Key words
ABO blood group, infection, traumatic patient, Libya.
Introduction
There are many sources of infection including environmental sources, person to person, self infection, and medical or surgical procedures [1]. Hospital associated infection is an important cause of patient morbidity and death and it represents a serious and growing health problem, it is estimated that about 2 million people acquire hospital infections each year and that about 90000 of these patients die as a result of their infections [2,3]. Enterobaceriaceae, Staphylococci, Pseudomonas and Acintobactr spices are the most common pathogens associated with infection and the most common sits of infection are urinary tract, lower respiratory tract, and blood stream and wound infection [4]. Risk factors for the invasion of colonizing pathogens can be categorized into many factors including iatrogenic, organizational, the severity of illness, underlying immunocomromised state, length of stay, and susceptibility to infection such as blood group antigens [2]. The role of blood group antigens in human diseases has been debated over many years and has been implicated as at least partially, responsible for the observed distribution of the major ABO blood group antigens [5]. Many of the associations of blood group antigens with specific pathogens involve the glycosphingolipids (GSLs) belonging to the histo-blood group P1Pk and GLOB blood group systems, specifically the P and Pk blood group antigens [6]. A recent discovery implicated that the Pk blood group antigen plays a role for protection from infection with HIV-1 [7], and the increased expression of P/Gb3 histo-blood group antigen correlates to decreased HIV infection, whereas decreased or absent P/Gb3 increases HIV susceptibility [8].
There is a large number of publications attempting to correlate blood groups susceptibility to infectious diseases such as malaria parasite, Helicobacter pylori, Klebsiella and Paravirous B19, and there is evidence that blood group antigens, that found on surface of cells, can act as receptors such as (P, ABH, Lewis, MNss, Kell, Duffy etc) for many bacteria and viruses [9]. The objective of this study is to assess the prevalence of bacterial infection among patients in the trauma hospital, and to correlate the susceptibility of ABO blood groups to the isolated bacteria.
Patients and methods
166 samples for culture and sensitivity were received from the in-patients at Abosleem Traumatic Hospital and ABO group was obtained from Blood bank documented system for each patient. Culture samples included, swabs from wounds, sputum and midstream urine, were cultivated on many types of media as routine diagnostic procedure. The bacterial growth identified by Gram stain and biochemical reaction.
Results
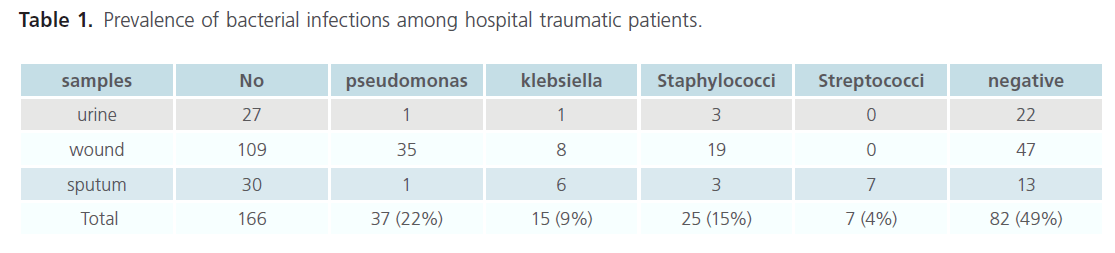
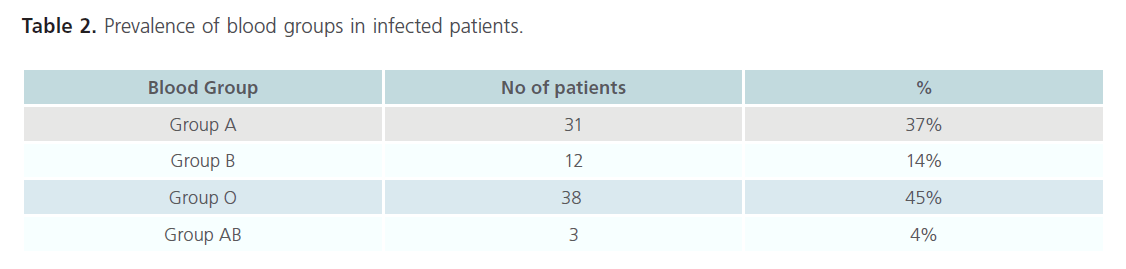
During the study 166 samples obtained from urine, wound, and sputum, 82 (49%) samples showed no growth, while 84 (51%) patients were infected during their stay in the hospital by one of the following isolates: Pseudomonas (22%); Klebsiella (9%); Staphylococci (15%); and Streptococci (4%) (Table 1). The majority of in-patients belong to blood group O (45%), preceded by group A (37%); B (14%) and AB (4%) (Table 2).
