Keywords:
Metabolic syndrome; Primary care center; Heart attack; Hyperglycemia; Hypertension; Hyperuricemia
Introduction
Background
At the beginning of the twentieth century, Kylin, a Swedish physician detected the aggregation of multiple cardiovascular risk factors when he came up with the description of a syndrome that involving hypertension, hyperglycemia and hiperuricemia [1]. In the 1940s, Dr. Jean Vague, a French clinician wrote out about abdominal obesity and fat distribution and its relation to diabetes and other disorders [2]. In 1965, an abstract was revealed at the European Association for the Study of Diabetes annual meeting by Avogaro and Crepaldi, which described a syndrome comprised hypertension, hyperglycaemia, and obesity [3]. In 1988, Gerry Reaven described a cluster of risk factors for diabetes and cardiovascular disease and demonstrated as ‘Syndrome X’. His main contribution was the introduction of the concept of insulin resistance [4,5]. His main contribution was the introduction of the concept of insulin resistance. In 1989, the syndrome was reintroduced by Kaplan as ‘The Deadly Quartet’ and in 1992 it was again renamed ‘The Insulin Resistance Syndrome’ [6]. At the present time, it was agreed that the well-established term ‘Metabolic syndrome’ remains the most usual description of this cluster of metabolic abnormalities [7].
There are several definitions for the metabolic syndrome. The National Cholesterol Education Program (NCEP/ATP III) and International Diabetes Federation (IDF) definitions are the most widely used. Current ATP III criteria define the metabolic syndrome as the presence of any three of the following five traits:
Abdominal obesity, defined as a waist circumference in men >102 cm and in women >88 cm. Serum triglycerides ≥ 150 mg/dL (1.7 mmol/L). Serum HDL cholesterol <40 mg/dL (1 mmol/L) in men and <50 mg/dL (1.3 mmol/L) in women. Blood pressure ≥130/85. Fasting plasma glucose (FPG) ≥110 mg/dL (5.6 mmol/L) [8].
IDF proposed a set of metabolic syndrome criteria in 2004. Central obesity is an essential element in this definition, with different waist circumference thresholds set for different race/ ethnicity groups:
Waist circumference in men ≥ 94 cm and in women ≥ 80 cm, this is for Europe’s people. For the Eastern Mediterranean and Middle East (Arab) populations, they recommend using European data until data that are more specific are available. MOREOVER, any two of the following:
Triglycerides ≥ 150 mg/dL (1.7 mmol/L) or treatment for elevated triglycerides. HDL cholesterol <40 mg/dL (1.03 mmol/L) in men or <50 mg/dL (1.29 mmol/l) in women, or treatment for low HDL. Systolic blood pressure ≥ 130, diastolic blood pressure ≥85, or treatment for hypertension. Fasting plasma glucose ≥ 100 mg/ dL (5.6 mmol/L), or previously diagnosed type 2 diabetes. An oral glucose tolerance test is recommended for patients with elevated fasting plasma glucose, but not required.
The prevalence of the metabolic syndrome in Member States of the Gulf Cooperative Council (GCC; Bahrain, Kuwait, Oman, Qatar, Saudi Arabia and the United Arab Emirates)-countries ranged from 20.7% to 45.9% [9]. People with Metabolic syndrome are twice as likely to die from and three times as likely to have a heart attack or stroke compared with people without the síndrome [10]. In addition, almost 200 million people globally have diabetes and 80 percent of these will die from cardiovascular disease, so there is an overwhelming moral, medical and economic imperative to identify those individuals with metabolic syndrome early, so that lifestyle interventions and treatment may prevent the development of diabetes and/or cardiovascular disease.
Clinical outcomes of metabolic syndrome
ATP III viewed CVD as the primary clinical outcome of metabolic syndrome. Most individuals who develop CVD have multiple risk factors and most individuals with this syndrome have insulin resistance, which grants increased risk for type 2 diabetes. When diabetes becomes clinically obvious, CVD risk rises severely. Beyond CVD and type 2 diabetes, individuals with metabolic syndrome seemingly are susceptible to other conditions, notably polycystic ovary syndrome, fatty liver, cholesterol gallstones, asthma, sleep disturbances, and some for metabolic syndrome of cáncer [11].
Pathogenesis of metabolic syndrome
The Metabolic syndrome seems to have some potential etiological categories like obesity and abnormal body fat distribution, insulin resistance and other contributing factors like progressing age which probably affects all levels of pathogenesis, which likely explains why prevalence of the metabolic syndrome rises with progressing age [12]. Of late, a pro-inflammatory state has been implicated directly in causation of insulin resistance, as well as atherogenesis. As a final point, several endocrine factors have been associated with abnormalities in body-fat distribution and hence indirectly to metabolic syndrome. Thus, pathogenesis of the metabolic syndrome is complex and ripe with opportunities for further research [11].
Therapeutic implications
Regardless of diagnostic criteria used, there is full agreement that therapeutic lifestyle change, with emphasis on weight reduction, constitutes first-line treatment for metabolic syndrome. Drug treatment to directly reduce insulin resistance is promising, but clinical trials to prove reduction of CVD are lacking. In patients in whom lifestyle changes fail to reverse metabolic risk factors, consideration should be given to treating specific abnormalities in these risk factors with drugs. Use of drugs to target risk factors should be in accord with current treatment guidelines [11].
Rationale
1. During working in general clinics at King Fahed Armed Forces Hospital (KFAFH), I noticed that no physician labels obese, diabetic and hypertensive patients as having metabolic syndrome despite their large number. Therefore, I was wondering about the prevalence of metabolic syndrome.
2. Some family members asked me how common metabolic syndrome is in our community.
3. No study done in KFAFH, Jeddah.
Aim
To determine the magnitude of the problem of metabolic syndrome as a health burden in KFAFH, Jeddah, 2012.
Objectives
1. To estimate the prevalence of metabolic syndrome among primary health care attendees in KFAFH in Jeddah 2012.
2. To compare prevalence of metabolic syndrome using ATP III and IDF definition in primary health care attendees in KFAFH in Jeddah 2012.
3. To estimate the prevalence of each criterion used in the definition of metabolic syndrome in primary health care attendees in KFAFH in Jeddah 2012.
4. To identify associated factors with metabolic syndrome in primary health care attendees in KFAFH in Jeddah 2012.
Literature Review
Several studies conducted to estimate prevalence of metabolic syndrome. One study conducted among US adults to estimate prevalence of the metabolic syndrome using ATP III criteria. It involves 8814 men and women aged 20 years or older from the Third National Health and Nutrition Examination Survey (1988 to 1994). The results showed the unadjusted and age-adjusted prevalence of the metabolic syndrome were 21.8% and 23.7%, respectively. The prevalence increased from 6.7% among participants aged 20 through 29 years to 43.5% and 42.0% for participants aged 60 through 69 years and aged at least 70 years, respectively. The age-adjusted prevalence was similar for men (24.0%) and women (23.4%) [13].
In Northwest Russia in 2000, study conducted in involving 3705 Russian adults aged 18-90 years. The results showed that the agestandardized prevalence rates of the metabolic syndrome among women were 19.8% using NCEP, 20.6% using AHA/NHLBI and 23.1% using IDF criteria. The corresponding rates for men were 11.5% using NCEP, 13.7% using AHA/NHLBI and 11.0% using IDF criteria. Among subjects with metabolic syndrome, central obesity was more common among women, while elevated triglycerides and blood glucose were more common among men [13].
