Keywords
Iron deficiency anemia; Dodola; Pregnant women; Prevalence
Introduction
Anemia is defined as reduction in red cell mass which will decrease oxygen-carrying capacity of red blood cells to tissues that can be investigated in the laboratory by reduction in hemoglobin concentration (hemoglobin level of less than 11 gm/ dL) or hematocrit value is less than 33% [1]. Anemia in pregnant women is often caused by iron deficiency, which is the most common nutrient deficiency in the world, affecting more than two billion people globally. Although it is particularly prevalent in less developed countries, it remains a significant problem in the developed world, even where other forms of malnutrition have already been almost eliminated [2] during pregnancy and lactation nutrient requirement like iron is increase to support foetal and then infant growth and development [3].
The requirement of iron during pregnancy is around 1000 mg, 450 mg for red blood cells and uterine muscle, 270 mg for foetal iron, 170-200 mg for daily loss and 90 mg for placenta. There are additional needs for blood loss during delivery, 190 mg and lactation 1 mg/day assuming the stores are adequate, and a pregnant women average daily requirement is 3.4 mg/day [4]. Pregnancy is a period of increase requirement for micronutrient and that fulfil demands for physiological changes of mother and the foetus. During this period, the micronutrient such as iron, zinc and folic is the major marker that affects both the foetus and pregnant women [5].
Iron is an essential mineral to human. It is necessary for the synthesis of haemoglobin and myoglobin as well as for the function of many vital iron dependent enzymes in women of reproductive age iron deficiency anemia reduces cognitive ability and physical performance [6]. The greatest need for increased iron intake occurs in the second half of pregnancy. When the iron needs of pregnancy are not met, maternal haemoglobin Falls below 11 g/d. when the haemoglobin level is below 10 mg/ dL (haematocrit under 33%), iron deficiency is suspected [7] Inadequate intake or absorption of iron conjunction with blood loss during pregnancy may contribute to anemia. Iron deficiency and consequent anemia during pregnancy could be associated with severe complication like increase risks of maternal mortality and morbidity, premature delivery and low birth weight [8,9].
Literature Review
Prevalence of iron deficiency anemia
Iron deficiency is the most common and wide spread nutrition disorder in the world. It affects more than 80% of the world population. Iron deficiency anemia is one of the prevalent nutritional deficiency problem affecting pregnant women [10]. Tanzania pregnant women revealed that 95% of Tanzanian pregnant subjects were anaemic and all these women suffering from mainly iron deficiency. In India 65% to 75% of pregnant affected by anemia [11]. Factors responsible for this prevalence of anemia have been shown to be iron deficiency. Ninety five percent of pregnant populations of Multan area in partisan were anaemic of these 76% of macrocytic hypo chromic resulting from iron deficiency is the most frequent form of anemia [12]. In sub-Saharan Africa the prevalence rate for iron deficiency anemia in pregnant women is 58%. Nearly half of the pregnant women in the world to be anaemic [2]. A study done in 2014 in the urban area of eastern Ethiopia puts the prevalence of maternal anemia during pregnancy was 56.8%. This is relatively high prevalence what we have try to see from other research’s [13]. A study carried out at Mekelle town, north-west Tigray in 2011 showed that the prevalence of iron deficiency anemia was 36.1% [14]. This shows a slight increased prevalence of iron deficiency anemia compared to another research conducted in western region of Ethiopia, which was 29% [15]. Another research conducted at Azezo health center in 2011 tries to show that the prevalence of iron deficiency anemia among pregnant women were 21.6% [16]. This is relatively low prevalence, decreased by half, a research conducted at Bahr Dar town with prevalence of 45.5% [17]. The prevalence of iron deficiency anemia and associated factors among pregnant women who had ANC follow up at Gondar University hospital 2014 was 16% [18]. Although iron deficiency anemia was been recognized as a public health problem for many years little progress has been reported and the global prevalence of iron deficiency remains unacceptably high. WHO and UNICEF therefore reemphasized the urgent need to combat iron deficiency anemia stress the importance of recognizing its multifactor etiology for development of effective control programs [2].
Among the 1000 post natal women, the prevalence was 537, of the 1077 antenatal women studied, 540 were anaemic. The high prevalence was strongly associated with low socioeconomic status. Hence it can be concluded that empowering women in terms of education and economic status is the key factor in combating anemia in pregnancy to prevent the vicious cycle of associated problems [11].
Source of iron rich foods
Nutrition plays an important role during pregnancy. Literatures showed that women who are not supplemented with iron during their pregnancy are highly susceptible to develop anemia, hence iron deficiency anemia is the most common type of anemia during pregnancy [13]. A study in northern Tigray showed that the prevalence of Anemia was high among pregnant women having a meal frequency of less than two times per day, who takes coffee and tea with meal and those who are not supplemented with iron and foliate compared to those who takes a meal frequency of greater than three times per day, who does not take coffee and tea with meal and those pregnant women who are supplemented with iron and foliate [14]. There is two forms of dietary iron, hem and non-hem. Hem iron is found in animal foods that originally contained hemoglobin such as red meats, fishes and poultry. Iron in plant foods, Such as lentils and beans is arranged in a chemical structure called non hem iron [19]. This is the form of iron added to iron enriched and iron fortified foods. Hem iron is absorbed better than non-hem iron, but most dietary iron is nonhem iron [8]. The amount of iron absorbed from the diets highly dependent on the composition of the diet, namely, the quantity of substance that enhance or inhabit dietary iron absorption. Tea and coffee inhibit iron absorption when consumed with a meal or shortly after a meal. Hem food sources, predominately red meats, contain highly absorbable iron and promote the absorption of iron from other less bio-available food sources. Vitamin C is also a powerful enhancer of iron absorption from non-metal foods when consumed with a meal. The size of the vitamin C effect on iron absorption increases with the quantity of vitamin C in the meal. Unfortunately, foods rich in vitamin C tend to be seasonally available, and both meat and vitamin C rich foods tend to be expensive in less developed countries. Germination and fermentation of cereals and legumes improves the Bioavailability of iron by reducing the content of fiber, a substance in food that Inhibit iron absorption. Although much is known about factors that enhance or inhibit iron absorption the amount of change in iron absorption that can be achieved through dietary improvements accessible to poor populations remains in question. Dietary improvement becomes more feasible as economic means and dietary diversity increase [20].