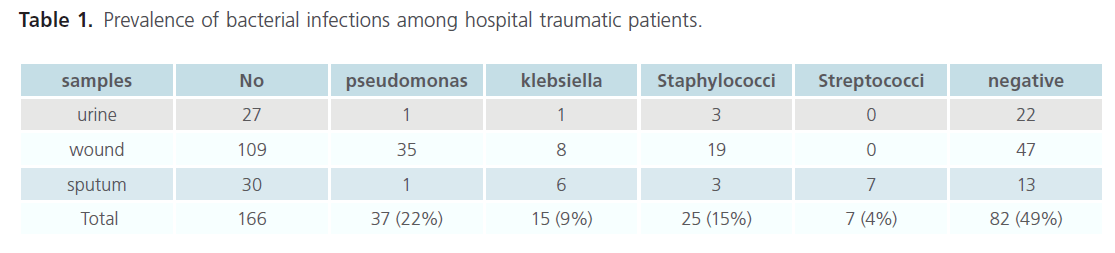
Table 1. Prevalence of bacterial infections among hospital traumatic patients.
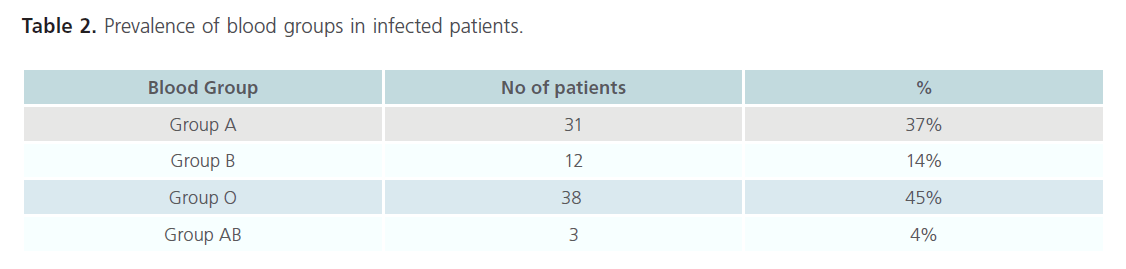
Table 2. Prevalence of blood groups in infected patients.
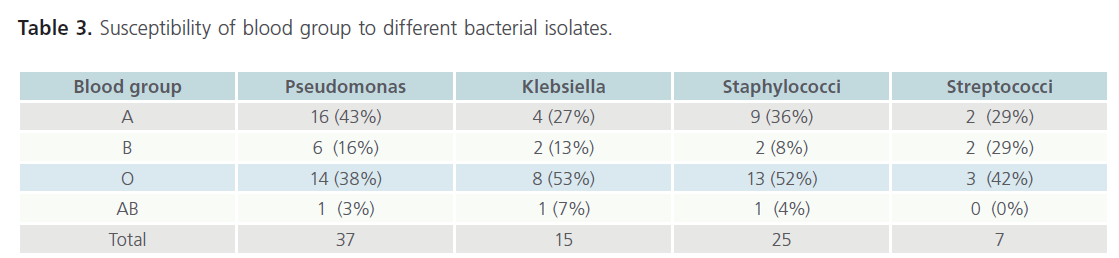
The distribution of different blood group within four main bacterial isolates was determined as following: 43% of blood group A patients were infected by pseudomonas; (27%) Klebsiella; (36%) Staphylococci; and (29%) Streptococci. While, group B individuals were infected with: Pseudomonas (16%), Klebsiella (13%), Staphylococci (8%) and Streptococci (29%). Meanwhile, blood group O patients had one of the following strains: 38% Pseudomonas, 53% Klebsiella, 52% Staphylococci, 42% Streptococci. Only, 3% of Pseudomonas, 7% of Klebsiella, and 4% of Staphylococci infected in-patients who expressed blood group AB, none of the patients had multiple infection (Table 3).
