Totir M1,2, Voinea LM1,2, Ciuluvica R1, Istrate S1,2*, Vrapciu AD1,2, Schmizer S1, Balta F1 and
Costache M1,3
1Carol Davila, University of Medicine and Pharmacy, 8, Eroii Sanitari BLVD, District 5, 050474, Bucharest, Romania
2Ophthalmology Clinic, University Emergency Hospital, 169 Splaiul Independentei BLVD, District 5, 050098, Bucharest, Romania
3Department of Pathology, University Emergency Hospital, 169 Splaiul Independentei BLVD, District 5, 050098, Bucharest, Romania
- *Corresponding Author:
- Sinziana Luminita Istrate
Carol Davila, University of Medicine and Pharmacy, 8
Eroii Sanitari BLVD, District 5, 050474,Bucharest, Romania
Tel: 0040726535515
E-mail: sanzinici@yahoo.com
Received date: September 11, 2018; Accepted date: October 05, 2018; Published date: October 09, 2018
Citation: Totir M, Voinea LM, Ciuluvica R, Istrate S, Vrapciu AD, et al. (2018) Carol Davila, University of Medicine and Pharmacy, 8, Eroii Sanitari BLVD, District 5, 050474, Bucharest, Romania. Arch Med Vol No:10 Iss No:5:6
Copyright: © 2018 Totir M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords:
Tumor of the follicular infundibulum; Basal cell carcinoma; Eyelid tumor
Abbreviations
BCC: Basal Cell Carcinoma; TFI: Tumor of Follicular Infundibulum; HE: Hematoxylin–Eosin, PAS: Periodic Acid Schiff
Introduction
Periocular region can be the site for different types of benign and malignant tumors developing from epidermis, dermis or annexes. Although histological analysis is mandatory and gold standard for final diagnosis, clinical diagnosis is also important in order to ensure proper treatment, to establish the necessity of a wide or narrow peritumoral tissue excision depending the clinical tumor characteristics and to appreciate the prognosis [1].
Tumor of the follicular infundibulum (TFI) is a rare, benign adnexal tumor with characteristic histopathological features [2-4]. The original report about the tumor of the follicular infundibulum was published by Mehregan and Butler [3].
The most frequent form is usually a solitary, smooth or slightly keratotic papule or nodule usually on head and neck, frequently clinically misdiagnosed as a basal cell carcinoma but the histopathological analysis reveals characteristic aspects for TFI. [4] Histological features are plate like growth of epithelial cells situated in the superficial dermis, extending parallel to the epidermis; the peripheral cell layer of the tumor plate shows palisading while the central cells show a pale staining cytoplasm as a result of their glycogen content [5,6]. According to Alomari et al. TFI has a unique staining pattern with a brushlike network of elastin fibers and no staining for Ber-EP4 in contrast to basal cell carcinoma [7].
Case
A 50-years-old woman presented with a 3 month history of an asymptomatic, elevated slow growing lesion in the medial part of the right inferior eyelid. She is a non-smoker, lives in rural area and stated chronic solar exposure. Medical history was significant for recent diagnosis of open angle glaucoma, RE cataract and virus B hepatitis.
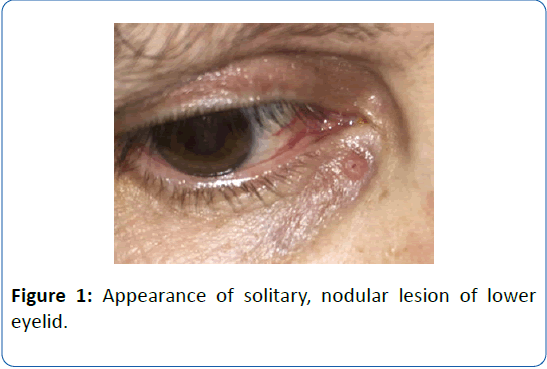
On examination, a 4 mm solitary, round, nodular, slightly elevated lesion with presence of telangiectasia, located in the medial part of the right inferior eyelid, not involving the eyelid margin, 5 mm below the inferior lacrimal punctum (Figure 1). No lymph nodes were detected at the clinical examination. Based on the clinical examination we could not decide between benign eyelid tumor and eyelid BCC.
