Peri-Procedural, Non-Invasive Hemodynamic Monitoring In TAVI-Patients: Potential Impact on Patient Selection and Outcome Prediction
Keywords
Transcatheter Aortic Valve Implantation (TAVI); Aortic Valve Stenosis (AS), Non-invasive whole body electrical bio-impedance measurements; NICaS®; In-hospital hemodynamic outcomes
Abbreviations
AS: Aortic Valve Stenosis; ANOVA: Analysis Of Variance; BI: Basal Impedance; BP: Blood Pressure; CE: Conformité Européenne; CI: Cardiac Index; CO: Cardiac Output; CPI: Cardiac Power Index; FDA: Food And Drug Administration; GGI: Granov Goor Index; HR: Heart Rate; ICU: Intensive Care Unit; LOS: Length Of Stay; LVEF: Left Ventricular Ejection Fraction; RAAS: Renin Angiotensin Aldosterone System; RR: Respiration Rate; SI: Stroke Index; STI: Systolic Time Intervals; STS: Society of Thoracic Surgeons; SV: Stroke Volume; TAVI: Transcatheter Aortic Valve Implantation; TPR: Total Peripheral Resistance; TPRI: Total Peripheral Resistance Index
Introduction
Aortic Valve Stenosis (AS) as one of the most frequent acquired valvular heart disease represents a major health problem with an appalling annual death particularly in the growing population of elderly patients [1]. With the advent of percutaneous, transcatheter aortic valve implantation (TAVI), the technology is particularly appealing to AS patients with advanced age and comorbidities whose outcome depends on less invasive surgical access and avoidance of mechanical ventilation as well as the use of cardioplegia and heart-lungmachine [2]. Although beneficial short and long term outcome is proven for transfemoral TAVI throughout the whole specter of transcatheter valve deploying systems, little is known about immediate and post-procedural short term hemodynamic changes compared to patients´ baseline status. This depends on the need of additional- predominantly invasive-hemodynamic measurement tools such as Swan-Ganz® or PICCO® catheterisation systems. Therefore, most of these data is missing or available only from baseline right heart catheterization [3]. Such an information regarding baseline hemodynamics and its changes after procedure may give important information on procedural timing and short-term outcomes. Moreover, these parameters may offer an accurate tool for tailored peri and post procedural in-hospital management and for discharge planning.
The NICaS® whole body electrical bio-impedance monitoring system provides an accurate and approved method to obtain hemodynamic parameters in an easy non-invasive manner and that can be used bedside at any time for repeated measurements [4,5]. The present series aim to report on feasibility and reproducibility of these measurements to illustrate short-term in-hospital hemodynamic outcomes in unselected patients subjected to transfemoral TAVI.
Methods
Patients
Over a period of 8 months, 52 unselected patients with severe symptomatic AS were scheduled to TAVI procedure after heartteam decision at the Universtity Heart Center of the University Hospital Marburg. Endovascular TAVI was applied in local anaesthesia and analgosedation without mechanical ventilation in all patients using the Medtronic Evolut R® (n=32), Edwards Sapien 3® (n=14) or Boston Scientific SYMETIS ACURATE neoTM TF® (n=4) system. All comers were measured with the NICaS® whole body electrical bioimpedance monitoring system at baseline at the day before TAVI. Measurements were repeated after six to eight hours at the same day of TAVI procedure at the cardiology intensive care unit (ICU) while all patients were free of inotropics vasopressors or sedatives. A second in-hospital follow-up was performed at the day of discharge [mean hospital length of stay (LOS) 6.2 ± 1.1 days].
One patient died at the beginning of TAVI procedure due to low-output heart failure and electro-mechanic dissociation before passing the aortic valve with guide-wire and was excluded from analysis. Thus, 51 patients left to be retrospectively analysed for hemodynamic outcomes at the day of procedure and before discharge.
NICaS® device and procedure
The NICaS® whole body electrical bio-impedance monitoring system (NIMedical, Israel Advanced Technology Industries, Hertzliya Pituach 4676672, Israel) is a FDA and European CE-sign approved non-invasive hemodynamic monitoring tool. Using a combination of pulse contour analysis and the Granov Goor Index (GGI) based on the systolic time intervals (STI) which similarly to left ventricular ejection fraction (LVEF)-can assess cardiac function and provide information on several circulatory parameters and volume status. The technology underwent several validation studies compared to Swan-Ganz- and PICCO®- catheterisation techniques [4-8].
