Keywords:
Primary health care; Diabetes mellitus; Depression; Chronic disease
Introduction
Diabetes mellitus is a chronic disease caused by inherited and/or acquired deficiency in production of insulin by the pancreas, or by the ineffectiveness of the insulin produced.
Such a deficiency results in increased concentrations of glucose in the blood, which in turn damage many of the body's systems, in particular the blood vessels and nerves [1].
There are two principle forms of diabetes: Type 1 diabetes (formerly known as insulin-dependent) and Type 2 diabetes (formerly named non-insulin-dependent), that results from the body's inability to respond properly to the action of insulin produced by the pancreas. Type 2 diabetes is much more common and accounts for around 90% of all diabetes cases worldwide. It occurs most frequently in adults, but is being noted increasingly in adolescents as well [1].
Diabetes care is complex and requires that many issues, beyond glycemic control, be addressed. A large body of evidence exists that supports a range of interventions to improve diabetes outcomes. One of these issues which should be taking in mind is psychological effect of diabetes on the patient’s life especially depression which is preventable and treatable [2].
Depression is a common mental disorder that presents with depressed mood, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, low energy, and poor concentration. And according to WHO depression is the leading cause of disability and the 4th leading contributor to the global burden of disease [3].
Current data indicate that the lifetime prevalence of depression in the general population may range from 2% to 15%, while it is much higher in patients with diabetes (9% to 27%) [4]. In the general population, depression is exceedingly common, sometimes difficult to diagnose, and under treated [5]. In patients with chronic conditions such as diabetes, depressive disorders seem to occur even more frequently, have a high rate of recurrence, and seem to be associated with worsened medical outcomes [6,7].
The high prevalence of depression in diabetes, the frequency of depression onset before diabetes complications, the similarity in the hypothalamic-pituitary axis changes found in depression and poorly controlled diabetes mellitus, indicates that diabetic patients are more susceptible to neurochemical and behavioral changes similar to those found in depression, and mood shifts often associated with glycemic changes [8-10].
Of practical clinical importance, growing evidence shows that depressive disorders in adults are associated with one of the key markers of medical outcome: worsened glycemic control [11,12]. Depressive disorders may place diabetic patients at increased risk for long-term complications [13,14]. Previous studies have suggested that the extent of the difference in glycemic control between depressed and nondepressed patients is equivalent to that of the glycemic differences between the intensive and conventional treatment groups of the Diabetes Control and Complications Trial [15,16]. This suggests that if it persists over time, hyperglycaemiaassociated depression may have substantial medical consequences [17]. It also underscores the importance of recognition and proper treatment of depression in diabetic patients [18].
Methodology
The PHCCs in Jeddah city were distributed to six main regions from each region one of them was chosen randomly by this we ended with six PHCCS. The study was conducted in the assigned sex PHCCs and the assigned physicians were trained for interviewing the patients. We interview a total of 155 patients.
We include both genders and all nationalities with type 2 DM and we exclude type 1 DM, We interviewed the first 26 patients attending the clinic; it took 2-3 clinics to finish interviewing the assigned number of patients to each physician. After the data collection the researcher choose randomly 10% of each sample in each PHCC and double check the data that were taking from the patient files it was less than 5% of the total data however it was corrected by the researcher to assure its validity.
We used The Arabic version of Beck’s Depression Inventory [19]. All data entered in Statistical Package for Social Science (SPSS V.20) and analyzed by suitable statistical test (Chi square and fisher exact test). In some of the analysis we had to collapse some cells together to be able to perform a statistical analysis on it.
Results
A total of 155 diabetic patients type 2 were included in this study according to the inclusion and exclusion criteria and the results were:
Population description
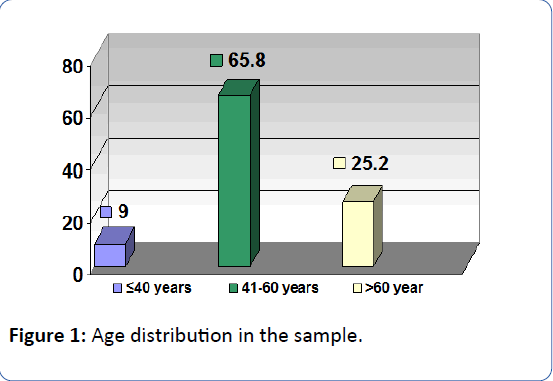
As shown in Figure 1 102 (65%) of our sample ages were between 41-60 years of age and the mean of age was 52.84 ± 9.5 years.