Nutrient requirement increases during pregnancy to support fetal growth and maternal health. Iron requirements of pregnant women are approximately double that of non-pregnant women because of increased blood volume during pregnancy, increased need of the foetus and blood losses that occur during delivery. These result in higher requirements about 700-850 mg of iron to meet required amount in mother and foetus during pregnancy at delivery and during prenatal period [21]. If this increased iron requirement not compensated by iron intake, iron deficiency anemia can occur that result in adverse health effects not only to pregnancy but also for infants [22].
Factors associated with Iron deficiency anemia among pregnant women
A study conducted western Tigray explains that maternal age is highly associated with iron deficiency anemia. That means as maternal age increased the occurrence of iron deficiency anemia increased [14]. Another study says urban residence and illiterates women’s are highly affected groups [23]. A study conducted in western part of Ethiopia elucidates iron deficiency anemia prevalence among women’s who are illiterate, living in rural area, among families People in lower socio economic groups have doubled the risk of those who are middle or upper class [16]. The maternal factor included were age, education, income having monthly income of less than 1000 Ethiopian birr, family size of more than or equal to five are highly associated with anemia [21]. A number of literatures show that socio-demographic factors are directly associated with maternal anemia during pregnancy who have home delivery [15]. Another study conducted at Nekemte concludes that age and occupation has no any association with iron deficiency anemia [23]. Women from low socio-economic status had a fourth fold increase risk compared to those high social class [24].
Methodology
Study settings
The study was conducted in Dodola General Hospital which is found in West Arsi Zone, Oromia Regional State, South East Ethiopia and 325 km away from Addis Ababa, Capital city of Ethiopia and 75 km from Zonal Town, Shashemene. The hospital is graduated from type A health center in 2002 E.C., the hospital give services for Dodola town population and six neighboring district population like Dodola rural, Adaba, Gadab Asasa, Kokosa, Nansabo and Other. In 2010 E.C. it became General Hospital. As the data obtained from program and data technician the recent catchment population is about 863,517 among these 426,988 are males and 436,529 are females. Children under one years of age are 27,805, less than five years of age are 141, 875, women 15-49 years of age are 191,096 and numbers of pregnant women are estimated to be 29,964. The town is located in Oromia Region which is conditioned by an overall elevation of between 2362 and 2493 meters above sea level. The climate is stable, with temperature variation 24 and 26 degree centigrade. It provide various services with its department of surgery, Gynecology, Pediatrics, Medical, Obstetrics, Emergency, Laboratory, Pharmacy and ART clinic. The study was conducted from February 5 to March 30, 2018 G.C. [25].
Study design
Institutional based cross-sectional study was conducted to assess the Prevalence of iron deficiency anemia and associated factors among pregnant women attending ANC follow up at Dodola General Hospital.
Source and study population
Source population: All pregnant women who live in Dodola Town and around Dodola Town.
Study population: All Pregnant women who came to Dodola General Hospital for Focused Ante Natal Care from February 5 to March 30, 2018 G.C.
Study unit: Selected individuals.
Eligibility Criteria
Inclusion criteria
• All pregnant women who attend ANC follow up at Dodola General Hospital during data collection period.
• Willingness to participate in the study.
Exclusion criteria: Pregnant women who was critically ill and mentally unstable during the study.
Sample Size and Sampling Procedure
Sample size determination
The sample size was determined by using single population proportion formula. The following assumption are made on the previous research that showed the prevalence of iron deficiency anemia among pregnant women who had ANC follow up at Gondar University hospital in 2014 was 16% by measuring hemoglobin [18]. The sample size was calculated based on the following formula. A confidence interval to 95% was considered and level of significance was taken at α=0.05, margin of error 5%.
n= (Zα/2)2 × p(1-p)d2
= (1.96)2 × 0.16(1-0.16) (0.05)2
n= 206.5244~207
n=207 × 10% = 20.7+207=227.7~228
Where
Zα/2 = Standard normal variable at 95% confidence level (1.96)
p=Population proportion prevalence
d=Margin of error
n=Sample size
10%=Non respondent rate
Sampling technique and procedure
The Study was conducted by using Systematic random sampling technique to get study unit. The first participant was chosen with lottery method and all the next participant was selected based on interval (k) which is obtained by k=N/n; where k is the interval of respondent, N- all pregnant mother those attend ante natal care at Dodola General Hospital per month and n- is sample size [26-29]. That is by taking the flow of ante natal care attendants of Dodola General Hospital from Dodola General Hospital ANC registration book in month October and November 2017 there is 320,350 ANC followers at Dodola General Hospital respectively and by taking the average (320+350/2 =335 which is N). Then, k=335/228=1.469~2. Assuming these flow of attendants were occur in our study period the data was collected until total sample size achieved [30-32].
Data collection method
The data was collected using pretested, semi structured questionnaires through interviews and patient chart review. The interviewer administrated questionnaires contains sociodemographic factors, obstetric factor and nutritional status among pregnant women attending ANC at Dodola General Hospital. The questionnaires were adapted by reviewing different literatures similar with this study and considering the local situation of the study subject.