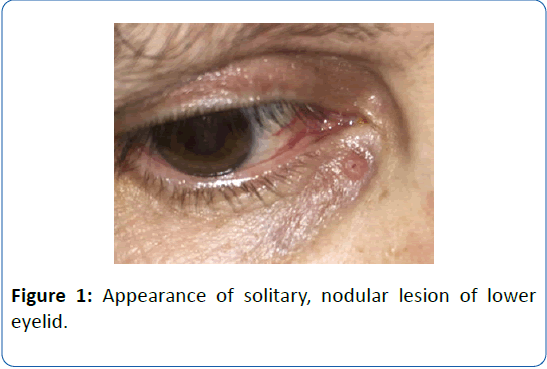
Figure 1: Appearance of solitary, nodular lesion of lower eyelid.
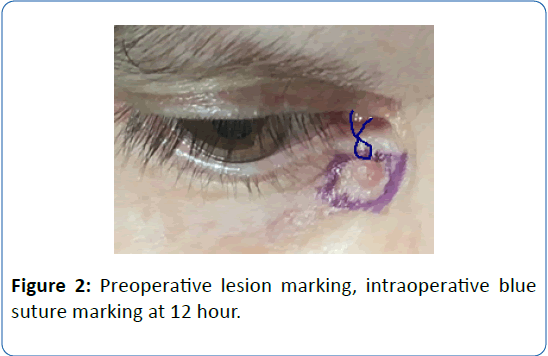
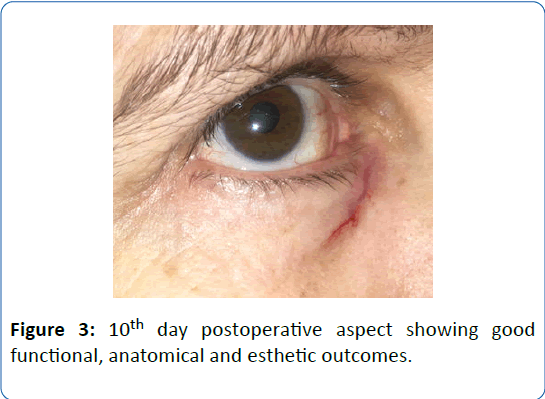
The patient underwent surgical excision of the tumor with two millimeters of healthy-appearing tissue excision that was enough to achieve tumor free-margins. Intraoperatively, we marked the excised piece at 12 o’clock position with blue suture in order for the pathologist to correctly orientate the specimen (Figure 2). Direct eyelid closure reconstruction was performed with good functional, anatomical and esthetic outcomes (Figure 3).
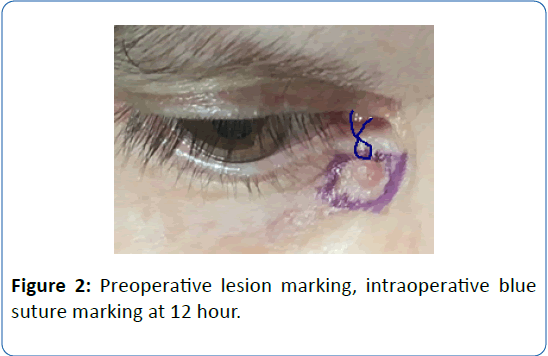
Figure 2: Preoperative lesion marking, intraoperative blue suture marking at 12 hour.