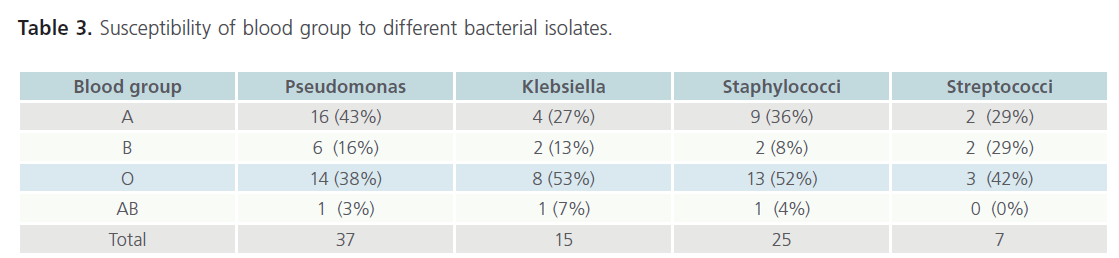
Table 3. Susceptibility of blood group to different bacterial isolates.
Discussion
Since the nosocomial infections are caused by viral, bacterial, and fungal pathogens. These pathogens should be investigated in all febrile patients who are admitted for a nonfebrile illness [2]. Many literature studies showed three important types of bacteria characterized to cause disease and associated with nosocomial infection, and linked to blood group antigens; Staphylococcus aureus were correlated to Lea blood group antigen, Pseudomonas aeruginosa linked to P blood group antigen which found to act as a receptor of other pathogenic bacteria such as E. coli, and as ligands for vetrotoxines from some bacteria like Shigella dysentereiae [14]. Klebsiella pneumoniae an important bacteria of hospital acquired infection was associated with B, and AB blood group antigens, compared with other blood group antigens [11]. Distribution of ABO blood group antigens in other tissues was associated with the disease and bacterial infections, such as Helicobacter pylori infection of peptic ulcer patients were referred to expression of ABH antigens in the mucosa of the stomach, these relationship explained the increase susceptibility of H. Pylori to blood group O or A phenotype and the non secretor of Leb blood group antigen [12,14].
The distribution of blood group antigens among traumatic Libyan patients refared to Trauma Hospital were 46% O blood group, 35% blood group A; 17% B blood group; and 2% AB blood group. Despite the majority of patient were blood group O, Pseudomonas infected more blood group A patients compared with other blood groups, these observation might be due to the expiration of P blood group antigen which acts as receptor for P. aeruginosa leading to increased density of colonization [14], similar study of minor blood group and their effects on blood transfusion showed that the P blood group antigen expressed on the cell surface of patients with blood group A more than other blood groups [17], this study strongly supports the association of P blood group antigens with Pseudomonas infection and the susceptibility of blood group A to Pseudomonas infection compared with other blood group antigen.
Staph aureus is one of an important agent associated with hospital associated infections, it was ranked the second causative agent in traumatic patients, mainly isolated from patients with blood group O more than other blood groups, these might be due to Lea blood group antigen which act as receptor for Staphylococci [18], it has been observed that blood group O individuals express more Lea compared with another blood groups among Libyan population [17], although 45% of Libyan population were blood group O these might explain the increased the prevalence of Staphylococci in traumatic Libyan patients.
In contrast to Kostink and colleagues [11] who demonstrated that blood group B and blood group AB individuals are at high risk of Klebsiella, this study found to be less prevalence in traumatic patients, it might be due to the high prevalence of blood group O among traumatic patients and the site of infection therefore the susceptible to Klebsiella infection is more with blood group O compared with other blood groups. The results of this study conclude that the most common bacterial infection among traumatic patients was Pseudomonas followed by Staphylococci and Klebseilla. Individuals of blood group A are more susceptible to Pseudomonas infection where as blood group O more susceptible to Klebsiella and Staphylococci but these observation require further study to include other blood group antigens and other factors which contribute to the infection includes the antibiotic resistance which is one of the important problem leading to nosocomial infection [15,16] and other blood group antigens such as Lewis antigens, MNS antigens, Kel and Duffy antigens with more samples from different site of the body from other Libyan hospitals.