Another study conducted in Spain (Madrid). It was cross-sectional study, involving 1344 people aged 31 to 70 years. ATP III and IDF criteria used. The age- and sex-adjusted prevalence of metabolic syndrome was 24.6% using the ATP III definition and 30.9% using the IDF definition. Prevalence figures by both definitions were higher in men than in women and increased with age [14].
One study conducted in china involving 1206 people and by using ATP III criteria, the prevalence of metabolic syndrome was 26.7%, and the prevalence of hypertension and diabetes were 38.0% and 4.3% respectively [15].
Another study was conducted in Malaysia involving 4341 people from Peninsular and East Malaysia with the result based on the WHO, ATP III, and IDF, the overall crude prevalence of Metabolic syndrome were 32.1%, 34.3%, 37.1%, respectively. Regardless of the criteria used, metabolic syndrome was higher in urban areas, in females, in the Indian population, and increased significantly with age. Risk factors also increased with age; abdominal obesity was most prevalent (57.4%), was higher in females (64.2%) and was highest in Indians (68.8%). Hypertension was higher in males (56.5%) and highest among Malaysians (52.2%). In contrast, the Chinese had the highest prevalence of hypertriglyceridemia (47.4%) [16].
One systematically review study documenting the prevalence of the metabolic syndrome among men and women in Member States of the Gulf Cooperative Council (GCC; Bahrain, Kuwait, Oman, Qatar, Saudi Arabia and the United Arab Emirates) countries in which obesity, Type 2 diabetes and related metabolic and cardiovascular diseases are highly prevalent. Its results showed that for men, the prevalence of the metabolic syndrome ranged from 20.7% to 37.2% (ATPIII definition) and from 29.6% to 36.2% (IDF definition) and for women, from 32.1% to 42.7% (ATPIII definition) and from 36.1% to 45.9% (IDF definition). Overall, the prevalence of the metabolic syndrome in the GCC states is some 10 to 15% higher than in most developed countries, with generally higher prevalence rates for women [9].
There are studies conducted in Saudi Arabia, like study conducted by Al-Nozha, it was community-based national epidemiological health survey and part of Coronary Artery Disease in Saudi Study (CADISS). It involves 17,293 people in the age group of 30-70 years of selected households over a 5-year period between 1995 and 2000 in Saudi Arabia. This study showed that the overall ageadjusted prevalence of metabolic syndrome in Saudi Arabia was 39.3%. Age adjusted prevalence in males is 37.2%, while females have a higher prevalence of 42%. Saudi subjects from urban areas have significantly higher prevalence of 44.1% compared to those living in rural areas of 35.6%. Low HDL affects 81.8% of females and 74.8% of males with metabolic syndrome leading all other factors, and it continued to be consistent in all different age groups [17].
In Riyadh, another study conducted and published online in 2010 August 13, it was cross sectional study involving 2,850 Saudi adults aged 18 to 55 years. This study showed that the overall prevalence of metabolic syndrome was 35.3%. Age-adjusted prevalence according to the European standard population is 37.0%. Low HDL-cholesterol was the most prevalent of all metabolic syndrome risk factors, affecting subjects [18].
In 2004 in primary care setting in Northern Area Armed Forces Hospital, King Khalid Military City, Hafr Al-Batin. A study conducted; it involves about 2250 Saudi male soldiers aged 20- 60 years residing in a military city in Northern Saudi Arabia. The result was: age-adjusted prevalence of metabolic syndrome was found to be 20.8%. Abdominal obesity was the most common component in the study population (33.1%) closely followed by raised serum triglycerides (32.2%) and elevated systolic blood pressure (29.5%). Over two-thirds of the subjects (71%) exhibited at least one criterion for metabolic syndrome. Prevalence of individual factors and mean values of the components of the syndrome showed a steady increase with increase in age and body fat.
In addition, another study conducted in Northern Area Armed Forces Hospital, King Khalid Military City, Hafr Al-Batin involving 2577 non-pregnant Saudi women aged 18-59 years. The result was: Age-adjusted prevalence of metabolic syndrome was found to be 16.1% and 13.6% by IDF and NCEP-ATPIII definitions, respectively. Abdominal obesity was the most common component in the study population (44.1% by NCEP-ATPIII and 67.9% by IDF cut-off points). It followed by low serum high-density lipoprotein cholesterol (36.0%). About two-thirds of the subjects (66.4% by NCEP-ATPIII and 67.9% by IDF definitions) exhibited at least one criterion for metabolic syndrome by both definitions. Mean values and prevalence of individual components of the syndrome showed a steady rise with increase in age, general and abdominal obesity, and the presence of diabetes. Since the cut-off, values for waist circumference by IDF definition were lower, prevalence rates by this definition were higher than those defined by NCEP-ATPIII [19].
Methodology
Study Design
Cross-sectional study.
Study area
Jeddah is a Saudi city located in the middle of the Eastern coast of the Red Sea known as the 'Bride of the Red Sea' and is considered the economic and tourism capital of the country. Its population is estimated around 3.4 million and it is the second largest city after Riyadh [20].
Study setting
It conducted in primary care center in KFAFH.
Primary care center has two sections, the male section and the female section, each section has its own reception, registry system and working hours. The working hours in the male section start from 7:30 AM to 4:00 PM then from 4:00 PM to 12:00 AM. The working hours in the female section start from 7:30 AM - 3:00 PM then from 3:00 PM to 9:00 PM.
Estimated number of patients attending primary care center in the morning shift in both sections is about 900-1000 patients. In the evening shift is around 400-500 patients.
In one month, the average attending of the patients is around 35000-40000.
Study population
Peoples who attended primary care center in KFAFH in 2012. An inclusion criterion was age 20 years and over. An exclusion criterion was pregnant females.
Sampling
Estimated sample size was 300 peoples calculated by Epi info program using the prevalence of 13%, and 95% confidence.
Sample technique
It was chosen by systematic random sample after registration in the computer system. The first patient selected randomly from the first 10 patients, and then every 10th patient chosen. Patients selected proportionally from both shifts (morning and evening). 200 patients from the morning shift and 100 patients from the evening shift selected.
Data Collection Tool
Data Collection sheet, which includes three parts. First part: socio-demographic data. Second part: check list about smoking habit (smoking cigarette or shisha, exsmoker defined as quit smoking for more than one year), physical activity (defined as doing regular exercise for 5, 3 or one day per week for 30 minute), past history of diabetes and hypertension, any medication for the treatment of diabetes, hypertension or dyslipidemia. Third part: Results of measurement: including measurement BP, BMI, waist circumference, fasting blood glucose and fasting HDL, triglycerides, cholesterol.
NCEP/ATP III and IDF definitions utilized to determine the criteria to diagnose metabolic syndrome. ATP III criteria define the metabolic syndrome as the presence of any three of the following five traits: Abdominal obesity, defined as a waist circumference in men >102 cm and in women >88 cm. Serum triglycerides ≥ 150 mg/dL (1.7 mmol/L). Serum HDL cholesterol <40 mg/dL (1 mmol/L) in men and <50 mg/dL (1.3 mmol/L) in women. Blood pressure ≥ 130/85. Fasting plasma glucose (FPG) ≥ 110 mg/dL (6.1 mmol/L) [8].