The questionnaire was prepared in English version then translated to Afaan Oromo (local language) for appropriateness of data collectors. Then after, Afaan Oromo version was again retranslated back to English version to check the consistency in meaning. Data was collected by Staff members of MCH ward (who works in Family planning and Expanded Program of immunizations). Training was given for data collectors prior to collecting data on how to collect data by group members.
Study Variables
Dependent variables: Prevalence of Iron deficiency anemia
Independent variables
• Socio-demographic status
• Age
• Marital status
• Ethnic group
• Religion
• Residence
• Occupation
• Educational status
• Income
• Family size
• Underlying Cause
• Number of ANC visit
• Parity
• Gravidity
• Birth interval
• Age at first marriage
• Gestational age
• Vaginal bleeding
• Immediate Cause
• Availability of supplement
• Caffeine intake
• Meal type
Operational definitions
Hemoglobin: Hemoglobin concentrations less than 11 g/dl in the blood of the individual
Iron: A micronutrient needed for the transport of oxygen in blood to various parts of the body.
Iron deficiency: A state of insufficient iron to maintain normal physiological functions of body tissues.
Iron Deficiency Anemia (IDA): An advanced stage of iron depletion and low hemoglobin concentration resulting in the condition of anemia or loss of iron excess and poor conditions.
Iron supplementation: Provision of specified dose of nutrient preparation which may be in the form of tablet, capsule or modified food for either treating an identified deficiency or prevention of the occurrence of such a deficiency in an individual.
Ante Natal Care (ANC): A comprehensive care which provides care for the mother's and fetus health is monitored, maintained and optimized to ensure a healthy pregnancy, safe delivery and post delivery period and provides nutritional supplements (iron/ folate and dietary information throughout the pregnancy.
Income: The money that earned for their work from Government, Private, daily labor and their agricultural products.
Gravidity: The number of times that a woman has been pregnant.
Parity: The number of times that a woman has given birth to a fetus at a gestational age of 28 weeks or more, regardless of whether the child was born alive or was stillborn.
Multigravida: A pregnant woman with one or more previous pregnancies.
Primigravida: A woman who is pregnant for the first time.
Nullipara: A women who has never given birth.
Data quality control
The questionnaires was prepared in English and translated in Afaan Oromo for the improvement of data quality. Five questionnaires was pre-tested at MWU GRH before two weeks of the actual data collection to ensure clarity, wordings, logical sequence and skip patterns of the questions and modification was made accordingly. The status of anemia was investigated at laboratory by measuring the level of hemoglobin.
Data processing and analysis
The collected data was entered, sorted, cleaned and analyzed by using SPSS version 20 statistical software. It was checked for its completeness, cleaned, processed and analyzed accordingly. Both bivariate and multivariate analysis was carried out to see the effect of Socio demographic conditions, obstetric factors and nutritional status. Finally summarized and presented by frequency tables and summary statistics.
Ethical considerations
The Ethical clearance was obtained from Madda Walabu University Goba Referral Hospital CBE office and Permission was obtained from Medical Director of Dodola General Hospital. Respondents were informed about the purpose of the study then information was collected after obtaining verbal consent from each participant. Respondents are allowed to refuse or discontinue participation at any time they want. Data collectors were request first for respondents consent orally and written consent forms are read for each respondent to obtain their agreement before starting interview. Furthermore, the participant was assured that their name and their answer was not mention in any way. Then, the researcher was assured the organization to have the copy of the study report and the participants have the right to know the result of the study. The study participants name and address information were not written, instead code was used to each study participants.
Results
Socio-demographic characteristics of the respondent
A total of 228 mothers participated in this study with response rate of 100%. The mean age of the women was 25.89 years with a SD of ±5.248 years. From the total mothers 83(36.4%) were in age group of 25-29, 66(28.9%) were in age group of 20-24 and the rest 17(7.5%) were in age group of above 35 in years. More than half of the mothers 163(71.5%) residence was urban and the remaining 65(28.5%) was rural. All the respondent 228(100%) were married.
The dominant ethnicity of the study population were Oromo 206(90.4%) followed by Amara 22(9.6%). More than half of the respondent 164(71.9%) were Islam followed by Orthodox 40(17.5%). The result of educational level of mothers showed that 88(38.6%) can’t read and write. Most of the mothers 137(60.1%) occupation was house wife and followed by 26(11.4%) was merchant. Majority of the partner’s educational status 82(36.0%) can read and write and 83(36.4%) were farmer (Table 1).