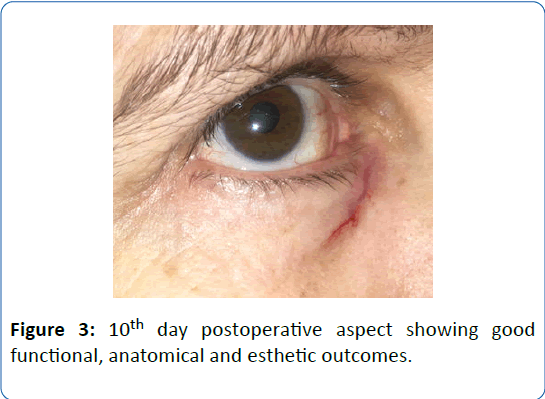
Figure 3: 10th day postoperative aspect showing good functional, anatomical and esthetic outcomes.
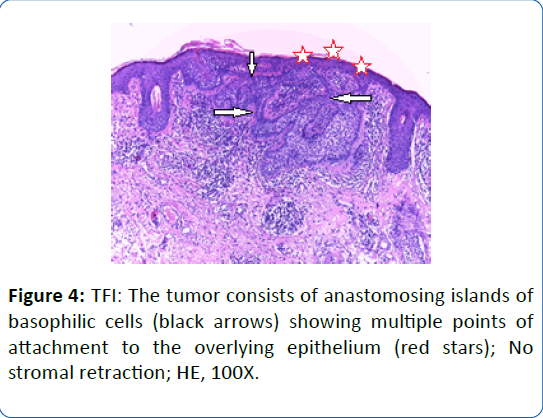
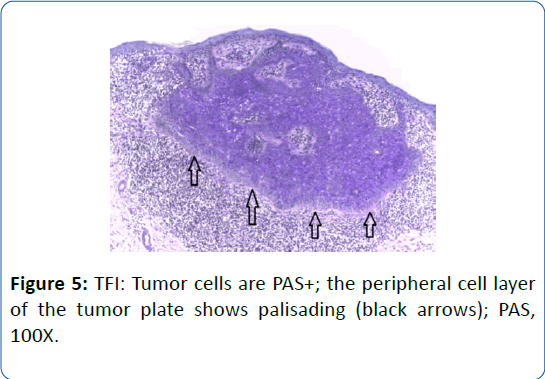
The specimen sample was fixated with 10% buffered formalin and was processed by conventional histopathological methods using paraffin embedding, sectioning at 3 μm and Hematoxylin–Eosin (HE) staining. Histopathological examination of standard-stained Hematoxylin-Eosin (HE) slides revealed in the middle of surgical excision piece a plate like growth of epithelial cells in the upper dermis extending parallel to the epidermis and showing multiple connections with the lower margin of the epidermis (Figure 4). The peripheral cell layer of the tumor plate shows palisading (Figure 5) and the centrally located cells show a pale-staining cytoplasm as a result of their glycogen content; small areas resembling the follicular infundibulum are seen (Figure 6); cytologic atypia, necrosis and mitotic activity are absent; there are not areas of retraction of the stroma from tumor.
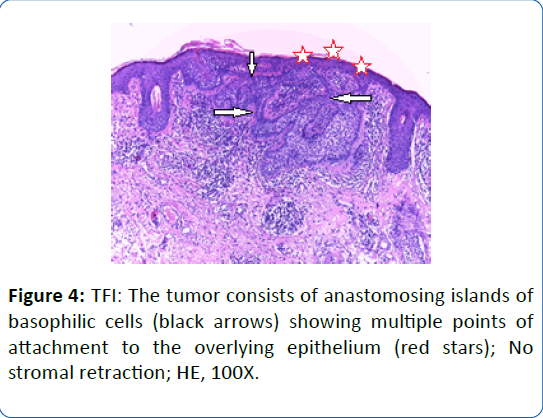
Figure 4: TFI: The tumor consists of anastomosing islands of basophilic cells (black arrows) showing multiple points of attachment to the overlying epithelium (red stars); No stromal retraction; HE, 100X.