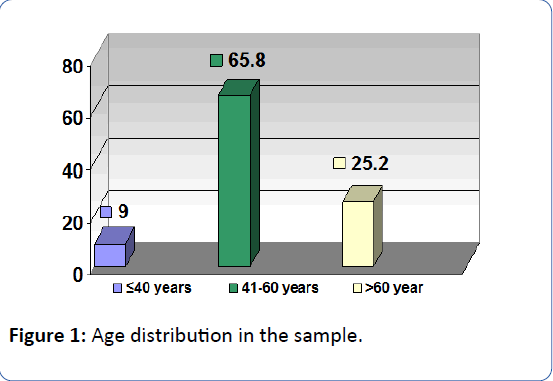
Figure 1: Age distribution in the sample.
Table 1 represent the distribution of the sample according to sex and nationality it showed that the majority of the sample were Saudi female 76 (49%) of the total sample.
| Gender |
Nationality |
Total |
| Saudi |
Non-Saudi |
|
| Male |
56 |
19 |
75 (48.4%) |
| Female |
76 |
4 |
80 (51.6%) |
| Total |
132 (85.2%) |
23 (14.8%) |
155 |
Table 1: The distribution of the sample according to gender and nationality.
As shown in Table 2 (47.7%) of diabetic patients were unemployed (56. %) of them are married while (89%) of employed sample were married.
| Variables |
|
Occupation |
Total % |
| |
Employed |
Unemployed |
Retired |
| Marital Status |
Single |
6 |
0 |
0 |
6 (3.9) |
| Married |
50 |
42 |
18 |
110 (71) |
| Divorced |
0 |
4 |
2 |
6 (3.9) |
| Widow |
0 |
28 |
5 |
33 (21.3) |
| Total |
|
56 (36.1%) |
74 (47.7%) |
25 (16.1%) |
155 |
Table 2: The distribution of the sample according to occupation and marital status.
As shown in Table 3 (66.5%) of diabetic patients were having an income of less than 2000 riyal per month.
| Monthly income in Saudi Riyal |
No. (%) |
| >2000 |
103 (66.5) |
| 2000-4000 |
17 (11) |
| 4001-6000 |
12 (7.7) |
| 6001-80000 |
11 (7.1) |
| 8001-10000 |
4 (2.6) |
| >10000 |
8 (5.2) |
| Total |
155 |
Table 3: Distribution of the sample according to income.
Prevalence of depression
The prevalence of depression among diabetics Type 2 in the study sample has been found to be 48.4%, 23% of them were having moderate-severe depression (Major depression disorder according to DSM VI Revised) while 25% of them were having mild depression (Figure 2).

Figure 2: The classification of depression in the study sample according to the degree of severity.
Depression in type 2 DM patients according to relevant variables
As shown in Table 4 the prevalence of depression among those who were older than 60 years old (64.1%) was significantly higher than that among patients who were younger than that and it was statistically significant (P value 0.012).
| Presence of depression |
Age groups |
Total |
X2 |
P-value |
| ≤ 40 |
41-50 |
51-60 |
>60 |
| Yes |
8 (57.1%) |
26 (52%) |
16 (30.8%) |
25 (64.1%) |
75 |
11.011 |
0.012 |
| No |
6 (42.9%) |
24 (48.0%) |
36 69.2%) |
14 (35.9%) |
80 |
Table 4: Distribution of diabetic patients according to age and the presence of depression.
As shown in Table 5 the prevalence of depression among those who were taking more than 3 drugs (56.8%) was significantly higher than that among patients who were taking less than 3 drugs and it was statistically significant (P value 0.033).
| Presence of depression |
Number of drugs |
|
Total |
X2 |
P-value |
| ≤ 3 |
>3 |
| Yes |
33 (40.7%) |
42 (56.8%) |
75 |
3.972 |
0.033 |
| No |
48 (59.3%) |
32 (43.2%) |
80 |
Table 5: Distribution of diabetic patients according to number of drugs and the presence of depression.