| Variables |
Category |
Frequency |
Percentage (%) |
| Age |
15-19 |
26 |
11.4 |
| 20-24 |
66 |
28.9 |
| 25-29 |
83 |
36.4 |
| 30-34 |
36 |
15.8 |
| >35 |
17 |
7.5 |
| Total |
228 |
100.0 |
| Marital Status |
Married |
228 |
100.0 |
| Single |
0 |
0 |
| Divorced |
0 |
0 |
| Widowed |
0 |
0 |
| Total |
228 |
100.0 |
| Ethnicity |
Oromo |
206 |
90.4 |
| Amara |
22 |
9.6 |
| Total |
228 |
100.0 |
| Religion |
Islam |
164 |
71.9 |
| Orthodox |
40 |
17.5 |
| Protestant |
16 |
7.0 |
| Catholic |
1 |
0.4 |
| Other |
7 |
3.1 |
| Total |
228 |
100.0 |
| Residence |
Urban |
163 |
71.5 |
| Rural |
65 |
28.5 |
| Total |
228 |
100.0 |
| Monthly income |
≤1000 |
125 |
54.8 |
| 1001-1500 |
65 |
28.5 |
| 1501-2000 |
26 |
11.4 |
| 2001-2500 |
7 |
3.1 |
| >2500 |
5 |
2.2 |
| Total |
228 |
100.0 |
| Educational Status of the mother |
Cannot read and write |
88 |
38.6 |
| Can read and write |
31 |
13.6 |
| Primary (1-8) school |
48 |
21.1 |
| Secondary (9-12) school |
30 |
13.2 |
| Collage and above |
31 |
13.6 |
| Total |
228 |
100.0 |
| Occupation |
House wife |
137 |
60.1 |
| Government employee |
21 |
9.2 |
| Private employee |
9 |
3.9 |
| Self employed |
13 |
5.7 |
| Merchant |
26 |
11.4 |
| Farmer |
22 |
9.6 |
| Total |
228 |
100.0 |
| Partner’s Educational Status |
Cannot read and write |
32 |
14.0 |
| Can read and write |
82 |
36.0 |
| Primary (1-8) school |
70 |
30.7 |
| Secondary (9-12) school |
28 |
12.3 |
| Collage and above |
16 |
7.0 |
| Total |
228 |
100.0 |
| Partner’s Occupation |
Unemployed |
15 |
6.6 |
| Government employee |
18 |
7.9 |
| Private employee |
16 |
7.0 |
| Self employed |
26 |
11.4 |
| Merchant |
60 |
26.3 |
| Farmer |
83 |
36.4 |
| Other |
10 |
4.4 |
| Total |
228 |
100.0 |
Table 1: Socio-demographic characteristics of pregnant mothers attended ANC follow up in Dodola General Hospital, Oromia Region, Southeast Ethiopia, 2018.
Reproductive health characteristics (obstetric factors)
More than half of the respondents 127 (55.7%) were gravida (2-5), 86(37.7%) were NulliPara and 174 (76.3%) had age at first marriage above 18 year. From the total participant 92 (40.4%) were in third trimester and 79(34.6%) of the participants had ANC follow up of two times. 78 (34.2%) of the respondent had single number of fetus in their uterus. Majority of the respondent has no history of vaginal bleeding during their current pregnancy (Table 2).
| Variable |
Category |
Frequency |
Percentage (%) |
| Gravidity |
1 |
55 |
24.1 |
| 2-5 |
127 |
55.7 |
| ≥6 |
46 |
20.2 |
| Total |
228 |
100.0 |
| Parity |
Nullipara |
86 |
37.7 |
| Multipara |
88 |
38.6 |
| Grandmultipara |
54 |
23.7 |
| Total |
228 |
100.0 |
| Age at first marriage |
<18 |
54 |
23.7 |
| ≥18 |
174 |
76.3 |
| Total |
228 |
100.0 |
| Birth interval |
Primigravida |
56 |
24.6 |
| <2 |
64 |
28.1 |
| 2-4 |
88 |
38.6 |
| ≥5 |
20 |
8.8 |
| Total |
228 |
100.0 |
| Family size |
2 |
60 |
26.3 |
| 3 |
49 |
21.5 |
| ≥4 |
119 |
52.2 |
| Total |
228 |
100.0 |
| Current pregnancy in weeks (Gestational age) |
≤12 |
75 |
32.9 |
| 13-27 |
40 |
17.5 |
| 28-40 |
92 |
40.4 |
| >40-≤42 |
21 |
9.2 |
| Total |
228 |
100.0 |
| Number of ANC visit in current pregnancy |
1 |
62 |
27.2 |
| 2 |
79 |
34.6 |
| 3 |
43 |
18.9 |
| 4 |
28 |
12.3 |
| Above four |
16 |
7.0 |
| Total |
228 |
100.0 |
| Supplementation of iron |
Yes |
174 |
76.3 |
| No |
54 |
23.7 |
| Total |
228 |
100.0 |
| Days of iron supplementation |
For a month |
46 |
20.2 |
| For two month |
86 |
37.7 |
| For three month |
31 |
13.6 |
| Above three month |
11 |
4.8 |
| Total |
174 |
76.3 |
| Number of fetus in current pregnancy in the uterus |
Singleton |
78 |
34.2 |
| Twins |
36 |
15.8 |
| I don’t know |
114 |
50.0 |
| Total |
228 |
100.0 |
| History of vaginal bleeding during current pregnancy |
Yes |
6 |
2.6 |
| No |
222 |
97.4 |
| Total |
228 |
100.0 |
Table 2: Reproductive health characteristics of pregnant mothers attended ANC follow up in Dodola General Hospital, Oromia Region, South East Ethiopia 2018.
Nutritional characteristics of the respondent
Among the total participants 184(80.7%) ate three times per day. Majority of the participant 137(60.1%) ate Injera with shiro. All of the respondents 228(100%) were use caffeine containing drinks and 132(57.9%) of them use caffeine containing drinks immediately after eating food and also 127(55.7%) drunks two to three cups of caffeine containing drinks per day (Table 3).
| Variable |
Category |
Frequency |
Percentage (%) |
| Frequency of food taking per day |
Once per day |
4 |
1.8 |
| Two times per day |
18 |
7.9 |
| Three types per day |
184 |
80.7 |
| Above three times per day |
22 |
9.6 |
| Total |
228 |
100.0 |
| Types of food taken during pregnancy |
Fruit and vegetables |
57 |
25.0 |
| Meat and egg |
34 |
14.9 |
| Injera with shiro |
137 |
60.1 |
| Total |
228 |
100.0 |
| Use of caffeine containing drinks |
Yes |
228 |
100.0 |
| Total |
228 |
100.0 |
| Timing of usage of caffeine containing drinks |
Immediately after eating food |
132 |
57.9 |
| After thirty minutes |
38 |
16.7 |
| After one hour |
16 |
7.0 |
| With food |
42 |
18.4 |
| Total |
228 |
100.0 |
| Number of cups of caffeine containing drinks per day |
1 |
32 |
14.0 |
| 2-3 |
127 |
55.7 |
| ≥4 |
69 |
30.3 |
| Total |
228 |
100.0 |
Table 3: Nutritional characteristics of pregnant mothers attended ANC follow up in Dodola General Hospital, Oromia Region, South East Ethiopia 2018.