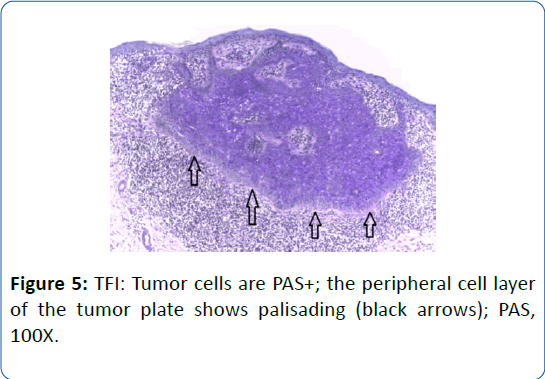
Figure 5: TFI: Tumor cells are PAS+; the peripheral cell layer of the tumor plate shows palisading (black arrows); PAS, 100X.

Figure 6: TFI: small area resembling the follicular infundibulum is seen (black arrow) surrounded by palestaining cytoplasm cells (red stars); Cytologic atypia, necrosis and mitotic activity are absent; HE 200X.
Immunohistochemical tests were performed. The paraffin blocks were cut and the resulting 3 μm thick sections were mounted on slides covered with poly-L-Lysine. Afterwards, the sections were deparaffinized in successive toluene and alcohol baths, rehydrated (three successive alcohol baths with decreasing concentration: 96%, 80% and 70%) followed by a final bath with distillate water for 10 minutes. For immunohistochemical staining, we used an indirect tristadial Avidin–Biotin complex method (deparaffination in toluene and alcohol series), rehydration, washing in PBS (phosphate buffered saline), incubation with normal serum, for 20 minutes, incubation with primary antibody overnight, DAKO LSAB kit, washing in carbonate buffer and development in 3,3’- diaminobenzidine (DAB) hydrochloride/hydrogen peroxide nuclear counterstaining with Mayer’s Hematoxylin.
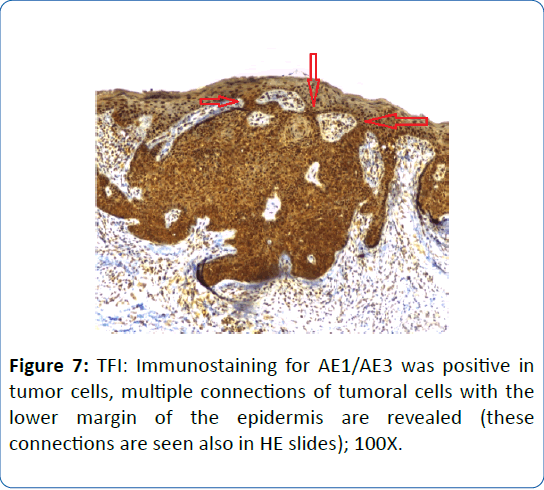
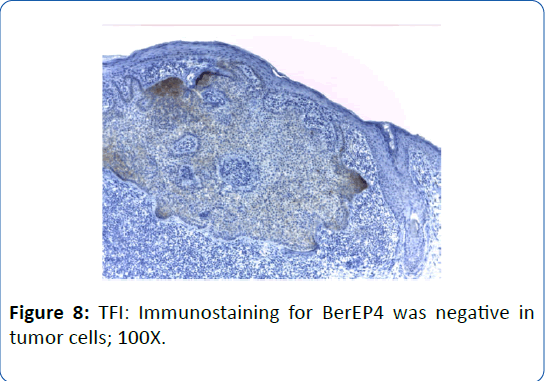
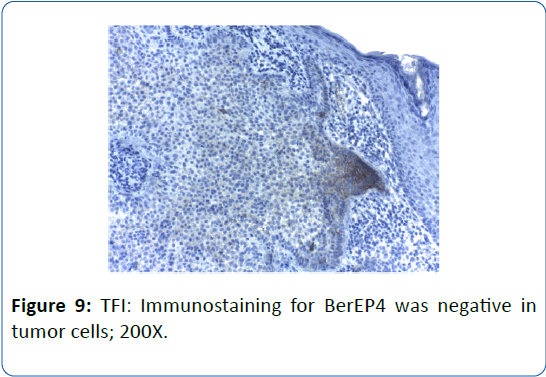
We used the following antibodies from Biocare: AE1/AE3 (mouse monoclonal, clone AE1/AE3, dilution 1:100) and BerEP4 (mouse monoclonal, clone Ber-EP4, dilution 1:100). The immunohistochemical staining found that the tumoral cells have a positive expression for AE1/AE3, but are negative for BerEP4 (Figures 7-9). Conventional histopathology and immunohistochemical tests that were performed revealed specific tumor characteristics that established as final diagnosis tumor of follicular infundibulum of the right inferior eyelid.