IDF criteria include waist circumference (as an essential criteria) in men ≥ 94 cm and in women ≥80 cm, PLUS any two of the following:
Triglycerides ≥ 150 mg/dL (1.7 mmol/L) or treatment for elevated triglycerides. HDL cholesterol <40 mg/dL (1.03 mmol/L) in men or <50 mg/dL (1.29 mmol/l) in women, or treatment for low HDL. Systolic blood pressure ≥ 130, diastolic blood pressure ≥ 85, or treatment for hypertension. Fasting plasma glucose ≥ 100 mg/ dL (5.6 mmol/L), or previously diagnosed type 2 diabetes. An oral glucose tolerance test recommended for patients with elevated fasting plasma glucose, but not required.
Data collection technique
The researcher met the patient in private room to explain the aim and the importance of this research, and how this research will be carried out. In addition, he explained to the patient that if there is no result of fasting lipid profile and fasting blood glucose done in the last 6 month, he will need to take fasting blood sample to measure the fasting blood glucose and fasting lipid profile. Once the patient agreed, he signed a written consent.
Through workshop, the researcher trained four nurses who assigned to cover both shifts and both sections, about how to measure the waist circumference and blood pressure. Waist circumference measured by locating top of right iliac crest and then places a measuring tape in a horizontal plane around abdomen at level of iliac crest. Tape measure was parallel to floor and not compressing the skin. Measurement was done at the end of a normal expiration [21]. Patient should not smoke or take caffeine one hour before measuring BP. Patient set for 5 minute in quiet room. BP measured while the patient sitting with the back supported and legs uncrossed. Appropriate cuff size chosen and the arm supported to the heart level and not covered with clothes. BP was measured using automatic BP measuring device. The height and weight were measured with light clothes and no shoes and BMI was calculated by dividing weight in kilograms (kg) by height in meter squared (m²) (kg/m²).
Then went to the lab where the blood sample for glucose, HDL, total cholesterol and triglycerides, taken by a nurse. Patient was fasting for 12 hours. If the patient is not fasting, he/she was given an appointment in the next day to do the investigations.
All of these measurements were filled in the data collection sheet by the researcher. For the lab result, it was taken from the computer system once it is available. After that, it was collected by the researcher and then entered to a personal computer.
Data entry and analysis
Data collected and analyzed using SPSS version 16. Univariate analysis: Continuous variables presented as mean and standard deviation (SD). Categorical variables presented as frequency and percentage. Bivariate analysis: Chi square test applied to test for association and/or difference between categorical variables and student’s t test applied for comparisons of the means of two continuous variables. Multivariate analysis: regression analysis used to adjust for confounding factors. Significance was determined at p value < 0.05 and 95% confidence Interval.
Results
Characteristics of the study population
Table 1 shows that the study included 300 patients. Their age ranged between 20 and 82 years with mean ages of males and females were 51.3 ± 14.8 and 48.6 ± 12.4 years, respectively. The prevalence of DM among male patients was 36.7% compared to 32.7% of females. The prevalence of hypertension among male patients was higher than among female patients (37.37% vs. 33.37%). The prevalence of obesity was higher among female patients than male patients (68% vs. 44.7%). The prevalence of smoking and ex smoking were higher among male than female patients were (9.3% and 20.7% vs. 1.7% and 0%). The prevalence of physical inactivity was higher among female than male patients (34.3%vs. 30.3%).
| Variables |
Male No. (%) |
Female No. (%) |
| Sex (n=300) N (%) |
150 (50%) |
150 (50%) |
| DM (n= 104) N (%) |
55 (36.7%) |
49 (32.7%) |
| HTN (n=106) N (%) |
56 (37.3%) |
50 (33.3%) |
| Obesity (n=169) N (%) |
67 (44.7%) |
102 (68.0%) |
| N (%) |
|
| Smoking history (n=300) |
| Smoker N (%) |
28 (18.6%) |
5 (3.4%) |
| Non-smoker N (%) |
60 (40.0%) |
145 (96.6%) |
| Ex-smoker N (%) |
62 (41.4%) |
0 (0.0%) |
| Physical activity per week (n=300) |
| Regular activity for 30 minutes for 5 days N (%) |
23 (15.3%) |
21 (14.0%) |
| Regular activity for 30 minutes for 3 days N (%) |
17 (11.3%) |
12 (8.0%) |
| Regular activity for 30 minutes for 1 days N (%) |
19 (12.7%) |
14 (9.4%) |
| No regular activity N (%) |
91 (60.7%) |
103 (68.6%) |
Table 1: Characteristics of the study populations.
Prevalence of metabolic syndrome
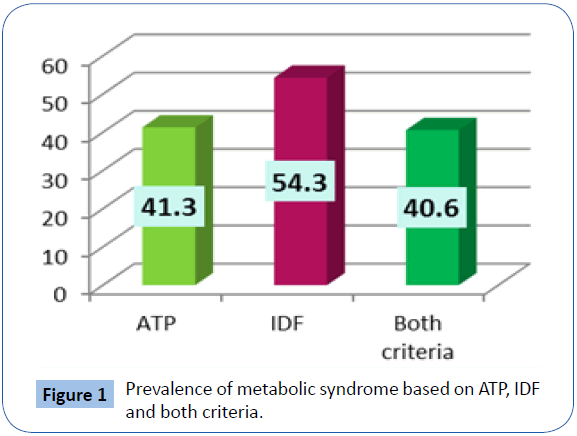
The prevalence of metabolic syndrome among study population, based on ATP criteria was 41.3% while its prevalence was 54.3% based on IDF criteria (Table 2). Based on both criteria, the prevalence was 40.6% (Figure 1).
| Metabolic syndrome |
Metabolic syndrome |
| Yes N (%) |
No N (%) |
| ATP |
124 (41.3%) |
176 (58.7%) |
| IDF |
144 (54.3%) |
121 (45.7%) |
| Both criteria |
122 (40.6) |
178 (59.4) |
Table 2: Prevalence of Metabolic syndrome by ATP and IDF and both criteria.
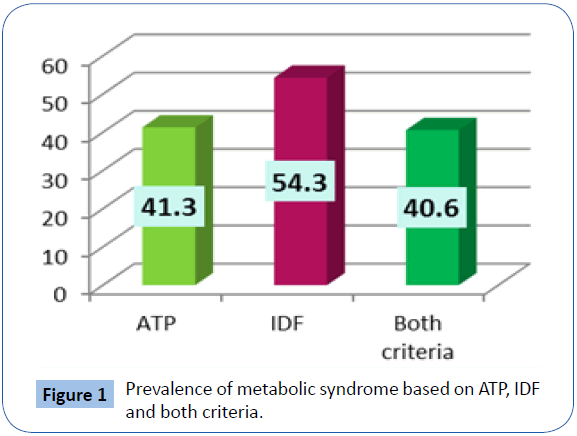
Figure 1: Prevalence of metabolic syndrome based on ATP, IDF and both criteria.