As shown in Table 6 the prevalence of depression among those who were using insulin (72%) was significantly higher than that among patients who were not taking insulin and it was statistically significant (P value 0.009).
| Presence of depression |
Use of insulin |
Total |
X2 |
P-value |
| Yes |
No |
| Yes |
18 (72%) |
57 (43.8%) |
75 |
6.655 |
0.009 |
| No |
7 (28%) |
73 (56.2%) |
80 |
Table 6: Distribution of diabetic patients according to use of insulin and the presence of depression.
As shown in Table 7 the prevalence of depression among those who were having complications (68.4%) was significantly higher than that among patients who were not having complications and it was statistically significant (P value 0.009).
| Presence of depression |
Presence of complications |
Total |
X2 |
P-value |
| Yes |
No |
| Yes |
26 (68.4%) |
49 (41.9%) |
75 |
8.09 |
0.009 |
| No |
12 (31.6%) |
68 (58.1%) |
80 |
Table 7: Distribution of diabetic patients according to presence of complications and the presence of depression.
As shown in Table 8 the prevalence of depression among those who were having more than 4 follow-up visits per year (58.6%) was significantly higher than that among patients who were having less than 4 follow-up visits per year and it was statistically significant (P value 0.016).
| Presence of depression |
Number of follow-ups/year |
Total |
X2 |
P-value |
| ≤ 4 |
>4 |
| Yes |
34 (40%) |
41 (58.6%) |
75 |
5.301 |
0.016 |
| No |
51 (60%) |
29 (41.4%) |
80 |
Table 8: Distribution of diabetic patients according to number of follow-ups per year and the presence of depression.
As shown in Table 9 the prevalence of depression among those who were having fasting blood sugar level more than 130 mg/dl (55.6%) was significantly higher than that among patients who were having fasting blood sugar level less than 130 mg/dl and it was statistically significant (P value 0.013).
| Presence of depression |
FBS level |
Total |
X2 |
P-value |
| ≤ 130 mg/dl |
>130 mg/dl |
| Yes |
20 (35.7%) |
55 (55.6%) |
75 |
5.638 |
0.013 |
| No |
36 (64.3%) |
44 (44.4%) |
80 |
Table 9: Distributions of diabetic patients according to fasting blood sugar level and the presence of depression.
As shown in Table 10 the prevalence of depression among female diabetic patients (50%) was higher than male diabetic patients (46.7%) but it was statistically insignificant (P value 0.4).
| Presence of depression |
Gender |
Total |
Fishers exact test |
P-value |
| Male |
Female |
| Yes |
35 (46.7%) |
40 (50%) |
75 |
172 |
0.4 |
| No |
40 (53.3%) |
40 (50%) |
80 |
Table 10: Distributions of diabetic patients according to gender and the presence of depression.
As shown in Table 11 the prevalence of depression among those who were having a family history of depression (66.7%) was significantly higher than that among patients who were not having a family history of depression but it was statistically insignificant (P value 0.08).
| Presence of depression |
Family History of depression |
Total |
Fishers exact test |
P-value |
| Yes |
No |
| Yes |
12 (66.7%) |
63 (46%) |
75 |
2.725 |
0.08 |
| No |
6 (33.3%) |
74 (54%) |
80 |
Table 11: Distributions of diabetic patients according to family history of depression and the presence of depression.
As shown in Table 12 the prevalence of depression among those who were not having another diseases (54.4%) was significantly higher than that among patients who were having another diseases but it was statistically insignificant (P value 0.053).
| Presence of depression |
Presence of other diseases |
Total |
Fishers exact test |
P-value |
| Yes |
No |
| Yes |
26 (40%) |
49 (54.4%) |
75 |
3.153 |
0.053 |
| No |
39 (60%) |
41 (45.6%) |
80 |
Table 12: Distributions of diabetic patients according to presence of other diseases and the presence of depression.
Discussion
The prevalence of depression in our study was 48% which considered to be high compared to other studies which they reported the prevalence to be between 11% and 40% [20-28]. Studies conducted in Netherlands (31%) [24], in Bahrain (33.3) [25], in Malaysia (30.5) [26], in Palestine (40%) [27], and in Nigerian Teaching Hospital (30%) [28]. This may be explained that we included mild depression in the study not like other studies which included major depression only according to DSM VI criteria, which was in this study 23%.