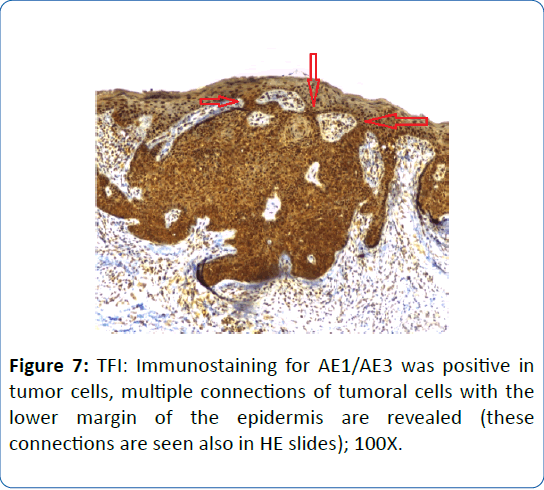
Figure 7: TFI: Immunostaining for AE1/AE3 was positive in tumor cells, multiple connections of tumoral cells with the lower margin of the epidermis are revealed (these connections are seen also in HE slides); 100X.
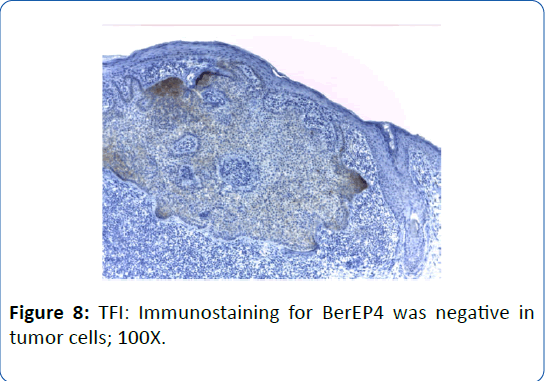
Figure 8: TFI: Immunostaining for BerEP4 was negative in tumor cells; 100X.
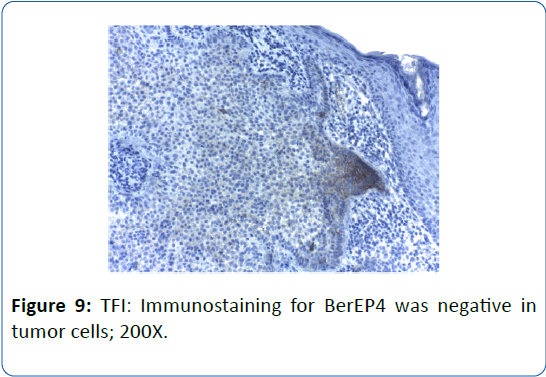
Figure 9: TFI: Immunostaining for BerEP4 was negative in tumor cells; 200X.
Discussion
BCC and TFI can be confused both clinically and histologically. Differential diagnosis for TFI can be made based on clinical appearance with BCC, nevi, actinic keratosis, trichoepithelioma, inverted follicular keratosis, seborrheic keratosis, warts [7-10] and based on histopathological aspect with BCC, trichilemmoma, clear cell seborrheic keratosis [9-11].