For each measurement, self-adhesive electrodes were placed either on the left or right wrist and the left or right ankle to achieve whole body impedance measurements. Current patients ´ weight systolic and diastolic blood pressure (BP), haematocrit, sodium and peripheral oxygen saturation were actualized to be inserted in NICaS® for each measurement. Measurements were performed in supine position after five minutes at rest. Each patient was measured by at least two independent investigators blinded for either baseline or follow-up results. It was warranted, that electrodes were placed at the same wrist and ankle for each patient at baseline and for the two follow-up time points. At least four consecutive measurements were carried out to achieve valuable results for each time point (mean number consecutive measurements for baseline 4.6 ± 0.2 after procedure 3.9 ± 0.7 and before discharge 4.1 ± 1.1). Outliers within the consecutive measurements >20% were eliminated to achieve accurate means (4.3% of all measurements).
Study objectives
The purpose of this investigation is to illustrate short-term inhospital hemodynamic changes in TAVI patients by repeated bedside non-invasive monitoring otherwise only obtainable by invasive methods and currently only reported for baseline characteristics of selected TAVI patients by Swan-Ganz- Catheterisation [3]. Primary goal was to confirm adaptive mechanisms of hemodynamic improvement up to discharge and to deduce management criteria for potential peri- and postprocedural benefit.
Statistical analysis
Categorical variables are presented as counts and percentages. Continuous variables following a normal distribution are presented as mean+standard deviation and were compared using unpaired student ’ s t-test. Continuous variables were assessed for normal distribution with the Anderson-Darling test. Data were analysed by one way ANOVA for comparison across multiple groups processing the data by the SPSS (version 15, SPSS Inc., Chicago, IL, USA) software package. All tests were performed two-sided and p values <0.05 were considered as statistically significant.
Results
Clinical characteristics
Patients’ baseline characteristics with regard to age, gender, body-mass-index and echocardiographic parameters are summarized in Table 1.
| Patients scheduled to TAVI procedure |
| Subjects (n) |
51 (100 %) |
| Male/female |
28 (53.3%)/23 (46.6%) |
| Age |
84.3 ± 4.1 |
| Body mass index (kg/m2) |
28.1 ± 5.7 |
| Functional NYHA Class |
| NYHA Class I |
2 (3.9%) |
| NYHA Class II |
10 (19.6%) |
| NYHA Class III |
35 (68.6%) |
| NYHA Class IV |
4 (7.8%) |
| Angina |
21 (41.2%) |
| Syncope |
10 (19.6%) |
| Echocardiographic values |
| LVEF (%) |
41.6 ± 6.8 |
| AV velocity max (cm/sec) |
398.2 ± 65.1 |
| AV gradient max (mmHg) |
67.5 ± 19.2 |
| AV gradient mean (mmHg) |
36.9 ± 11.8 |
| AV opening area (cm2) |
0.81 ± 0.11 |
Table 1 Characteristics of study subjects.
Mean ICU-LOS was 1.8 ± 0.8 days and mean hospital LOS was 6.2 ± 1.1 days. No patient reported neurological symptoms or signs of peripheral arterial malperfusion after procedure. There were no cases of access site bleeding. Transthoracic echocardiography (TTE) and vascular ultrasound was performed on all patients before discharge despite of cardiac symptoms or inconspicuous post-procedural access site. In no patient, more than of first degree residual aortic valve prosthesis regurgitation was detectable while mild regurgitation (I°) was observed only in 8 of the 51 patients (15.7%). Arteriovenous fistulas aneurysms or local dissection could be excluded by vascular Doppler interrogation prior to discharge. No significant changes were observed in serum electrolytes, parameters of renal function, haemoglobin or leukocyte counts between baseline and the day of discharge.
There were no significant changes detectable for resting heart rate (HR), resting respiration rate (RR), stroke volume (SV), stroke index (SI), diastolic and mean arterial blood pressure (BP) as well as for basal impedance (BI) at discharge as compared to baseline (Table 2).
| Parameters |
Measurement changes compared to baseline |
| Baseline |
6-8 h after TAVI |
P value |
before discharge (6.2 ± 1.1 days) |
P value |
| Resting heart rate (HR); (bpm) |
75.7 ± 18.2 |
75.1 ± 16.3 |
0.789 |
77.9 ± 18.6 |
0.4745 |
| Resting respiration rate (RR); (/min) |
18.0 ± 4.4 |
18.10 ± 4.43 |
0.915 |
18.52 ± 4.87 |
0.518 |
| Stroke volume (SV); (ml) |
70.46 ± 24.45 |
63.95 ± 24.51 |
0.0199 |
76.62 ± 25.08 |
0.118 |
| Stroke index (SI), (ml/m2) |
36.81 ± 12.29 |
34.55 ± 13.78 |
0.206 |
40.87 ± 14.12 |
0.078 |
| Diastolic arterial BP; (mmHg) |
69.06 ± 9.13 |
63.40 ± 12.84 |
0.004 |
66.00 ± 11.87 |
0.162 |
| Mean arterial BP; (mmHg) |
89.21 ± 10.01 |
85.75 ± 13.65 |
0.061 |
87.58 ± 11.90 |
0.353 |
| Basal impedance (BI); (ohm) |
365.21 ± 71.90 |
375.54 ± 73.42 |
0.231 |
351.60 ± 66.81 |
0.086 |
Table 2 Parameters without significant changes at discharge as compared to baseline. (Transient significant early impact after TAVI on stroke volume (SV) and diastolic arterial blood pressure (BP) is discussed in the Results´ section).