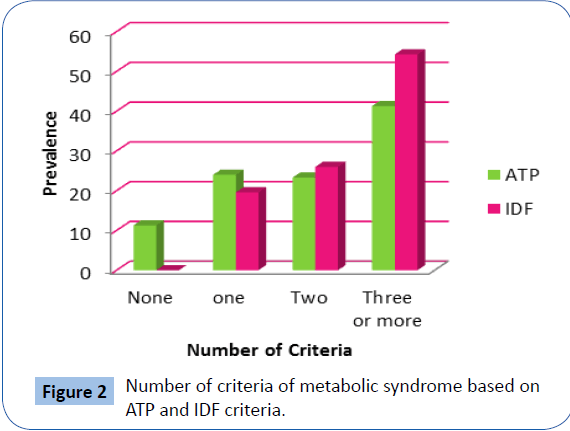
Figure 2 demonstrates the number of criteria of metabolic syndrome by ATP and IDF criteria separately.
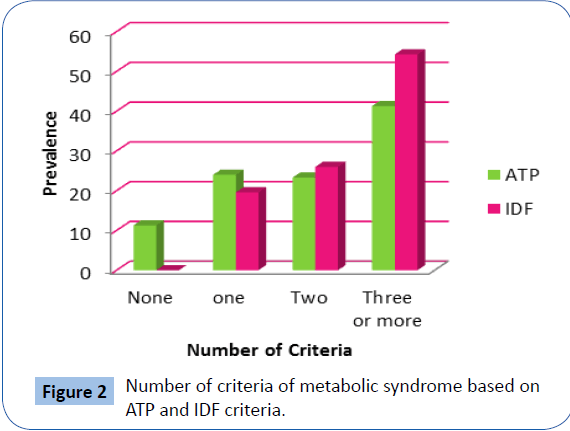
Figure 2: Number of criteria of metabolic syndrome based on ATP and IDF criteria.
Prevalence of metabolic syndrome according to ATP criteria
Table 3 shows that the prevalence of metabolic syndrome based on ATP criteria among diabetic patients was “77 (74%)” while its prevalence among non-diabetic patients was “47 (24%)”. This difference was statistically significant, p=0.001. The prevalence of metabolic syndrome based on ATP among obese patients was “81 (48%)” while it was “43 (32.8%)” among non-obese patients. The prevalence of metabolic syndrome among male was “64 (42.6%)” compared to “60 (40%)” among females with no statistically significant difference.
| Variables |
ATP |
| Yes N (%) |
No N (%) |
| DM |
| Yes (n=104) |
77 (74) |
27 (26) |
| No (n=196) |
47 (24) |
149 (76) |
| p-value=0.001 |
| Obesity |
| Yes (n=169) |
81 (48) |
88 (52) |
| No (n=131) |
43 (32.8) |
88 (67.2) |
| p-value=0.006 |
| Gender |
| Male (n=150) |
64 (42.6) |
86 (57.4) |
| Female (n=150) |
60 (40) |
90 (60) |
| p-value=0.36 |
Table 3: Prevalence of metabolic syndrome according to ATP among participants according to DM, obesity and gender.
Prevalence of metabolic syndrome according to ID criteria
Table 4 shows that the prevalence of metabolic syndrome among diabetic patients was “84 (84.8%)”, based on IDF criteria while its prevalence among non-diabetic patients was “60 (36.1%)”. This difference was statistically significant, p=0.001. The prevalence of metabolic syndrome among obese patients was “91 (54.2%)”, based on IDF while it was “53 (54.6%)” among non-obese patients. The prevalence of metabolic syndrome among male was “76 (60.8%)” compared to “68 (48.5%)” among females. This difference was statistically significant, p=0.03.
| Variables |
IDF |
| Yes N (%) |
No N (%) |
| DM |
| Yes (n=99) |
84 (84.8) |
15 (15.2) |
| No (n=166) |
60 (36.1) |
106 (63.9) |
| p-value=0.001 |
| Obesity |
| Yes (n=168) |
91 (54.2) |
77 (45.8) |
| No (n=97) |
53 (54.6) |
44 (45.4) |
| p-value=0.52 |
| Gender |
| Male (n=125) |
76 (60.8) |
49 (57.4) |
| Female (n=140) |
68 (48.5) |
72 (51.5) |
| p-value=0.03 |
Table 4: Prevalence of metabolic syndrome according to IDF criteria according to DM, obesity and gender.
Comparison between different measures according to presence of metabolic síndrome
1. Using ATP criteria: As illustrated in Table 5, there was a statistically significant difference between patients with metabolic syndrome and those without metabolic syndrome, based on ATP criteria regarding their weight (84.67.26 ± 15.36 vs. 79.4.08 ± 17.6 kg), BMI (32.88 ± 5.8 vs. 30.68 ± 6.31 Kg/m2), systolic BP (135.27 ± 15.19 vs. 120.39 ± 16.55 mmHg), diastolic blood pressure (79.03 ± 10.9 vs. 73.2 ± 11.68 mmHg), waist circumference (106.46 ± 10.28 vs. 97.69 ± 15.18), Fasting blood sugar (7.87 ± 3.4 vs. 5.18 ± 1.61 mmol/L), HDL (1.07 ± 0.25 vs. 1.34 ± 0.33 mg/dL ) and triglycerides (1.73 ± 0.64 vs. 1.15 ± 0.52 mg/dL). There were no statistically significant difference between them regarding their height, cholesterol, and LDL.
| Categories |
Metabolic syndrome according to ATP criteria |
Mean Difference |
95% CI |
P value |
| Yes |
No |
|
| Mean |
Std. Deviation |
Mean |
Std. Deviation |
|
| Height (cm) |
160.68 |
10.4 |
161.11 |
9.8 |
-0.42 |
-2.77 |
1.91 |
0.721 |
| Weight (KG) |
84.67 |
15.36 |
79.4 |
17.6 |
5.27 |
1.5 |
9.03 |
0.006 |
| BMI |
32.88 |
5.8 |
30.68 |
6.31 |
2.2 |
0.81 |
3.95 |
0.002 |
| Systolic BP |
135.27 |
15.19 |
120.39 |
16.55 |
14.88 |
11.24 |
18.52 |
0.0001 |
| Diastolic BP |
79.03 |
10.9 |
73.2 |
11.68 |
5.82 |
3.23 |
8.42 |
0.0001 |
| Waist Circumference (cm) |
106.46 |
10.28 |
97.69 |
15.18 |
8.77 |
5.87 |
11.66 |
0.0001 |
| FBS (mmol/L) |
7.87 |
3.4 |
5.18 |
1.61 |
2.69 |
2.04 |
3.34 |
0.0001 |
| Cholesterol (mmol/L) |
5.1 |
1.08 |
4.91 |
1 |
0.19 |
-0.45 |
0.44 |
0.11 |
| HDL (mmol/L) |
1.07 |
0.25 |
1.34 |
0.33 |
-0.27 |
-0.33 |
-0.2 |
0.0001 |
| LDL (mmol/L) |
3.13 |
0.97 |
2.96 |
0.93 |
0.17 |
-0.05 |
0.39 |
0.132 |
| TG (mmol/L) |
1.73 |
0.64 |
1.15 |
0.52 |
0.57 |
0.43 |
0.71 |
0.0001 |
Table 5: Comparison of different measures used in this research according to presence of metabolic syndrome bases on ATP criteria.