In the literature, eyelid tumors epidemiology studies found in variable percentages that benign tumors (like cysts, seborrheic keratosis, nevi, papilloma, chalazia) are more frequent then malignant tumors (BCC, squamous cell carcinoma, sebaceous gland carcinoma and malignant melanoma) [12,13]. BCC is the most frequent eyelid malignancy representing about 90% of the eyelid tumors [14]. TFI is a rare epithelial tumor with a nonspecific clinical presentation [4]. The lesion tends to be asymptomatic or rarely to associate pruritus after sun exposure [7,8].
Irregular borders, pearly lesions, ulceration, lesion that does not heal, telangiectasias are signs that suggest a malignancy but appearance can be variable and can lead to clinical confusion between benign and malignant lesions. Lesions in the periocular region are particular because of the eyelid skin characteristics, risk of malignant tumors to invade orbit, esthetic implications that can be dramatic in case of large and invading tumor, also that surgical treatment should preserve healthy peritumoral tissue in order to maintain a normal eyelid function and a healthy ocular surface for a good visual outcome [1].
A comparison between the histological characteristics of TFI and BCC (Table 1). Immunohistochemistry for BCC typically demonstrates positive expression of Ber-EP4 and AE1/AE3 while for TFI expression of Ber-EP4 is negative and for AE1/AE3 is positive. The accuracy of the clinical diagnosis of eyelid malignancies is variable in published studies ranging from 65% to 96% [1]. In our case, the presumed diagnosis of benign or malignant eyelid tumor based on clinical aspect was difficult. We decided for tumor surgical excision with 2 mm predetermined margins (taking into account the possibility to perform reexcision) and histopathological, immunohistochemical analysis and tumor margins control.
| |
TFI |
BCC |
| Features of peripheral palisading |
(Yes) No stromal retraction |
(Yes) With stromal retraction |
| Attachment to the overlying epidermis |
(Yes) |
(Yes) |
| Cytologic atypia and mitoses |
- |
(Yes) |
| Increased glycogen and PAS+ stain |
(Yes) |
- |
Table 1: Histological characteristics of TFI and BCC [5,9].
We tried to preserve healthy clinical peritumoral tissue and prevent unnecessary extensive excision given the fact that the lesion affected the medial part of the lower eyelid, inferior to the inferior lacrimal punctum and the patient was young without significant skin laxity.
In our case, final diagnosis was based on histopathological and immunohistochemical aspect and indicated a benign tumor (tumor of the follicular infundibulum) which was safely and completely excised with a narrow margin of clearance (that made possible the eyelid reconstruction by direct closure), reexcision was not necessary and direct eyelid reconstruction provided a good, rapid functional and esthetic outcome. Our case report respects the characteristics of the TFI reported by Alomari et al. females have slight prevalence, usually a solitary lesion, located on face and scalp, except the age that was over 60 years old and in our case is 50 years old [7].
In the literature, TFI diagnosis is based on histologic findings and treatment is by surgical excision (which can also provide the histopathological specimen that is analyzed and provides a final, definitive diagnosis), cryotherapy and topical keratolitics [5,9].
Prognosis is excellent, TFI has no malignant potential but it worth mentioning that it may be present in patients with Cowden’s syndrome [4,5]. Weyers et al. consider that TFI is encountered commonly in association with basal cell carcinoma, often as an incidental finding and consider that TFI may be one of many manifestations of BCC rather than a differential diagnosis of it [11]. These facts can lead to the conclusion that we need to have a periodical follow-up for patients with diagnosed TFI.
Conclusions
TFI is a rare benign adnexal tumor that is often clinically not suspected but has characteristic histopathological features and unique staining aspect, like peripheral palisading and pale cells, also positive expression of AE1/AE3 and negative expression of Ber-EP4 [1,4].