As shown in previous studies that younger age was associated with presence of depression as result of more conflicts and instability and stress. Also high prevalence of depression among patients older than 60 years was higher these finding were reported in the same distribution in our study and they were significant. These known to be due to the long duration of the disease and by the presence of complications as the patients get older [22].
The prevalence of depression among patients taking more than 3 drugs was 56% this is could be due to presence of comorbid disease and also the presence of complications and it was a significant finding in our study [21].
The prevalence of depression among patients who use insulin was 72% while the depression was reported among 43.8% of those not taken insulin which was significant, peyrot and Ruben found that odds ratio is increased by 0.4 in diabetic’s type 2 who are taking insulin to have depression. It can be explained by that they are uncontrolled or having a complicated course of the disease [20,22,23].
Also we found that those with complication were more prone to depression than other (68.4%) which was also statistically significant [20,22,23]. Peyrot and Ruben reported that having more than 2 complications will increase odds ratio of having depression by 2.7 from that we can say that depression and complications of diabetes could be linked. Lustman said the longer the time spent being depressed, the greater the risk of developing retinopathy due to long periods of poor glycemic control and in the short term, hyperglycemia [21]. This is supported by De Groot et al. whose meta-analysis indicates that there is a significant association between depression and diabetic retinopathy, neuropathy, nephropathy, sexual dysfunction and macrovascular complications. This means an increase in depressive symptoms was associated with a rise in the severity or number of diabetes complications [21].
The high prevalence of depression among patients who were having more than 4 follow-ups per year can be explained also that those patients are having uncontrolled and complicated course of diabetes are having more follow-ups than the controlled patients [20,22,23].
We found that patients with uncontrolled diabetes were having depression more the controlled one (55.6% vs. 35.7%) our indicator was the level of fasting blood sugar of the patient, due to unavailability of Hba1C in the in the study area. Lustman and others found that uncontrolled diabetes will increase the odds of having depression as shown in our results through difficulty to maintain their initiative activities as Lin found [20,22,23].
Our results shows that female were more depressed than male diabetics 50% vs. 46%, although it was insignificant statically. Lustman and peyrot reported that females are more prone to have depression than male [22].
As we discussed before previous studies shows that family history of depression will increase the odds of having depression in our finding were in the same track (66% vs. 46%), but it was statistically insignificant [20].
Our study shows that 66.5% of the samples taking were having income less than 2000 Saudi riyal per month, which could be explained that only low income patients will follow their diabetes in governmental primary care, but those who have monthly income more than 2000 Saudi riyal they may seek other alternative sectors such as private hospitals or private polyclinics.
Conclusion
The results showed that 48% of type 2 DM patients had depression according to BDI scores; however it was higher than that recorded in studies conducted in other parts of the world. The prevalence of depression more among females (50%) than that among males (46%), which was in agreement with most of the studies conducted in the same issue, however it was insignificant in our study. Also it was noticed that depression was more prevalent among patients below 40 years and more than 60 years and it was also an agreement by most of other studies which were done on same topic. Also we found that family history of psychiatric illness and use of insulin were significantly increasing the occurrence of depression, same results were found by peyrot and Ruben.
And we found that taking more than 3 drugs or having more than 4 follow-ups per year will increase the odds of having depression, which was explained that by the presence of complications in those patients, which was found to be a significant factor in increasing cases of depression among our sample. Also uncontrolled type 2 DM patients were having more depression than controlled patients.
In the end, Depression among type 2 DM patients in our area was high and it is affecting the outcome of our care as well and it associated with factors that will increase the odd of occurrence of it Age, Sex, No. of drugs, Use of insulin, Complications, Fasting blood glucose level (control level), No. of follow-ups per year.
Recommendations
Increase the physicians’ awareness about the presence of depression in diabetics and how to deal with it. Emphasize on the topic of depression in the health education. Implementation of an annual education programs to the physicians to update and improve quality of care through courses or online continuous medical education programs which the physician in his office or home can access. Further studies in the coming years are needed among diabetic patients to improve quality of care that is presented to them knowing that more than 20% of our community has diabetes.
23226
References
- American Diabetes Association (2003) Standards of Medical Care for Patients With Diabetes Mellitus. Diab Care 26: S33-S50.
- Anderson RJ, Freedland KE, Clouse RE, Lustman PJ (2001) The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diab Care 24: 1069-1078.