2. Using IDF criteria: As illustrated in Table 6, there was a statistically significant difference between patients with metabolic syndrome and those without metabolic syndrome, based on ATP criteria regarding their weight (84.67.26 ± 15.36 vs. 79.4.08 ± 17.6 kg), BMI (32.88 ± 5.8 vs. 30.68 ± 6.31 Kg/m2), systolic BP (135.27 ± 15.19 vs. 120.39 ± 16.55 mmHg), diastolic blood pressure (79.03 ± 10.9 vs. 73.2 ± 11.68 mmHg), waist circumference (106.46 ± 10.28 vs. 97.69 ± 15.18), Fasting blood sugar (7.87 ± 3.4 vs. 5.18 ± 1.61 mmol/L), HDL (1.07 ± 0.25 vs. 1.34 ± 0.33 mg/dL ) and triglycerides (1.73 ± 0.64 vs. 1.15 ± 0.52 mg/dL). There were no statistically significant difference between them regarding their height, cholesterol, and LDL.
| Categories |
Metabolic syndrome according to IDF criteria |
Mean Difference |
95% CI |
P value |
| Yes |
No |
| Mean |
Std. Deviation |
Mean |
Std. Deviation |
| Height (cm) |
160.92 |
10.65 |
160 |
8.99 |
0.91 |
-1.46 |
3.29 |
0.449 |
| Weight (Kg) |
84.39 |
15.07 |
83.48 |
17.28 |
0.89 |
-3.07 |
4.85 |
0.658 |
| BMI |
32.69 |
5.74 |
32.55 |
5.73 |
0.13 |
-1.25 |
1.52 |
0.85 |
| Systolic BP |
134.73 |
15.51 |
118.87 |
15.96 |
15.86 |
12.03 |
19.68 |
0.0001 |
| Diastolic BP |
78.97 |
10.81 |
72.58 |
9.71 |
6.38 |
3.9 |
8.87 |
0.0001 |
| Waist Circumference (cm) |
106.02 |
10.38 |
101.73 |
13.72 |
4.29 |
1.3 |
7.28 |
0.005 |
| FBS (mmol/L) |
7.67 |
3.25 |
5.08 |
1.65 |
2.58 |
1.97 |
3.19 |
0.0001 |
| Cholesterol (mmol/L) |
5.06 |
1.07 |
4.89 |
0.98 |
0.17 |
-0.07 |
0.42 |
0.164 |
| HDL (mmol/L) |
1.1 |
0.27 |
1.38 |
0.3 |
-0.27 |
-0.34 |
-0.2 |
0.0001 |
| LDL (mmol/L) |
3.08 |
0.97 |
2.95 |
0.91 |
0.13 |
-0.09 |
0.35 |
0.263 |
| TG (mmol/L) |
1.66 |
0.64 |
1.08 |
0.47 |
0.57 |
0.44 |
0.71 |
0.0001 |
Table 6: Comparison of different measures used in this research according to presence of metabolic syndrome bases on IDF criteria.
As shown in Table 7, there was a statistically significant difference between normal patients, those having metabolic syndrome according to one criteria and patients with metabolic syndrome according to both criteria regarding their weight, BMI, systolic blood pressure, diastolic blood pressure, waist circumference, fasting blood glucose, HDL and serum triglycerides. There were no statistically significant difference between them regarding their height, cholesterol and LDL.
| Categories |
Normal |
One criteria |
Both criteria |
P value |
| Mean |
Std. Deviation |
Mean |
Std. Deviation |
Mean |
Std. Deviation |
| Height (cm) |
160.97 |
9.53 |
161.77 |
11.26 |
160.71 |
10.48 |
0.89 |
| Weight (Kg) |
79.28 |
17.95 |
78.17 |
16.41 |
85.13 |
14.98 |
0.01 |
| BMI |
30.68 |
6.39 |
29.95 |
6.24 |
33.05 |
5.66 |
0.003 |
| Systolic BP |
118.86 |
16.02 |
130.79 |
15.9 |
135.39 |
15.28 |
0.0001 |
| Diastolic BP |
72.53 |
11.75 |
77.38 |
9.96 |
79.16 |
10.94 |
0.0001 |
| Waist Circumference (cm) |
97.08 |
15.59 |
100.83 |
11.45 |
106.75 |
10.09 |
0.0001 |
| FBS (mmol/L) |
5 |
1.53 |
6.44 |
1.58 |
7.89 |
3.42 |
0.0001 |
| Cholesterol (mmol/L) |
4.91 |
1.01 |
4.92 |
0.92 |
5.1 |
1.09 |
0.32 |
| HDL (mmol/L) |
1.35 |
0.33 |
1.25 |
0.31 |
1.07 |
0.25 |
0.0001 |
| LDL (mmol/L) |
2.97 |
0.93 |
2.89 |
0.92 |
3.12 |
0.98 |
0.32 |
| TG (mmol/L) |
1.12 |
0.51 |
1.48 |
0.66 |
1.71 |
0.64 |
0.0001 |
Table 7: Comparison of different measures used in this research according to presence of metabolic syndrome bases on IDF, ATP criteria or both.
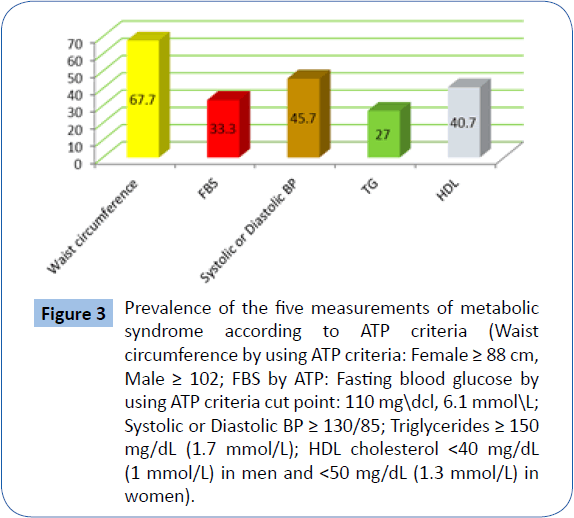
As Shown in Figure 3, waist circumference was above normal in 67.7% of the participants according to ATP criteria (88 cm for males and 102 cm for males). Fasting blood glucose was above normal (6.1 mmol/L) among one third of the participants (33.3%) according to ATP criteria. Systolic and/or diastolic blood pressure was above normal among 45.7% of the participants, triglycerides was above normal among 27% of the participants while HDL was less than normal among 40.7% of them.
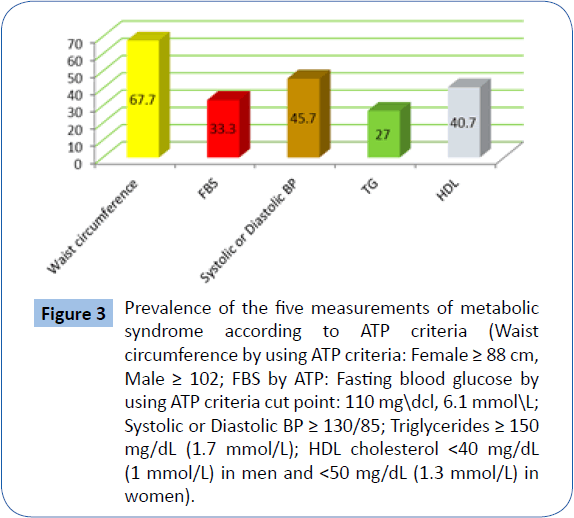
Figure 3: Prevalence of the five measurements of metabolic syndrome according to ATP criteria (Waist circumference by using ATP criteria: Female ≥ 88 cm, Male ≥ 102; FBS by ATP: Fasting blood glucose by using ATP criteria cut point: 110 mgdcl, 6.1 mmolL; Systolic or Diastolic BP ≥ 130/85; Triglycerides ≥ 150 mg/dL (1.7 mmol/L); HDL cholesterol < 40 mg/dL (1 mmol/L) in men and < 50 mg/dL (1.3 mmol/L) in women).