TFI has a non-specific appearance and may be clinically misdiagnosed with other tumors, especially BCC which can lead to unnecessarily extensive surgery that may not be recommended for benign tumors especially in the periocular region where the need for preserving healthy peritumoral tissue is very important [9].
The accuracy of the clinical diagnosis of eyelid malignancies is variable; pathologists have the definitive role in tumor diagnosis and provide an accurate, final diagnosis.
Acknowledgements
Financial support of project no: PN16200401/2016 (National Core Programme) and contract no. 114/2014 ORBIMPLANT (PN-II-PT-PCCA-2013-4) is gratefully acknowledged. The authors declare that there is no conflict of interest regarding the publication of this paper. All authors of the paper have equal contribution to this publication.
23433
References
- Rossato LA, Carneiro RC, Miyazaki A, Matayoshi S (2014) Accuracy of clinical examination in the diagnosis of eyelid lesions. Rev Bras Oftalmol 73: 324-328.
- Lee DW, Yang JH, Lee HM, Won CH, Chang S, et al. (2011) A case of tumor of the follicular infundibulum with sebaceous differentiation. Ann Dermatol 23: 198-200.
- Mehregan AH, Butler JD (1961) A tumor of follicular infundibulum. Report of a case. Arch Dermatol 83: 924-927.
- Haddad N, de Oliveira Filho J, Reis MJL, Michalany AO, da Rosa Nasser K, et al. (2014) Tumor of follicular infundibulum with unique features. An Bras Dermatol 89: 964-966.
- El-Darouti MA (2013) Clinically non-specific, histologically very specific tumor, challenging cases in dermatology, Springer, London, UK.
- Abbas O, Mahalingam M (2009) Tumor of the follicular infundibulum: An epidermal reaction pattern? Am J Dermatopathol 31: 626-633.
- Alomari A, Subtil A, Owen CE, McNiff JM (2013) Solitary and multiple tumors of follicular infundibulum: A review of 168 cases with emphasis on staining patterns and clinical variants. J Cutan Pathol 40: 532-527.
- Kolenik SA, Bolognia JL, Castiglione FM Jr, Longley BJ (1996) Multiple tumors of the follicular infundibulum. Int J Dermatol 35: 282-284.
- Kubba A, Batrani M, Taneja A, Jain V (2014) Tumor of follicular infundibulum: an unsuspected cause of macular hypopigmentation. Indian J Dermatol Venereol Leprol 80: 141-144.
- Hutchinson KW, Boulton JE, Sullivan TJ, Whitehead KJ (2001) Periocular tumour of the follicular infundibulum. Clin Exp Ophthalmol 29: 100-101.
- Weyers W, HÃÂÃÂÃÂâÂÂÃÂâ â≢ÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂörster S, Diaz-Cascajo C (2009) Tumor of follicular infundibulum is Basal cell carcinoma. Am J Dermatopathol 31: 634-641.
- Asproudis I, Sotiropoulos G, Gartzios C, Raggos V, Papoudou-Bai A, et al. (2015) Eyelid tumors at the university eye clinic of IOANNINA, Greece: A 30-year retrospective study. Middle East Afr J Ophthalmol 22: 230-232.
- Savannah EBaril, Suzanne KFreitag (2012) Incidence of benign and malignant eyelid tumors at the massachusetts eye and ear infirmary over one year. Invest Ophthalmol Vis Sci 53: 1448.
- Saleh GM, Desai P, Collin JR, Ives A, Jones T, et al. (2017) Incidence of eyelid basal cell carcinoma in England: 2000ÃÂÃÂÃÂâÂÂÃÂâÂÂÃÂâÃÂÃÂââ¬Ã
¡ÃÂâââ¬Ã
¡ÃÂìÃÂÃÂââ¬Ã
¡ÃÂâââÂÂìÃÂ
âÂÂ2010. Br J Ophthalmol 101: 209-212.