Impact on CO, CI and CPI
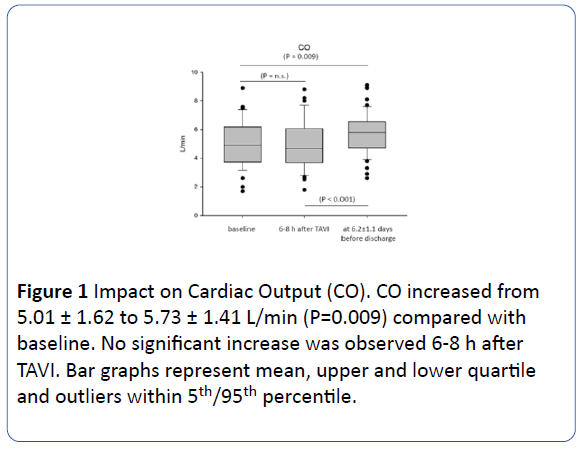
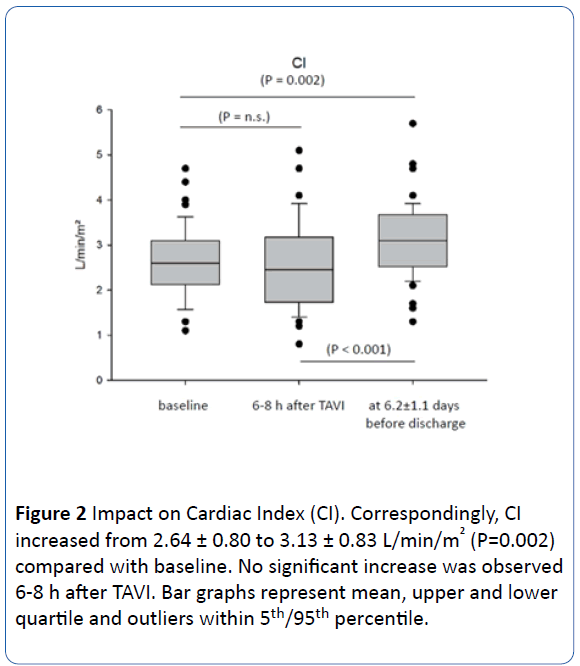
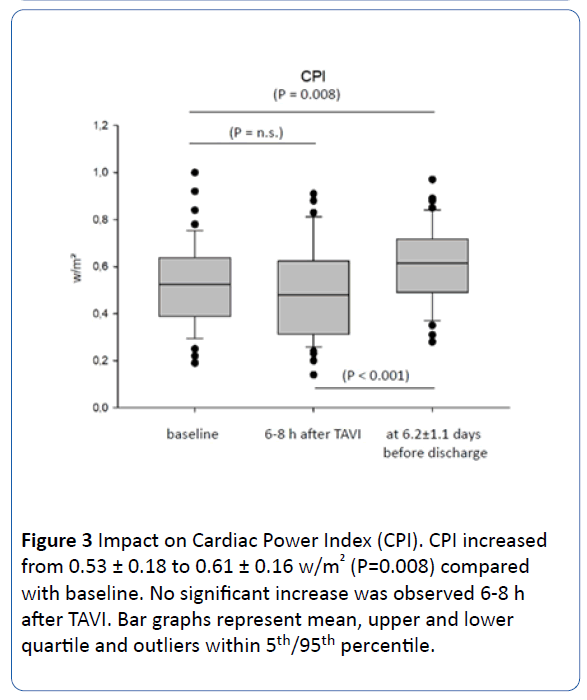
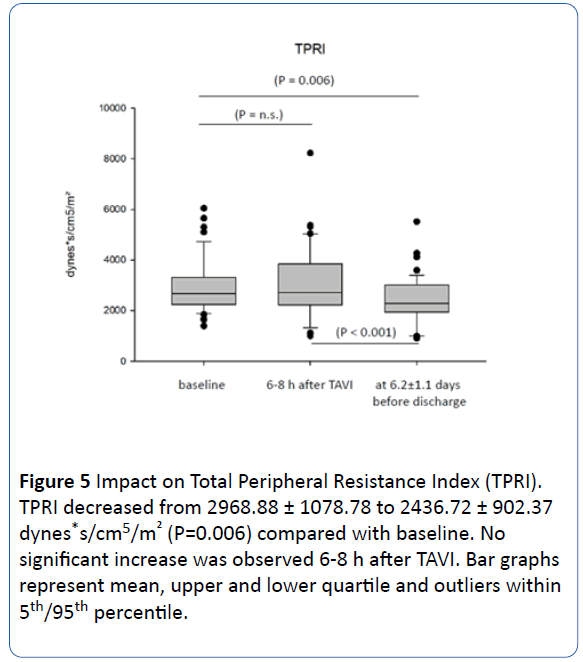
When comparing discharge to baseline, there was a successful increase in cardiac output (CO) from 5.01 ± 1.62 to 5.73 ± 1.41 L/min (P=0.009) corresponding to an cardiac index (CI) increase from 2.64 ± 0.80 to 3.13 ± 0.83 L/min/m2 (P=0.002) and of increase in cardiac power index (CPI) from 0.53 ± 0.18 to 0.61 ± 0.16 w/m2 (P=0.008) as well. Interestingly, no significant changes could be observed immediately at measurements six to eight hours after TAVI compared to baseline (Figures 1, 2 and 3).