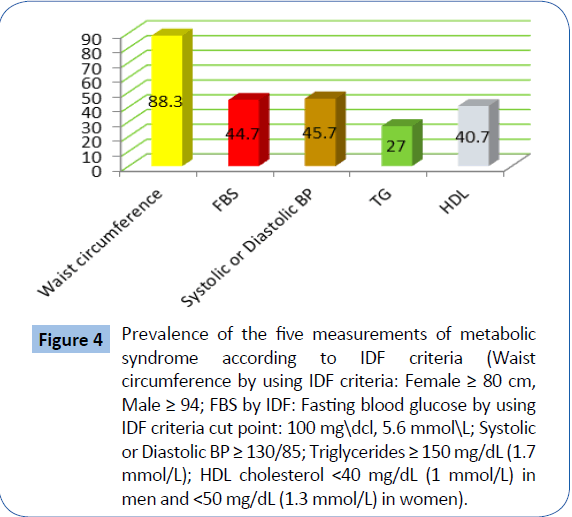
As Shown in Figure 4, waist circumference was above normal (80 cm for females and 94 cm for males) in 88.3% of the participant according to IDF criteria. Fasting blood glucose was above normal according to IDF criteria (5.6 mmol/L) in 44.7% of the participants. Systolic and/or diastolic blood pressure was above normal among 45.7% of the participants, triglycerides was above normal among 27% of the participants while HDL was less than normal among 40.7% of them.
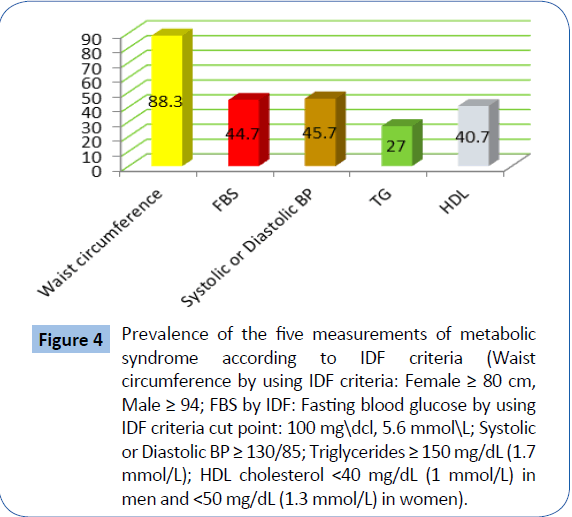
Figure 4: Prevalence of the five measurements of metabolic syndrome according to IDF criteria (Waist circumference by using IDF criteria: Female ≥ 80 cm, Male ≥ 94; FBS by IDF: Fasting blood glucose by using IDF criteria cut point: 100 mgdcl, 5.6 mmolL; Systolic or Diastolic BP ≥ 130/85; Triglycerides ≥ 150 mg/dL (1.7 mmol/L); HDL cholesterol < 40 mg/dL (1 mmol/L) in men and < 50 mg/dL (1.3 mmol/L) in women).
Factors associated with metabolic syndrome
1. According to ATP criteria: Table 8 shows that increase in age was a significant risk factor (OR=1.314, 95% CI=1.108-1.343, p=0.001), positive family history of DM was a significant risk factor (OR=10.6, 95% CI=1.419-14.084, p=0.001) and history of obesity was a significant risk factor for metabolic syndrome (OR=6.24, 95% CI=2.997-8.863, p=0.012). Gender was not significantly associated with metabolic syndrome.
| Variable |
Odds Ratio |
95% CI |
P value |
| Lower |
Upper |
| Age |
1.314 |
1.108 |
1.343 |
0.001 |
| Gender* |
1.21 |
0.79 |
2.27 |
0.27 |
| Family History of DM |
10.6 |
1.419 |
14.084 |
0.001 |
| Obesity |
6.24 |
2.297 |
8.863 |
0.012 |
| * Male is the reference category |
Table 8: Adjusted odds ratio for the factors associated with metabolic syndrome as per ATP.
2. According to IDF criteria: Table 9 shows that increase in age was a significant risk factor (OR=1.302, 95% CI=1.108-1.343, p=0.001) and positive family history of DM was a significant risk factor for metabolic syndrome (OR=10.92, 95% CI=1.463-14.427, p=0.001). Gender and obesity were not significantly associated with metabolic syndrome.
| Variable |
Odds Ratio |
95% CI |
P value |
| Lower |
Upper |
| Age |
1.302 |
1.108 |
1.343 |
0.001 |
| Gender* |
3.7 |
0.99 |
2.948 |
0.054 |
| Family History of DM |
10.92 |
1.463 |
14.427 |
0.001 |
| Obesity |
0.219 |
0.497 |
1.537 |
0.64 |
| * Male is the reference category |
Table 9: Adjusted odds ratio for the factors associated with metabolic syndrome as per IDF.
Discussion
This study estimates the prevalence of metabolic syndrome among peoples who attended primary care center in KFAFH in 2012 using the NCEP-ATPIII and IDF criteria.
Al-Nozha et al. found that the metabolic syndrome is highly prevalent in males and females in KSA [17]. The overall prevalence of metabolic syndrome in Saudi Arabia is affecting slightly more than one third of Saudi population. In the present study, the prevalence of metabolic syndrome among study population, based on ATP criteria was 41.3% while its prevalence was 54.3% based on IDF criteria. These alarming figures place a large proportion of the Saudi community at increased risk for the development of CAD, DM, and hypertension. In addition, this high prevalence could be attributed to the fact that there is no diabetic clinic or clinic of chronic diseases in primary care center and most of the patients with the chronic disease come every day in primary center in addition this center located beside the main hospital. The wide range of age observed in the present study could be attributed to the fact that most of our attendances to primary care in KFAFH are of old age.
The metabolic syndrome is consider a risk factor for incident CAD as has been shown by several studies [10,22-26]. In addition, researchers established association with other disorders including fatty liver disease, polycystic ovary syndrome, sleepdisordered breathing and chronic kidney disease [27-30].
In a study conducted to estimate the prevalence of metabolic syndrome among employees of Qassim University in Saudi Arabia using the NCEP-ATPIII criteria, a prevalence of (31.4%) reported [31].
Al-Qahtani et al. Found an age-adjusted prevalence of 20.8% among military personnel. Ford et aI. found an ageadjusted prevalence of 23.9% using the data from a nationally representative sample of American citizens derived from a crosssectional health survey [12]. Alexander et al. Found a prevalence of 43.5% among subjects older than 50 years from the data derived from the same survey as Ford et al. Japer et al. Found a prevalence of 23% among Arab Americans in their study in 2004 [32,33]. Meigs et al. Studied a large multi-ethnic cohort demographically representative of the US population and found an overall prevalence of the syndrome in 24% of the general population, with an inter-ethnic variation of 21-31% [34]. Villegas et al. found a prevalence of 20.7% among Irish middle-aged men and women [35]. Using the WHO definition of metabolic syndrome, Abdul-Rahim et al. Found a prevalence of 17% among the Palestinians in the West Bank. Al-Lawati et al. in their study of the prevalence of the syndrome among Omani adults found a prevalence of 21% [36,37].