Prevalence of Iron deficiency anemia
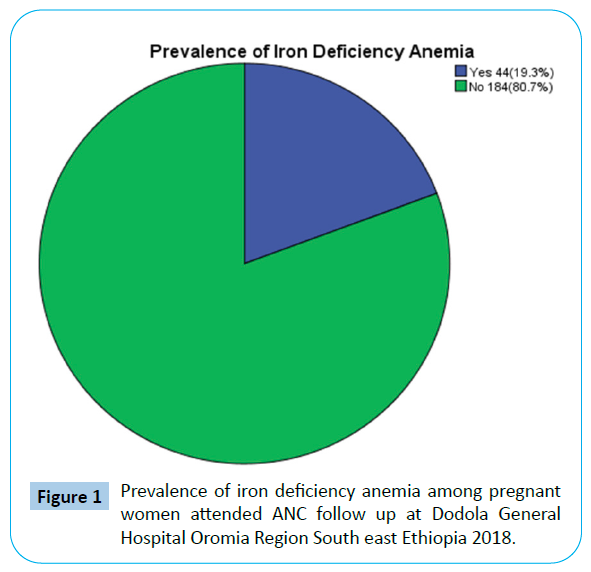
Among the total participants 44(19.3%) has iron deficiency anemia (Figure 1).
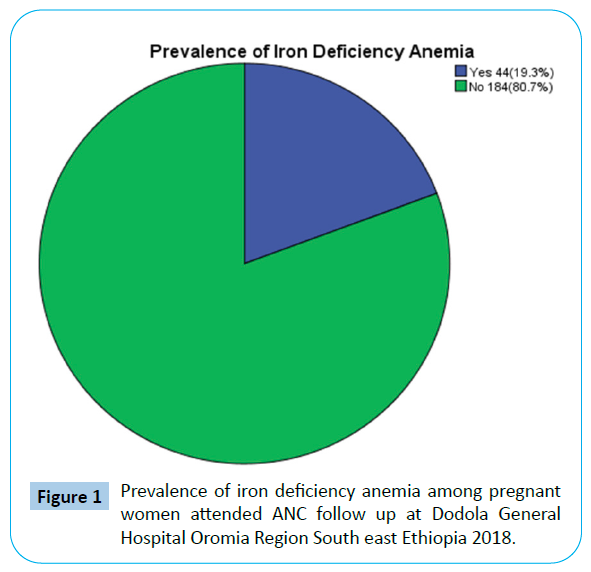
Figure 1: Prevalence of iron deficiency anemia among pregnant women attended ANC follow up at Dodola General Hospital Oromia Region South east Ethiopia 2018.
Factors associated with iron deficiency anemia among pregnant women attended ANC follow up
Bivariate analysis: Bivariate analysis was done to assess any association between individual independent variables and iron deficiency anemia. Binary logistic regression analysis revealed that birth interval, monthly income, residence, bleeding during pregnancy, occupation, meal type, number of ANC visit, caffeine intake, days of iron supplementation and amount of cups of caffeine containing drinks to be significantly associated with (p-value <0.05) iron deficiency anemia (Table 4). But the other independent variables like religion, maternal age, age at first marriage, gestational age, educational status, ethnicity, family size, gravidity, parity, meal frequency, number of fetus in current pregnancy, partner’s educational status as well as occupation doesn’t show any association with iron deficiency anemia.
| Variables |
Category |
IDA |
COR (95%CI) |
P-value |
| Yes |
No |
| Birth interval |
Primigravida |
14 |
42 |
1.883 (1.291-2.746) |
0.001 |
| <2 |
21 |
43 |
0.23 (0.01-2.06) |
| 2-4 |
9 |
79 |
5.3 (0.08-7.15) |
| ≥5 |
0 |
20 |
1.00 |
| Monthly income |
≤1000 |
39 |
86 |
4.433 (2.059-9.546) |
0.000 |
| 1001-1500 |
3 |
62 |
1.05 (0.48-2.27) |
| 1501-2000 |
2 |
24 |
1.15 (0.52-2.53) |
| 2001-2500 |
0 |
7 |
1.03 (0.56-2.23) |
| >2500 |
0 |
5 |
1.00 |
| Residence |
Urban |
23 |
140 |
1.00 |
0.002 |
| Rural |
21 |
44 |
0.344 (1.469- 5.744) |
| Vaginal bleeding during pregnancy |
Yes |
4 |
2 |
9.100 (1.611-51.409) |
0.012 |
| No |
40 |
182 |
1.00 |
| Occupation |
House wife |
34 |
103 |
1.366 (1.077-1.732) |
0.010 |
| Government employee |
3 |
18 |
1.00 |
| Private employee |
2 |
7 |
3.07 (1.30-7.22) |
| Self employed |
1 |
12 |
1.04 (0.78-3.86) |
| Merchant |
3 |
23 |
3.76 (0.61-23.03) |
| Farmer |
1 |
21 |
0.43 (0.66-2.61) |
| Meal type |
Fruit and vegetables |
2 |
55 |
1.00 |
0.000 |
| Meat and egg |
4 |
30 |
0.17 (0.12-7.83) |
| Enjera with shiro |
38 |
99 |
0.318 (0.170- 0.594) |
| Number of ANC visit |
1 |
31 |
31 |
2.413 (1.602-3.634) |
0.000 |
| 2 |
4 |
75 |
1.31 (0.66-2.61) |
| 3 |
3 |
40 |
1.58 (0.78-3.19) |
| 4 |
6 |
22 |
2.01 (0.93-3.31) |
| Above 4 |
0 |
16 |
1.00 |
| Timing of usage of caffeine containing drinks |
Immediately after eating food |
16 |
116 |
1.03 (1.01-3.03) |
0.000 |
| After thirty minutes |
4 |
34 |
0.02 (0.1-1.05) |
| After one hour |
0 |
16 |
1.00 |
| With food |
24 |
16 |
0.490 (0.372-0.644) |
| Days of iron supplementation |
For one month |
7 |
39 |
0.508 (0.396-0.650) |
0.000 |
| For two month |
7 |
79 |
0.33 (0.01-1.31) |
| For three month |
0 |
31 |
0.51 (0.14-2.05) |
| Above three month |
0 |
11 |
1.00 |
| Number of cups of caffeine containing drinks per day |