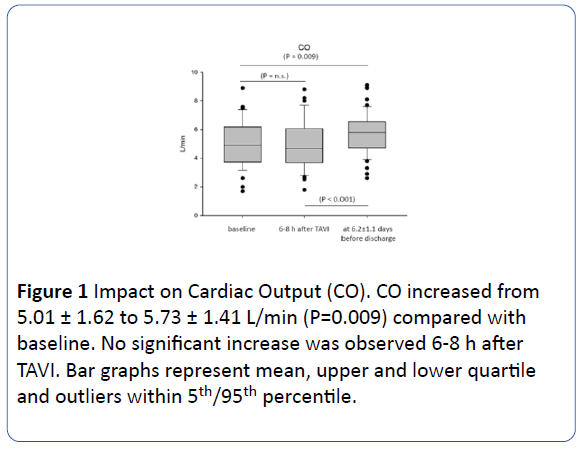
Figure 1: Impact on Cardiac Output (CO). CO increased from 5.01 ± 1.62 to 5.73 ± 1.41 L/min (P=0.009) compared with baseline. No significant increase was observed 6-8 h after TAVI. Bar graphs represent mean, upper and lower quartile and outliers within 5th/95th percentile.
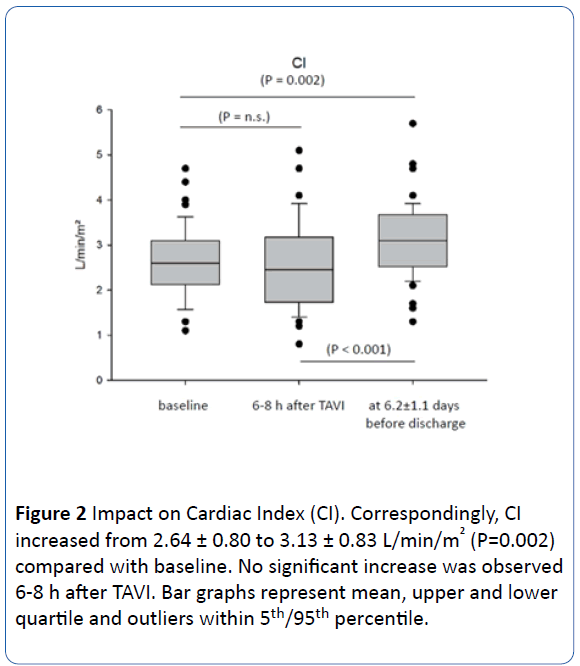
Figure 2: Impact on Cardiac Index (CI). Correspondingly, CI increased from 2.64 ± 0.80 to 3.13 ± 0.83 L/min/m2 (P=0.002) compared with baseline. No significant increase was observed 6-8 h after TAVI. Bar graphs represent mean, upper and lower quartile and outliers within 5th/95th percentile.