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, et al. (1994) Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the united states. Results from the national comorbidity survey. Arch Gen Psychiatry 51: 8-19.
- Katon W, von Korff M, Lin E, Bush T, Ormel J (1992) Adequacy and duration of antidepressant treatment in primary care. Med Care 30: 67-76.
- Gavard JA, Lustman PJ, Clouse RE (1993) Prevalence of depression in adults with diabetes. An epidemiological evaluation. Diab Care 16: 1167-1178.
- Lustman PJ, Griffith LS, Freedland KE, Clouse RE (1997) The course of major depression in diabetes. Gen Hosp Psychiatry 19:138-143.
- Frasure-Smith N, Lespérance F, Talajic M (1993) Depression following myocardial infarction. Impact on 6-month survival. JAMA 270: 1819-1825.
- Cohen ST, Welch G, Jacobson AM, De Groot M, Samson J (1997) The association of lifetime psychiatric illness and increased retinopathy in patients with type I diabetes mellitus. Psychosomat 38: 98-108.
- Kovacs M, Mukerji P, Drash A, Iyengar S (1995) Biomedical and psychiatric risk factors for retinopathy among children with IDDM. Diab Care 12: 1592-1599.
- Hudson J, Hudson M, Rothschild A, Vignati L, Schatzberg A, et al. (1984) Abnormal results of dexamethasone suppression tests in nondepressed patients with diabetes mellitus. Arch Gen Psychiatry 41: 1086-1089.
- Bellush L, Rowland N (1989) Stress and behavior in streptozotocin diabetic rats: biochemical correlates of passive avoidance learning. Behav Neurosci 103: 144-150.
- Weinger K, Jacobson AM, Draelos MT, Finkelstein DM, Simonson DC (1995) Blood glucose estimation and symptoms during hyperglycemia and hypoglycemia in patients with insulin-dependent diabetes mellitus. Am J Med 98: 22-31.
- Mazze RS, Lucido D, Shamoon H (1984) Psychological and social correlates of glycemic control. Diab Care 7: 360-366.
- Lustman P, Griffith L, Clouse R (1988) Depression in adults with diabetes. Results of 5-year follow-up study. Diab Care 11: 605-612.
- Leedom L, Meehan W, Procci W, Zeidler A (1991) Symptoms of depression in patients with type II diabetes mellitus. Psychosomat 32: 280-286.
- The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329: 977-986.
- Abdel-Khalek A (1998) Internal consistency of an Arabic adaptation of the beck depression inventory in four Arab countries. Psychol Rep 82: 264-266.
- Tellez-Zenteno JF, Cardiel MH (2002) Risk factors associated with depression in patients with type 2 diabetes mellitus. Arch Med Res 33: 53-60.
- Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, et al. (2000) Depression and poor glycemic control. Diab Care 23: 934-942.
- Xu L, Ren J, Cheng M, Tang K (2004) Depressive symptoms and risk factors in Chinese persons with type 2 diabetes. Arch Med Res 35: 301-307.
- Peyrot M, Ruben RR (1999) Persistence of depressive symptoms in diabetic adults. Diab Care 22: 448-452.
- Pouwer F, Geelhoed-Duijvestijn PH, Tack CJ, Bazelmans E, Beekman AJ, et al. (2010) Prevalence of comorbid depression is high in out-patients with Type 1 or Type 2 diabetes mellitus. Results from three out-patient clinics in the Netherlands. Diab Med 27: 217-224.
- Nasser J, Habib F, Hasan M, Khalil N (2009) Prevalence of depression among people with diabetes attending diabetes clinics at primary health settings. Bahrain Med Bulletin 31: 3.
- Kaur G, Tee GH, Ariaratnam S, Krishnapillai AS, China K (2013) Depression, anxiety and stress symptoms among diabetics in Malaysia: a cross sectional study in an urban primary care setting. BMC Fam Pract 14: 69.
- Sweileh WM, Abu-Hadeed HM, Al-Jabi SW, Zyoud SH (2014) Prevalence of depression among people with type 2 diabetes mellitus: a cross sectional study in Palestine. BMC Pub Health 14: 163.
- James BO, Omoaregba JO, Eze G, Morakinyo O (2010) Depression among patients with diabetes mellitus in a Nigerian teaching hospital. South Afr J Psychiat 16: 61-64.