1857
References
- Greenwood, D., Slack, RCB., Peutherer, JF. Medical Microbiology. London: Churchill Livingstone. 2002. p. 709.
- Jamovich, D., Winder, ML., Domachowske, J., Steele, RW., Tola, RW. Hospital acquire infections. Medicine from WebMD. 2006.
- Zerr, DM., Garrison, MM., Allpress, AL., Heath, J., Christakis, DA. Infection control and hospital associated infections among surgical patients: variability and associations in a multicenter pediatric setting. Pediat 2005; 115: e387-e392.
- Osmon, S., Warren, D., Seiler, SM., Shannon, W., Fraser, VJ. et al. The influence of infection on hospital mortality for patients requiring >48 h of Intensive Care. Chest. 2003; 124: 1021-1029.
- Anstee, DJ. The relationship between blood groups and disease. Blood 2010; 115: 4635-4643.
- Musken, A., Souady, J., Dreisewerd, K., Zhang, W., Distler, U. et al. Application of thin-layer chromatography/infrared matrix-assisted laser desorption/ionization orthogonal time-off light mass spectrometry to structural analysis of bacteria-binding glycosphingolipids selected by affinity detection. Rapid Commun Mass Spectrum 2010; 24: 1032- 1038.
- Lund, N., Olsson, ML., Ramkumar, S., Sakac, D., Yahalom, V. et al. The human P(k) histo-blood group antigen provides protection against HIV-1 infection. Blood 2009; 113: 4980-4991.
- Branch, D. Blood groups and susceptibility to virus infection: new developments. Curr Opin Haem 2010; 558-564.
- King, MJ. Blood group antigens on human erythrocytes-distribution, and possible functions. Biochim Biophys Acta 1994; 1197: 15-44.
- Olsson, ML., Hellberg, A. P-related Blood Group System. Transfusion 2003; 34: 899.
- Kostiuk, OP., Chernyshora, LI., Slukving, II. Protective effect of lactobacillus acidophilus on development of infection, caused by Klebsiella pneumoniae. Fiziol Zh 1993; 39: 62-8.
- Colbeck, JC., Hansen, LM., Fong, JM., Solnick, JV. Genotyping Profile of the Outer Membrane Proteins BabA and BabAB in Clinical Isolates of Helicobacter pylori. Infect Immun. 2006; 74: 4375-8.
- Rad, R., Gerhard, M., Lang, R., Schniger, M., Thomas, R. et al. The Helicobacter pylori blood group antigen-binding adhesion facilitates bacterial colonization and augment a nonspecific immune response. J Immunol. 2002; 168: 3033-3041.
- Suadicani, P., Hein, HO., Gyntelberg, F. Genetic and life style determinants of peptic ulcer. A study of 3387 men aged 54 to 74 years: The Copenhagen male study. Scand J Gasroentterol. 1999; 34: 12-7.
- Cartelle, M., Tomas, MD., Pertegae, S., Becerio, A., Dominguez, MA. et al. Risk factor for colonization and infection in a hospital outbreak caused by a strain of Klebsiella pneumoniaewith reduced susceptibility to expanded-spectrum cephalosporin. J Clinical Microbial 2004; 42: 4242-4249.
- Zavascki, AP., Barth, AL., Gaspareto, PB., Goncalves, AL. et al. Risk factors for nocomial infections due to pseudomonas aeruginosa producing metallo-β-lactmase in two tertiary-care teaching hospitals. J Antimicrob Chemot. 2006; 58: 882-885.
- Najla, F., Elmagri, A., Alkout, AM. Minor blood group antigens and their effects on blood transfusion in Libyan population. Thesis of Ms degree in Biomedical Science. Academy of Graduate Studies. 2008.
- Saadi, AT., Essery, SD., Raza, MW., El Ahmer, OR., Alkout, AM. et al. Adhesins of Staphylococcus aureus that bind Lewisa antigen relationship to sudden infant death syndrome. Toward anti-adhesin therapy of microbial diseases. Bat-Sheva Seminar. Zichron Yaakov, Israel. 1996. pp. 62-63.