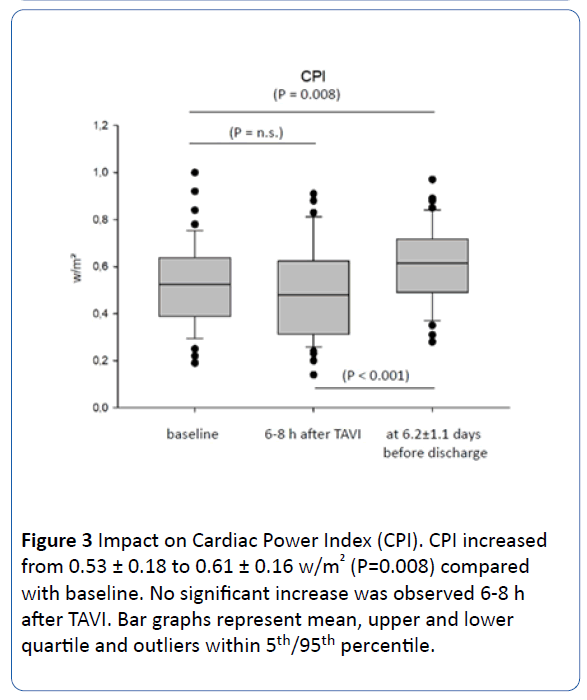
Figure 3: Impact on Cardiac Power Index (CPI). CPI increased from 0.53 ± 0.18 to 0.61 ± 0.16 w/m2 (P=0.008) compared with baseline. No significant increase was observed 6-8 h after TAVI. Bar graphs represent mean, upper and lower quartile and outliers within 5th/95th percentile.
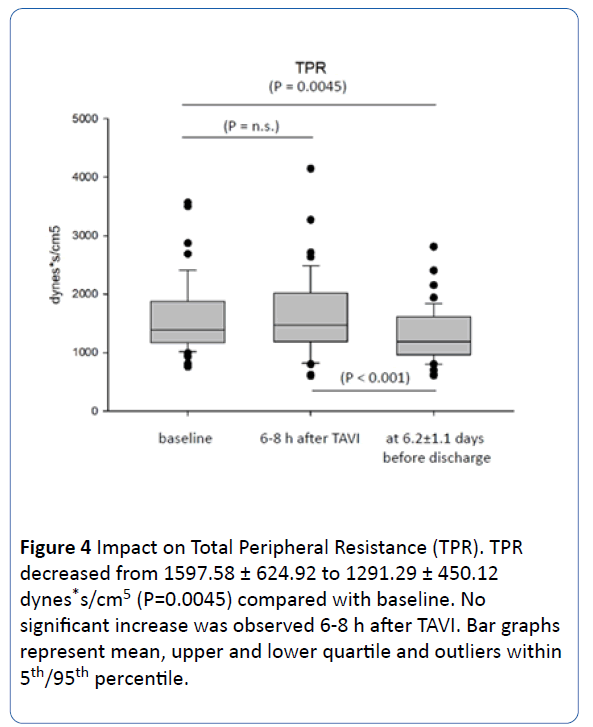
Impact on TPR and TPRI
Total peripheral resistance (TPR) significantly decrease from 1597.58 ± 624.92 to 1291.29 ± 450.12 dynes*s/cm5 (P=0.0045) corresponding to a total peripheral resistance index (TPRI) decrease from 2968.88 ± 1078.78 to 2436.72 ± 902.37 dynes*s/cm5/m2 (P=0.006) at discharge compared to baseline. Similar to CO, CI and CPI, no early changes were detectable for same day after TAVI measurements (Figures 4 and 5).
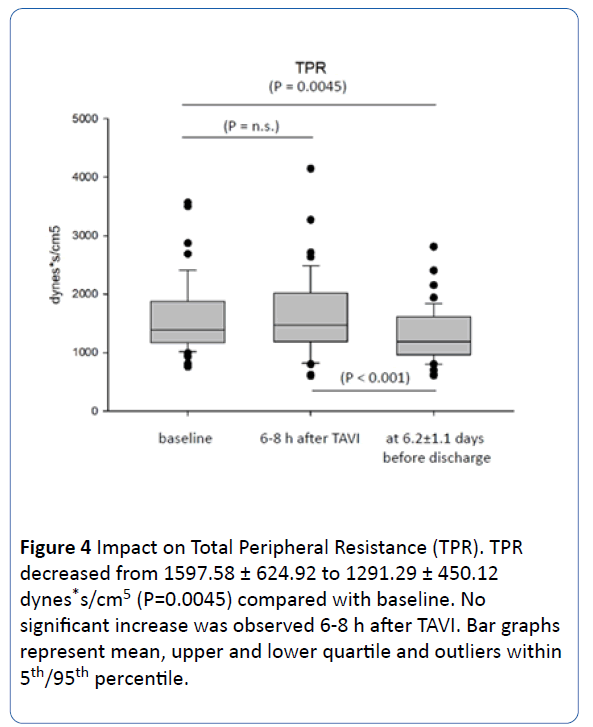
Figure 4:Impact on Total Peripheral Resistance (TPR). TPR decreased from 1597.58 ± 624.92 to 1291.29 ± 450.12 dynes*s/cm5 (P=0.0045) compared with baseline. No significant increase was observed 6-8 h after TAVI. Bar graphs represent mean, upper and lower quartile and outliers within 5th/95th percentile.