Moreover, our data showed an increasing prevalence of the metabolic syndrome that is proportionate with increasing age that goes hand in hand with increasing prevalence of CAD among older populations. It is likely that the prevalence of metabolic syndrome will probably increase in the coming years due to the rapidly increasing prevalence of obesity among adults in Saudi Arabia, similar to data from the US that showed age-adjusted prevalence increased by 23.5% among females and 2.2% among males comparing data from 1994 and 2000 [38]. In Qassim, the prevalence of metabolic syndrome showed a steady increase with increasing age and BMI.
Given that the prevalence of overweight and obesity exceeds 70% in the KSA and that overweight and obese individuals are at a substantially higher risk of having metabolic syndrome, these results have important public health implications [39]. Strategies to combat the increasing prevalence of overweight and obesity that also target those with elevated risk factor pro?les, including sedentary habits and low cardio-respiratory fitness (CRF), are likely to be the most effective in improving the health of the population. The ?nding in the present study that the odds of metabolic syndrome increases among obese patients (OR=6.2) compared with normal weight categories supports results from NHANES III, in which the ORs for metabolic syndrome were 5.2 (95% CI 3.9 to 6.9) in overweight, 25.2 (19.3 to 32.9) in obese class I, and 67.7 (40.5 to 113.3) in obese class II and III participants, as compared with normal weight men [40]. In addition, in another study conducted in USA, the odds of metabolic syndrome increases across overweight (OR=4.7) and obese categories (OR=30.6) compared with normal weight categories. However, in the present sample, it is also noteworthy that almost half of obese patients did not have metabolic syndrome, whereas around one-third of normal weight subjects had metabolic syndrome. Thus, although there is a robust relationship between level of obesity and the presence of multiple risk factors, there is considerable variability in the presence of metabolic syndrome within BMI categories. The idea that some obese individuals appear healthy and display none of the traditional risk factors for chronic disease, including dyslipidemia and insulin resistance, has been reported previously [41-44].
Increased body weight plays the most important role. The observed prevalence of the metabolic syndrome in NHANESIII was 5% among the subjects of normal weight, 22% among the overweight, and 60% among the obese. Also a number of findings indicate that obesity (the cardinal feature of the metabolic syndrome) as an independent factor for causing renal dysfunction [45].
In a study conducted by Katzmarzyk et al. in USA, they indicated that the risk of CVD mortality was significantly higher in obese men, regardless of whether they had metabolic syndrome, than in normal weight men without metabolic syndrome while the higher risk of all-cause mortality in obese men was limited to those with metabolic syndrome (RR 1.55, 95% CI 1.14 to 2.11). In addition, there was a higher risk of CVD mortality in overweight men with metabolic syndrome (1.80, 1.10 to 2.97), but there was no higher risk of CVD mortality in healthy overweight men [41]. Although indirect, these results support the existence of “metabolically normal” obese individuals, which suggests that weight loss is of particular importance for overweight individuals with two or more CVD risk factors. In sum, the results indicate that weight loss should be promoted in all obese individuals, but should be more aggressively pursued among overweight and obese individuals accompanied by other risk factors [46].
Our study, though not representative of the population of Saudi Arabia, brings forth some striking results. It is obvious that prevalence of metabolic syndrome is alarmingly high among our study population. Equally alarming is the fact that the prevalence of risk factors for metabolic syndrome and its associated diseases (diabetes and obesity) is very high.
The components of the metabolic syndrome, such as central obesity and diabetes mellitus, are particularly common amongst the Saudi population, as shown by various other studies. It is projected that the prevalence of these diseases is rising at a faster rate in Saudi Arabia than in other parts of the world [47]. Therefore, it is vital to conduct nationwide research studies to obtain more specific and representative data. However, available evidence is strong enough to suggest that immediate intervention health program for metabolic syndrome must be developed to encourage healthier lifestyles, improve dietary habits, promote physical activity and exercise and discourage smoking among Saudi citizens.
Conclusion
This study has shown that almost 40 to 50% of the people attended KFAFH have metabolic syndrome and therefore they are at higher risk for both cardiovascular disease and diabetes mellitus. Metabolic syndrome was more prevalent among obese, diabetic and older patients. Similar studies are required among a wider range of subjects to assess the scope of the problem in Saudi Arabia.
Recommendations
1. Immediate interventional programs should be develop to encourage healthier lifestyles, improve dietary habits, promote physical activity and exercise and discourage smoking among Saudi citizens.
2. Physician at primary health care should be motivated to identify the problem and implement necessary remedial and preventive measures focusing on weight control, increased physical exercise, stopping smoking, controlling dyslipidemia, hypertension and diabetes.
3. General population should be educated to raise their consciousness toward the value of screening. Control of this syndrome among population is of vital importance and requires the attention of all health professionals.
4. Conduction of a nationwide research studies to obtain more specific and representative data about metabolic syndrome.
Ethical Considerations
1. Written permission from Joint Program of Family and Community Medicine obtained before conduction of the research.
2. Ethical approval from the local Ethical committee.
3. Written individual consent taken before entering in the study and the patient knew the result of hisher investigation and measurements.
4. If the patient diagnosed or at risk of having metabolic syndrome, heshe received health education, advice on life style modification andor medication.
5. All information kept confidential and not be accessed except for the purpose of scientific research.
Utilization
The result of the study can play a role in developing preventive measure of diabetes, hypertension, obesity, dyslipidemia in addition to CVD.
22651
References
- Kylin E (1923) Studies on hypertension hyperglycaemia hyperuric syndrome. Zentralbl Inn Med 44: 105-127.
- Vague J (1947) Sex differentiation, determinant factor of forms of obesity. Obes Res 53: 339-340.
- Avogaro P, Crepaldi G (1965) Essential hyperlipidemia, obesity and diabetes. Diabetologia 1: 137.
- Reaven GM (1988) Banting Lecture 1988. Role of insulin resistance in human disease. Diabetes 37: 1595-1607.
- Kaplan NM (1989) The deadly quartet. Upper-body obesity, glucose intolerance, hypertriglyceridemia, and hypertension. Arch Intern Med 149: 1514-1520.
- Haffner SM, Valdez RA, Hazuda HP, Mitchell BD, Morales PA, et al. (1992) Prospective analysis of the insulin-resistance syndrome (syndrome). Diabetes 41: 715-722.
- Alberti G (2009) Harmonizing the metabolic syndrome. Circulation 120: 1640-1645.
- National Cholesterol Education Program (NCEP) (2002) Third Report of the National Cholesterol Education Program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 106: 3143-3421.
- Mabry RM, Reeves MM, Eakin EG, Owen N (2010) Gender differences in prevalence of the metabolic syndrome in gulf cooperation council countries: A systematic review. Diabet Med 27: 593-597.
- Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, et al. (2001) Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24: 683-689.
- Grundy SM, Brewer HB, Cleeman JI, Smith SC Jr, Lenfant C, et al. (2004) Definition of metabolic syndrome, report of the national heart, lung, and blood institute/american heart association conference on scientific issues related to definition. Circulation 109: 433-438.