One |
2 |
30 |
1.00 |
0.000 |
| 2-3 |
10 |
117 |
3.35 (0.85-8.15) |
| ≥4 |
32 |
37 |
0.143 (0.072-0.285) |
| Iron Supplementation during current pregnancy |
Yes |
14 |
160 |
1.00 |
0.000 |
| No |
30 |
24 |
0.070 (0.033-0.151) |
Table 4: Bivariate Logistic Regression analysis of factors associated with iron deficiency anemia among pregnant women attended ANC follow up at Dodola General Hospital Oromia Region South East Ethiopia 2018.
Multivariate Analysis
Factors independently associated with iron deficiency anemia among pregnant women
Binary logistic regression analysis was performed in order to identify factors independently associated with iron deficiency anemia. Eleven (11) factors that associated with iron deficiency anemia at P-value<0.05 during bivariate analysis were subjected all together in a multiple regression analysis these include participant’s; (1) Birth interval, (2) Monthly income, (3) Residence, (4) Vaginal bleeding during pregnancy, (5) Occupation, (6) Meal type, (7) Number of ANC visit, (8) Caffeine intake, (9) Days of iron supplementation, (10) Number of cups of caffeine containing drinks per day, (11) Iron supplementation during the current pregnancy. Up on fitting this factors using binary logistic regression and by specifying “backward LR” methods with removal at P<0.05 after controlling confounders revealed that five (5) variables that are significantly associated with iron deficiency anemia among pregnant women were monthly income [AOR=4.2, 95% CI:1.72-11.01], Number of ANC visit [AOR=0.023, 95% CI: 0.001-0.422], Vaginal bleeding during pregnancy [AOR=9.1, 95% CI: 1.56-24.93], Meal type [AOR=2.45, 95% CI: 1.58-9.81], Timing of usage of caffeine containing drinks [AOR=4.12, 95% CI: 1.78- 12.3] (Table 5).
| Variables |
Category |
IDA |
AOR (95%CI) |
P-value |
| Yes |
No |
| Monthly income |
≤1000 |
39 |
86 |
4.2 (1.72-11.01) |
0.016 |
| 1001-1500 |
3 |
62 |
0.84 (0.06-10.7) |
0.719 |
| 1501-2000 |
2 |
24 |
0.72 (0.52-2.53) |
0.275 |
| 2001-2500 |
0 |
7 |
0.89 (0.48-2.27) |
0.134 |
| >2500 |
0 |
5 |
1.00 |
|
| Number of ANC visit |
1 |
31 |
31 |
0.023 (0.001-0.42) |
0.011 |
| 2 |
4 |
75 |
1.35 (0.70-2.60) |
0.369 |
| 3 |
3 |
40 |
1.02 (0.50-2.12) |
0.941 |
| 4 |
6 |
22 |
0.62 (0.31-1.25) |
0.183 |
| Above 4 |
0 |
16 |
1.00 |
|
| Vaginal bleeding during pregnancy |
Yes |
4 |
2 |
9.1 (1.56-24.93) |
0.012 |
| No |
40 |
182 |
1.00 |
|
| Meal type |
Fruit and vegetables |
2 |
55 |
1.00 |
|
| Meat and egg |
4 |
30 |
2.82 (0.33-24.00) |
0.587 |
| Injera with shiro |
38 |
99 |
2.45 (1.58-9.81) |
0.017 |
| Timing of usage of caffeine containing drinks |
Immediately after meal |
16 |
116 |
2.15 (0.49-5.02) |
0.484 |
| After thirty minutes |
4 |
34 |
2.45 (0.28-20.76 |
0.696 |
| After one hour |
0 |
16 |
1.00 |
|
| With food |
24 |
18 |
4.12 (1.78-12.3) |
0.004 |
Table 5: Multivariate Logistic Regression analysis of factors associated with iron deficiency anemia among pregnant women attended ANC follow up at Dodola General Hospital Oromia Region South East Ethiopia 2018.