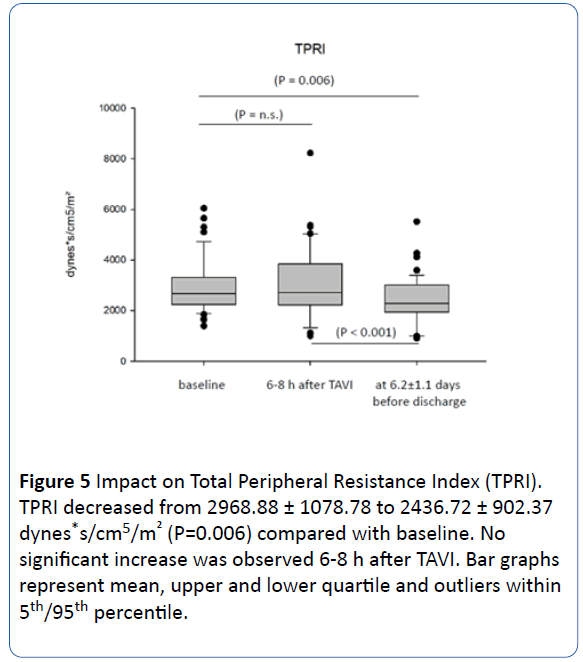
Figure 5:Impact on Total Peripheral Resistance Index (TPRI). TPRI decreased from 2968.88 ± 1078.78 to 2436.72 ± 902.37 dynes*s/cm5/m2 (P=0.006) compared with baseline. No significant increase was observed 6-8 h after TAVI. Bar graphs represent mean, upper and lower quartile and outliers within 5th/95th percentile.
Impact on systolic BP
On non-invasive BP readings, there were only significant changes in systolic values detectable at discharge. While baseline systolic BP was 130.4 ± 18.3 mmHg, there was only a mild numerical increase six to eight after TAVI (133.7 ± 22.6 mmHg) but a significant increase at discharge to 136.9 ± 19.5 mmHg (P=0.0203).
Early impact on SV, Garnov-Gor-Index and diastolic BP. Interestingly, significant decrease could be observed immediately at the same day after TAVI for these parameters. SV decreased slightly significant from 70.46 ± 24.44 to 63.95 ± 24.51 ml (P=0.019) after procedure and recovered significantly at discharge to 76.62 ± 25.08 ml (P>0.0001, when compared to six to eight hour measurements after intervention).
This did not correspond to significant changes in SI but similar effect was observed for the Garnov-Goor-Index with a decrease from 12.03 ± 4.52 to 10.69 ± 4.01 (P=0.017) and recovery to 12.46 ± 3.79 at discharge (P=0.0002). Transient more pronounced decrease of diastolic BP was observed from 69.1 ± 9.1 to 63.4 ± 12.8 mmHg (P=0.004). Values recovered at discharge to 66 ± 11.9 mmHg (P=0.007).
Discussion
Untreated severe AS leads to different deleterious changes in hemodynamics and myocardial function as a consequence of i.e., pressure overload, low-output and adaptive circulatory response. All this results in left ventricular hypertrophy, diastolic dysfunction, activation of intrinsic catecholamines and of the renin-angiotensin-aldosterone-system (RAAS) leading to subsequent impairment of LVEF and progressive organ damage in advanced stages of the disease. Symptoms of angina congestive heart failure and syncope are associated with a high mortality that approaches 50% in the first two years [1,2].
Since the landmark PARTNER-trials, TAVI emerged to become an established alternative to conventional surgery in these patients over the last decade [9,10]. Initially only applicable to individuals with high surgical risk with regard to comorbidities (i.e., STS Score >10%) and outcome, several controlled trials and registries demonstrated non-inferiority for TAVI in older patients at intermediate and low risk as well [11,12]. Nevertheless, additional tools providing information on selection criteria above established risk scores might be helpful to discriminate patients who benefit most.