- Ford ES, Giles WH, Dietz WH (2002) Prevalence of the metabolic syndrome among US adults: Findings from the third national health and nutrition examination survey. JAMA. 287: 356-359.
- Sidorenkov O, Nilssen O, Brenn T, Martiushov S, Arkhipovsky VL, et al. (2010) Prevalence of the metabolic syndrome and its components in northwest Russia: The Arkhangelsk study. BMC Public Health 10: 23.
- Martinez MA, Puig JG, Mora M, Aragon R, O'Dogherty P, et al. (2009) Metabolic syndrome: Prevalence, associated factors, and C-reactive protein: The MADRIC (MADrid RIesgo cardiovascular) study. Metabolism 57: 1232-1240.
- Li JB, Wang X, Zhang JX, Gu P, Zhang X, et al. (2010) Metabolic syndrome: Prevalence and risk factors in southern china. J Int Med Res 38: 1142-1148.
- Mohamud WN, Ismail AA, Sharifuddin A, Ismail IS, Musa KI, et al. (2011) Prevalence of metabolic syndrome and its risk factors in adult malaysians: Results of a nationwide survey. Diabetes Res Clin Pract 91: 239-245.
- Al-Nozha M, Al-Khadra A, Arafah MR, Al-Maatouq MA, Khalil MZ, et al. (2005) Metabolic syndrome in Saudi Arabia. Saudi Med J 26: 1918-1925.
- Al-Daghri NM, Al-Attas OS, Alkharfy KM, Sabico SL, Chrousos GP, et al. (2010) Decreasing prevalence of the full metabolic syndrome but a persistently high prevalence of dyslipidemia among adult Arabs. PLoS One 5: e12159.
- Al-Qahtani DA, Imtiaz ML (2005) Prevalence of metabolic syndrome in Saudi adult soldiers. Saudi Med J 26: 1360-1366.
- Al-Qahtani DA, Imtiaz ML, Saad OS, Hussein NM (2006) A comparison of the prevalence of metabolic syndrome in Saudi adult females using two definitions. Metab Syndr Relat Disord 4: 204-214.
- Wang J, Thornton JC, Bari S, Willia MSB, Gallagher D, et al. (2003) Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutr 77: 379-384.
- Girman CJ, Rhodes T, Mercuri M, Pyorala K, Kjekshus J, et al. (2004) 4S group and the AFCAPS/Tex CAPS research group: The metabolic syndrome and risk of major coronary events in the scandinavian simvastatin survival study (4s) and the air force/texas coronary atherosclerosis prevention study (AFCAPS/Tex CAPS). Am J Cardiol 93: 136-141.
- Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, et al. (2002) The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 288: 2709-2716.
- Klein BE, Klein R, Lee KE (2002) Components of the metabolic syndrome and risk of cardiovascular disease and diabetes in beaver dam. Diabetes Care 25: 1790.
- Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, et al. (2003) Carotid atherosclerosis and coronary heart disease in the metabolic syndrome: Prospective data from the bruneck study. Diabetes Care 26: 1251.
- Kip KE, Marroquin OC, Kelley DE, Johnson BD, Kelsey SF, et al. (2004) Clinical importance of obesity versus the metabolic syndrome in cardiovascular risk in women: A report from the women's ischemia syndrome evaluation (WISE) study. Circulation 109: 706.
- Marceau P, Biron S, Hould FS, Marceau S, Simard S, et al. (1999) Liver pathology and the metabolic syndrome X in severe obesity. J Clin Endocrinol Metab 84: 1513.
- Pasquali R, Gambineri A, Anconetani B, Vicennati V,Colitta D, Caramelli E, et al. (1999) The natural history of the metabolic syndrome in young women with the polycystic ovary syndrome and the effect of long-term oestrogen-progestagen treatment. Clin Endocrinol (Oxf) 50: 517.
- Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, et al. (2002) Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med 165: 670.
- Vgontzas AN, Papanicolaou DA, Bixler EO, Hopper K, Lotsikas A, et al. (2000) Sleep apnea and daytime sleepiness and fatigue: Relation to visceral obesity, insulin resistance and hypercytokinemia. J Clin Endocrinol Metab 85: 1151-1158.
- Barrimah IE, Mohaimeed AR, Midhat F, Al-Shobili HA (2009) Prevalence of metabolic syndrome among qassim university personnel in Saudi Arabia. International J Health Sci 3: 133-142.
- Alexander CM, Landsman PB, Teutsch SM, Haffner SM (2003) NCEP defined metabolic syndrome, diabetes mellitus and prevalence of coronary heart disease among NHANES III participants aged 50 years and older. Diabetes 52: 1210-1214.
- Jaber LA, Brown MB, Hammad A, Zhu Q, Herman WH (2004) The prevalence of the metabolic syndrome among arab americans. Diabetes Care 27: 234-238.
- Meigs JB, Wilson PWF, Nathan DM, Agostino RB, Haffner SM, et al. (2003) Prevalence and characteristics of the metabolic syndrome in san antonio heart and framingham offspring studies. Diabetes 52: 2160-2167.
- Villegas R, Perry IJ, Creagh D, Hinchion R, O’Halloran D (2003) Prevalence of metabolic syndrome in middle-aged men and women. Diabetes Care 26: 3198-3199.
- Abdul-Rahim HF, Husseini A, Bjertness E, Giacaman R, Gordon NH, et al. (2001) The metabolic syndrome in the west bank population. An urban-rural comparison. Diabetes Care 24: 275-279.
- Al-Lawati JA, Mohammad AJ, Al-Hinal HQ, Jousilahti P (2003) Prevalence of the metabolic syndrome among Omani adults. Diabetes Care 26: 1781-1785.
- Ford ES, Giles WH, Mokdad AH (2004) Increasing prevalence of the metabolic syndrome among US adults. Diabetes Care 27: 2444-2449.
- Al-Nozha MM, Al-Mazrou YY, Al-Maatouq MA, Arafah MR, Khalil MZ, et al. (2005) Obesity in Saudi Arabia. Saudi Med J 26: 824-829.
- Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, et al. (2003) The Metabolic syndrome: Prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med 163: 427-436.
- Katzmarzyk PT, Tchurch TS, Janssen J, Ross R, Blair SN (2005) Metabolic syndrome, obesity, and mortality. Diabetes Care 28: 391-397.
- Brodoff DN, Bleicher SJ (1982) Characterization of the syndromes of obesity. In diabetes mellitus and obesity. Metabolic syndrome: 219-226.
- Sims EA (2001) Are there persons who are obese, but metabolically healthy? Metabolism 50: 1499-1504.
- Karelis AD, St-Pierre DH, Conus F, Lhoret RR, Poehlman ET (2004) Metabolic and body composition factors in subgroups of obesity: What do we know? J Clin Endocrinol Metab 89: 2569-2575.
- Elsaid SA, Hamada MA, Alsaran KA (2009) Obesity and metabolic syndrome in Saudi hemodialysis patients. JNRT 2: 18-27.
- National Institutes of Health (2000) The practical guide to the identification, evaluation and treatment of overweight and obesity in adults. Bethesda, US.
- King H, Aubert RE, Herman WH (1998) Global burden of diabetes 1995-2025: Prevalence, numerical estimates and projections. Diabetes Care 21: 1414-1431.