This study found that those pregnant women who had monthly income less than or equal to one thousand birr were about 4.2 times more likely to develop iron deficiency anemia [AOR=4.2, 95% CI: 1.72-11.01; p=0.016] compared to those who had monthly income of greater than one thousand birr. Pregnant women who had ANC visit one times during their pregnancy were about 0.023 times more likely to develop iron deficiency anemia [AOR=0.023, 95% CI: 0.001-0.42; P=0.011] compared to those who had ANC visit three times and above. However, those who had ANC visit two times during their pregnancy were less likely to develop iron deficiency anemia. Those women who had history of vaginal bleeding during their pregnancy were about 9.1 times more likely to develop iron deficiency anemia [AOR=9.1, 95% CI: 1.56-24.93; P=0.012] when compared to those who had no history of vaginal bleeding during their current pregnancy time and those women who eats only injera with shiro during their pregnancy were about 2.45 times more likely to develop iron deficiency anemia [AOR=2.45, 95% CI: 1.58-9.81; P=0.017] compared to those who eats vegetables and protein containing foods like meat, egg. Those women who drunks caffeine containing drinks with food during their pregnancy were about 4.12 times more likely to develop iron deficiency anemia [AOR=4.12, 95% CI: 1.78-12.3; P=0.004] when compared to those who drunks caffeine containing drinks after one hour during their pregnancy.
Discussion
This study attempted to assess the prevalence of iron deficiency anemia and associated factors among pregnant women attending Antenatal care follow up at Dodola General Hospital. The overall prevalence of iron deficiency anemia was 19.3%. This finding is relatively high when compared to another study conducted at Gondar University Hospital (16%) [23], and relatively low when compared to another study conducted at Azezo health center (21.6%) [21]. The result of this study is decreased by 38.7% and 37.5% when we compare with another studies conducted in Sub-Saharan Africa (58%) [2], and in the urban area of Eastern Ethiopia 56.8% [18] respectively. The result of this study is relatively low prevalence when compared with a study carried out at Mekelle town, North West Tigray in 2011 showed that the prevalence of iron deficiency anemia was 36.1% [19] and 29% was another study conducted at western region of Ethiopia [20]. Decrease in prevalence of iron deficiency anemia in this study might be due to difference in sample size, study design, socio demographic status and altitude.
In this study, significance association between monthly income and iron deficiency anemia was observed. Those pregnant women who had monthly income less than or equal to one thousand birr were about 4.2 times more likely to develop iron deficiency anemia [AOR=4.2, 95% CI: 1.72-11.01; p=0.016] when compared to those who had monthly income of greater than one thousand birr. The possible explanation for those women who had monthly income less than or equal to one thousand birr might be due to low socioeconomic status of the women, which have impact on their nutritional status and health seeking behaviour. Women in low socio-economic classes are likely to be poorly educated and often have financial constraints. These women cannot afford good health services or they might not have access to health services and also they tend to consume diets that are low in micronutrient, animal protein and phytate which interferes with intestinal uptake of iron that results in the deleterious effects of poor nutrition. This study in lined with a study carried out at Mekelle town, North West Tigray [19].
Pregnant women who had ANC visit one times during their pregnancy were about 0.023 times more likely to develop iron deficiency anemia [AOR=0.023, 95% CI: 0.001-0.42; P=0.011] when compared to those who had ANC visit three times and above. The possible explanation for those women who had ANC visit one times during their pregnancy might be due to mothers are likely to get iron and folic acid supplementation for a shorter duration during pregnancy as compared to those who had ANC visit three times and above. This may have contributed to the high prevalence of iron deficiency anemia recorded in this study.
History of vaginal bleeding during pregnancy is associated with iron deficiency anemia. Those women who had history of vaginal bleeding were 9.1 times more likely to develop iron deficiency anemia than those who had no history of vaginal bleeding during their pregnancy [AOR=9.1, 95% CI: 1.56-24.93; P=0.012]. The possible explanation might be those women who had history of vaginal bleeding during pregnancy are more likely to develop iron deficiency anemia because if the women losses significant amount of blood the body quickly pools water from tissues outside the bloodstream in an attempt to keep the blood vessels filled. As a result the blood is diluted, and the hematocrit level is reduced. Overtime bleeding reduces the amount of iron in the body so that the bone marrow is not able to increase production of new red blood cells to replace the lost [28].
From the present study found that meal type during pregnancy is one of the independent variable which significantly associated with iron deficiency anemia. Those mothers who were eats only injera with shiro were 2.45 times more likely to develop iron deficiency anemia than those who eats vegetables and protein containing foods [AOR=2.45, 95% CI: 1.58-9.81; P=0.017]. The possible explanation is those pregnant women who were eats only injera with shiro were develop iron deficiency anemia because it might be due to lack of contents of iron in the food that they eat only injera with shiro or if the pregnant women eat white teff there is no iron in these injera so that this women is going to loss iron in the food that she take it if so simply she develop iron deficiency anemia.
The last independent variables in this study which can be associated with iron deficiency anemia were taking of caffeine containing drinks with food. Those women who drunken caffeine containing drinks with food were 4.12 times more likely to develop iron deficiency anemia than those who did not drunk caffeine containing drinks during their pregnancy [AOR=4.12, 95% CI: 1.78-12.3; P=0.004]. This study in lined with a study carried out at Mekelle town, North West Tigray [19]. The possible explanation might be those women who had taken caffeine containing drinks with food are more likely to develop iron deficiency anemia is due to caffeine containing drinks inhibit absorption of iron.
However, increased number of pregnancy and delivery has no significant association with iron deficiency anemia in this study. The same finding was observed in a study conducted in Azezo health center this might be due to experience gained from the first pregnancy, the consequent increased awareness, good diet, as well as interaction with other women at the Ante natal clinic.
Strengths of the study
• High respondent rate was achieved.
• The data was collected by the staff members of MCH ward.
• Despite the presence of limitation, this study tries to address important issues in the study area and include several associated factors that affect prevalence of IDA and tried to understand about associated factors of the IDA in the source population based on the findings from the study population.