The less-invasive TAVI method results in shorter ICU-LOS lower incidence of blood transfusion and reduced kidney injury early mobilization and faster hospital discharge. However, little is known about immediate in-hospital and long term hemodynamic effects in this patients´ collective.
Our present retrospective data analysis illustrates the shortterm impact of TAVI with regard to haemodynamic parameters and myocardial function immediately after treatment and before discharge compared to patients’ baseline hemodynamics. The primary objective was to get real-life hemodynamic data for the standardized approach without specific interference with the usual pre- and post-procedural treatment or in-hospital management.
Causal increase in myocardial function and proadaptive haemodynamic response is expected in TAVI but difficult to be verified more accurately because of additional need of established invasive measurement approaches. Moreover, little is known about time intervals required to observe these effects. The present results of the NICaS® measurements show a significant increase in CO, CI and CPI and a reduction in TPR and TPRI as an early positive hemodynamic response at a mean of 6.2 ± 1.1 days after procedure. These effects are not detectable as an immediately after TAVI even at a time when patients are at stabile conditions not requiring inotropic or vasopressor support at the ICU. This may result from persistent periprocedural stressors and filling status reflected in slightly diminished SV and Garnov-Goor-Index as a correlate for LV systolic function later recovering during the next few day of in-hospital stay. Thus, this parameters may be successfully used not only to illustrate hemodynamic improvement but also for discharge planning in the absence of recovery.
Detectable increase in arterial BP even up to hypertensive levels after TAVI is associated with an improved patients´ outcome [13,14]. Such a significant increase is supported by our data for systolic BP before discharge compared to baseline values. Independently, early decrease in diastolic BP may reflect transient responses to residual aortic regurgitation, volume status and/or concomitant vasodilation.
On aggregate, there is future potential to use NICaS® as an additional tool in the diagnostic armamentum for patients with TAVI. Facing the non-invasive, accurate and at any time repeatable measurements, further investigations should focus on criteria for patients selection, timing of procedure, early postprocedural management, tailored medication, discharge planning or long term ambulatory outcomes and might be of prognostic significance.
Study Limitations
Even though our observation is in line and consistent with expectable results in TAVI patients, one of our limitations is the retrospective observational design in a small cohort of patients. Therefore, larger trials are warranted in order to confirm our findings and to show whether there is prognostic relevance for patients ’ selection or differences in short and long term outcome. In addition, it would be helpful to have a more continuous follow-up period of time with repeated postprocedural measurements during in-hospital LOS to evaluate the durability of acute procedural success and patients´ outcome.
Even though investigators were blinded for either baseline or follow-up results, we cannot exclude individual bias of different time intervals prior to and after TAVI as well as before discharge for each patient and an influence of differing concomitant medication. There were few changes in baseline oral cardiovascular medication during in-hospital stay and 5 patients required application of intravenous diuretics after TAVI procedure (Table 3). Thus, this could be an influential factor on changes in hemodynamics. Nevertheless, our observation was designed to describe such changes based on established in hospital periprocedural patients´ management not guided and influenced by NICaS® measurements.
| Changes in oral medication |
| Newly prescribed oral medication |
| Beta-blockers |
n=2 (3.92%) |
| Bisoprolol |
1 (1.96%) |
| Metoprolol |
1 (1.96%) |
| Angiontensin converting enzyme antagonists |
n=3 (5.88%) |
| Ramipril |
3 (5.88%) |
| Angiotensin receptor blockers |
n=1 (1.96%) |
| Candesartan |
1 (1.96%) |
| Diuretics |
n=4 (7.84%) |
| Torasemide |
3 (5.88%) |
| Hydrochlorothiacide |
1 (1.96%) |
| Mineralocorticoid-receptor antagonists |
n=3 (5.88%) |
| Spironolactone |
2 (3.92%) |
| Eplerenone |
1(1.96%) |
| Discontinued oral medication |
| Beta-blockers |
n=4 (7.84%) |
| Bisoprolol |
3 (5.88%) |
| Nebivolol |
1 (1.96%) |
| Angiontensin converting enzyme antagonists |
n=2 (3.92%) |
| Ramipril |
1 (1.96%) |
| Lisinopril |
1 (1.96%) |
| Calcium channel blockers |
n=1 (1.96%) |
| Amlodipine |
1 (1.96%) |
| Dose modification |
| Beta-blockers |
n=5 (9.80%) |
| Bisoprolol up-titration |
2 (3.92%) |
| Bisoprolol down-titration |
1 (1.96%) |
| Nebivolol up-titration |
1 (1.96%) |
| Metoprolol down-titration |
1 (1.96%) |
| Calcium channel blockers |
n=3 (5.88%) |
| Amlodipine down-titration |
2 (3.92%) |
| Lercanidipine up-titration |
1 (1.96%) |
| Transient use of intravenous diuretics after TAVI |
| Furosemide |
n=5 (9.80%) |
(for a maximum of 3 days after TAVI) |
Table 3 Changes in cardiovascular medication during in hospital stay (n=51 Patients; 100%).
