Bagias G, Papachristos V, et al. (2014) Testicular dislocation after scrotal trauma: A case report and brief literature review. Urol Case Rep 2: 101-104.