Limitations of the Study
One of the limitations of this study is the nature of the study design, being as a cross-sectional study design, whereby it may not explain the temporal relationship between the outcome variable and some explanatory variables; this limits interpretation of the estimated associations. There was a social desirability for dietary information and monthly income.
Conclusion
The prevalence of iron deficiency anemia among pregnant women in this study was relatively low. This study revealed that pregnant women who had monthly income less than or equal to one thousand birr, Ante natal care visit one times, history of vaginal bleeding, who eats only injera with shiro and drunks caffeine containing drinks with food during their current pregnancy were significantly associated with iron deficiency anemia among pregnant women.
39617
References
- WHO/UNICEF (2008) Iron deficiency anemia: Assessment, prevention and control: A guide for program managers.
- https://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf
- Pacino MF (2003) Pregnancy and lactation; physiological and sentiment requirements and the role of dietary supplements, INUTR 133: 1997s-2005
- Samson N (2006) Obstetrician and Gynecologist: Obstetrics and Gynecology Lecture Note for Health Science Students. Hawasa University.
- Agarwal AK, Sharma K, Sharma MC, Prasad N, Kumar O (2006) Prevalance of anemia in pregnant and lactating women in India. India J med Res 124: 173-184.
- Rowland TW, Green GM, Kelleher JF (1988) The effect of iron therapy on the exercise capacity of non-anemic iron deficiency runner. Am J Dis Child 142;165-169.
- Sifakis S, Pharmakides G (2000) Anemia in pregnancy. Ann NY Acadsci 900: 125-136.
- Sola MMJ, KinaboJ (1997) Prevalence of anemia in pregnant women during the last trimester. Int J food science Nutrition 48: 265-270.
- American College of Obstetricians and Gynecologists (2008) ACOG Practice Bulletin No. 95: anemia in pregnancy.
- Silvia M, Simpson RJ, Mackie AT (2003) physiology and molecular biology of dietary iron absorption. Annu Rev Nutr 33-283-301.
- Yewelsew A, Alemtsehay B, Michael KH, Barbara JS, Isabel A, et al. (2007) Inadequate intakes of dietary iron among pregnant women from subsistence house –holds in Sidama district, southern Ethiopia. Public Health Nutr 11: 379-386.
- De Maeyer E, Adiels-Tegman M (1985) The prevalence of anemia in the World. 38: 302-316
- https://www.who.int/gho/publications/world_health_statistics/EN_WHS09_Full.pdf
- https://apps.who.int/disasters/repo/13849_files/i/nutrition_health_development.pdf
- Awan M, Akbar M, Khan M (2004) study of anemia in pregnancy women of rail colony Multan Pakistan J Med Res 43: 11-14.
- Kefyalew A, Abdullah M (2014) Prevalence of Anemia and associated factors among pregnant women in an urban area of Eastern Ethiopia. Anemia 2014.
- Abel G, Afework M (2015) Prevalence of Anemia and associated factors among pregnant women in north western zone of Tigray, northern Ethiopia. J Nutr Metab 2015: 165430.
- Eyasu E, Birhan A, Eshetu F, Merga F, Tadesse B (2014) Prevalence of Anemia in pregnant women and associated factors in western Ethiopia. Food sci quality manag 31: 2014
- Meseret A, Bamlaku E, Aschalew G, Tigist K, Mohammed S, et al. (2013) Prevalence of Anemia and associated risk factors among pregnant women attending antenatal care in Azezo health center Gondar town, Northwest Ethiopia.
- Mulugeta M, Aster A (2015) Maternal Anemia during pregnancy in Bahr Dar town.
- Mulugeta M, Zelalem A, Meseret A, Bamlaku E (2014) Prevalence of iron deficiency anemia and associated factors among pregnant women attending antenatal care follow up in Gondar University Hospital Northwest Ethiopia.
- Harrell RE (1997) Preventing iron deficiency through fortification. Nutrition Rev 55: 210-222.
- Aunt, JR, Gallagher Sk, Hanson LK (1994) effects of ascorbic acid on apparent iron absorption by women with low iron stores, Am J Clinical Nutrition 59: 1381-1385.
- Nero T, Jate L, Tew KD (2001) Iron deficiencies and requirements. Biomed Pharamactother 55: 324-332.
- Blot I, Diallo D, chermia TJ (1999) iron deficiency in pregnancy: effects on new born. Curropin Hematol 6: 65-70.
- Mihrete H, Fufa M, Mitiku A, Bacha C, Getahun D, et al. (2015) Magnitude of Anemia and associated factors among pregnant women attending antenatal care in Nekemte Health Center, Nekemte, Ethiopia.
- Nwizu EN, Ibrahim SA, Gala HS (2011) Socio demographic and maternal factors in Anemia in pregnancy at Booking in Kano, Northern Nigeria. Afr J Reprod Health 2011: 15: 33-41.
- Kalaivani K (2009) Prevalence and consequence of anemia in pregnancy. Indian J Med Res 99: 627-633.
- Center for Disease Control and Prevention (1998) Recommendation to prevent and control iron deficiency anemia in the United States, center for disease control and prevention. MMWRR Recommendation Rep 47: 1-29.
- Cops well ME, Parvanta E, Acres L, Yip R, Britten Han GM (2003) Iron supplementation during pregnancy, anemia and birth weight a randomized controlled trial. Am J Clin Nutr 78: 773-81
- YIPR Karl B, Baileys, Rosalind S (1996) The utility of comparinces of hemoglobin distribution. In: iron nutrition in health and disease. London. Hall berg L, ASPN Cr (eds), HohnLibby. pp: 31-38
- Ethiopia Central Statistical Agency (2011) Ethiopia demographic and health survey 2005: preliminary report. Central Statistical Agency, Addis Ababa, Ethiopia. PP: 156-157.