Conclusion
Non-invasive whole body electrical bio-impedance measurements with the NICaS® system represent an accurate bedside tool for monitoring immediate and short-term hemodynamic changes in unselected patients subjected to TAVI procedure. Results can be easily used for tailored periprocedural management, early patients´ mobilization and discharge planning. Future studies have to focus on improvement of clinical and prognostic parameters guided by NICaS® monitoring.
Declarations
Ethics and consent to participate
The analysis was approved by the local Ethics Committee complying with the Declaration of Helsinki, and all patients gave written informed consent to participate.
Trial Registration Number: 105/18.
Consent for publication
All patients gave written consent for anonymized data publication.
Authors’ contributions
Birgit Marcus - NICaS®-Measurements, Manuscript preparation
Konstantinos Karatolios - TAVI-procedure, Heart-teamdecision
Corinna Wulle-NICaS®-Measurements
Daniela Pethig-NICaS®-Measurements
Ardawan Rastan-Heart-team-decision, TAVI-procedure
Bernhard Schieffer-TAVI-procedure, Heart-team-decision
Dimitar Divchev-Manuscript preparation, NICaS®- measurements, TAVI-procedure, Heart-team-decision
Competing interest
None declared.
Funding
No funding was obtained for this study
Acknowledgements
Not Applicable
Data availability
Raw data of NICaS®-measurements is included as a separate Excel file.
24564
References
- Vahanian A, Alfieri O, Andreotti F (2012) Guidelines on the management of valvular heart disease (version 2012): The joint task force on the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg. 42: S1-44.
- Bonow RO, Carabello BA, Kanu C (2006) American College of Cardiology/American Heart Association Task Force on Practice Guidelines, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons. ACC/AHA 2006 Guidelines for the Management of Patients with Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 114: e84–e231.
- O'Sullivan CJ, Stortecky S, Heg D (2013) Clinical outcomes of patients with low-flow, low-gradient, severe aortic stenosis and either preserved or reduced ejection fraction undergoing transcatheter aortic valve implantation. Eur Heart J 34: 3437-3450.
- Cotter G, Moshkovitz Y, Kaluski E (2004) Accurate, noninvasive continuous monitoring of cardiac output by whole-body electrical bioimpedance. Chest 125: 1431-1440.
- Torre-Amione G, Milo O, Kaluski E (2004) Whole-body electrical bio-impendance is accurate in non-invasive determination of cardiac output: a thermodilution controlled, prospective, double blind evaluation. J Card Fail 10(4): S38-S39.
- Paredes OL, Shite J, Shinke T (2006) Impedance cardiography for cardiac output estimation: reliability of wrist-to-ankle electrode configuration. Circ J 70(9): 1164-1168.
- Tanino Y, Shite J, Paredes OL (2009) Whole body bioimpedance monitoring for outpatient chronic heart failure follow up. Circ J. 73(6): 1074-1079.
- Taniguchi Y, Emoto N, Miyagawa K (2013) Noninvasive and simple assessment of cardiac output and pulmonary vascular resistance with whole-body impedance cardiography is useful for monitoring patients with pulmonary hypertension. Circ J 77(9): 2383-2389.
- Smith CR, Leon MB, Mack MJ (2011) Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 364: 2187-2198.
- Leon MB, Smith CR, Mack M (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. NEJM 21(363): 1597-1607.
- Vendrik J, Van Kesteren F, Van Mourik MS (2018) Procedural Outcome and Midterm Survival of Lower Risk Transfemoral Transcatheter Aortic Valve Implantation Patients Treated With the SAPIEN XT or SAPIEN 3 Device. Am J Cardiol 121: 856-861.
- Waksman R, Rogers T, Torguson R (2018) Transcatheter aortic valve replacement in low-risk patients with symptomatic severe aortic stenosis. J Am Coll Cardiol 72: 2095-2105.
- Perlman GY, Loncar S, Pollak A (2013) Post-procedural hypertension following transcatheter aortic valve implantation: incidence and clinical significance. JACC Cardiovasc Interv 6: 472-478.
- Klinkhammer BJ, Dyke CM, Haldis TA. The development or worsening of hypertension after transcatheter aortic valve replacement (TAVR) improves short-term and long-term patient outcomes. Heart Asia. 2018;10(2): e010994